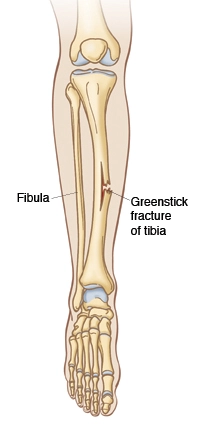
Greenstick Fracture
What is a Greenstick Fracture?
Greenstick fracture, also known as an incomplete fracture, is a type of broken bone commonly seen in children. It occurs when the bone bends and cracks, but doesn’t completely break. This type of fracture is typically seen in the long bones of the body, such as the forearm. The name “greenstick” is derived from the idea that the bone behaves in a similar way to a green stick, which bends and cracks but does not completely break.
Because children’s bones are more flexible than those of adults, they are more likely to experience greenstick fractures. The condition is often a result of falls or other forms of trauma, as the bones are still in the developmental stage and more pliable. Although greenstick fractures can be painful, they usually heal relatively quickly, as the bones have a greater capacity to remodel and repair themselves at a young age. However, proper medical attention and care are crucial to ensure proper healing and prevent any complications. Treatment options may include casting or splinting to immobilize the affected area and allow the bone to heal correctly.
Greenstick fractures happen to kids younger than ten. The age range of 5 to 14 years old is the most often impacted, with a 1 in 100 occurrence. Adults typically experience it. On one side of the bone, only the cortex and periosteum are injured by a partial thickness fracture, whereas the other side of the bone is unaffected. occurs most frequently in long bones such as the humerus, femur, tibia, and radius. After the first two weeks, green stick fractures continue to shift because they are unstable.
Understanding the unique characteristics and management of greenstick fractures is important for healthcare professionals and caregivers dealing with pediatric injuries. Early diagnosis and appropriate treatment are essential for ensuring proper healing and minimizing any potential long-term effects on the child’s growth and development.
Types of greenstick fractures
Longer bones, such as yours, are typically affected by greenstick fractures.
- Humerus (upper arm bone).
- Radius and ulna (forearm bones).
- Phalanges (finger and toe bones).
- Femur (thigh bone).
- Fibula (calf bone).
How common are they?
Greenstick fractures are quite prevalent, particularly in young patients. In the United States, millions of children suffer from greenstick fractures each year.
Pathophysiology
A greenstick fracture is a partial thickness fracture in which the periosteum and cortex are the only areas of the bone that are disrupted on one side while the other side of the bone is left intact. They are particularly common in long bones, such as the clavicle, ulna, fibula, tibia, and radius. Most often, they affect the ulna, radius, or humerus and occur in the forearm and arm. This is due to the fact that individuals often brace falls by extending their arms, which can cause upper extremity fractures.
Though far less often than long bones, greenstick fractures can also happen in the face, chest, scapula, and almost any other bone in the body. Greenstick fractures, for instance, can happen to the nose and jaw. Up to 55% of pediatric mandibular fractures are condylar fractures, making them the most prevalent type of fracture. Condylar fractures come in three different forms. The most frequent types of fractures are incomplete greenstick fractures or low subcondylar fractures.
Because most of the nasal bones’ cartilage is composed of cartilage, nasal trauma is the most prevalent cause of greenstick fractures in children. This is because the nasal sutures are not cemented together.
Signs and symptoms
Greenstick fractures typically trigger pain in the location that was injured, and some of its clinical characteristics are comparable to those of a typical long bone fracture. Because these fractures are unique to children, a younger child may groan uncontrollably while an older child will shield the damaged area. The region may be bruised, red, and swollen, much as with a typical fracture.
Greenstick fractures typically result in a bend to the wounded area rather than a clear deformity, which is troublesome since they are stable fractures because part of the bone remains whole and unbroken. Pain in the region is one of the symptoms, which may arise from improper use of that particular bone. This may be pain from a single injury or a very slow-moving chronic condition.
How is a greenstick fracture diagnosed?
See a physician if you’re having any of the aforementioned symptoms:
- You have constant pain in a limb that lasts for a day or two.
- Your leg has a noticeable bend in it.
- Nothing can be weighted on your leg.
- Your doctor will examine you physically during your visit to check for any deformities, edema, pain, or numbness. Your doctor may ask you to twitch your fingers or do other similar procedures to look for the nerve damage that can occasionally accompany bone fractures. They could also examine the joints above and below the damaged location. They can advise getting an X-ray to be sure you have a greenstick fracture.
Treatment / Management
A closed reduction and immobilization must be carried out by the medical professional if the degree of angulation is considerable. Immobilization is necessary for all greenstick fractures, and casting a few days following the original injury reduces the chance that growing edema following the fracture will necessitate a recast. It is normally advised to suggest a kid for orthodontic care during the first appointment, however, this will depend on the child’s age and degree of angulation.
Long bone greenstick fractures should be immobilized in a cast for around six weeks. The location of the fracture determines the kind of cast to be used. While proximal fractures require long arm casting and may be converted to a short arm cast halfway through the healing phase, at around three weeks, distal fractures can be placed in short arm casts. Patients need closer orthopedic follow-up if they have proximal fractures. However, because greenstick fractures are more likely to refracture and cause displacement than buckle or plastic bending injuries, and because they are unstable, all of them should have some kind of orthopedic follow-up.
Splinting is an option for treating greenstick fractures, however, it is less frequent. It works best when there is little angulation and attentive patient or family follow-up. Splinting might be less expensive and enable the splint to be taken off for showers.
Differential Diagnosis
Among these are Salter-Harris fractures, torus fractures, spiral fractures, non-accidental fractures, open fractures, pathologic fractures, non-displaced fractures, and plastic deformities (non-displaced spiral fractures of the distal tibia).
Prognosis
The majority of greenstick fractures mend successfully without causing noticeable or functional alterations to the fractured bone, hence the prognosis is generally favorable. However, there is a chance of refracture, total fracture, and fracture displacement if the patient is not immobilized appropriately and receives inadequate orthopedic follow-up.
Complications
Because greenstick fractures are unstable and require prompt immobilization, there is a significant risk of refracture. Recurrent forearm fractures can occur often after an original greenstick fracture. One case series states that further radiographic examination of the proximal and distal segments of the radius is necessary to confirm that their rotational positions match one another following the reduction of the radius greenstick fracture. This is known as the radius crossover sign, and it may lessen the possibility of forearm deformity and loss of mobility. In one case report, scapular winging was discovered during a physical examination due to a greenstick scapula fracture.
The following are the most typical side effects of greenstick fracture surgery:
- Malunion: This is the misalignment of a damaged bone during the healing process.
- Nonunion: The partial or complete regrowth of a bone.
- Acute compartment syndrome (ACS): When blood flow to the muscle is impeded, irreparable injury to the muscles and nerves may result.
How can greenstick fractures be prevented from happening?
Greenstick fractures could be unavoidable, particularly if your youngster is traumatized by a fall or similar incident. However, you may lower the chance of damage in your family in a few ways:
- Wear your seatbelt at all times.
- Ensure that everyone is wearing the appropriate safety gear for all sports and activities.
- Make sure there is nothing in your house that may trip someone up.
- When reaching for anything at home, always use the appropriate tools or equipment. Children should never be allowed to stand on counters, chairs, or tables.
Overview
The best way to address greenstick fractures, which are most common in children, is to form an interprofessional team with the pediatrician, emergency department doctor, orthopedic nurse, and orthopedic surgeon. A closed reduction and immobilization must be carried out by the medical professional if the degree of angulation is considerable. Immobilization is necessary for all greenstick fractures, and casting a few days following the original injury reduces the chance that growing edema following the fracture will necessitate a recast. It is normally advised to suggest a kid for orthodontic care during the first appointment, however, this will depend on the child’s age and degree of angulation.
The majority of children have positive outcomes. To make sure that healing is taking place properly, though, follow-up is necessary.
FAQs
What is the difference between a fracture and a greenstick fracture?
Whole fracture: In this type of fracture, the bone has been broken into individual pieces entirely. Greenstick fracture: More prevalent in youngsters, this incomplete fracture causes the bone to be partially bent or shattered.
What is another name for a greenstick fracture?
A greenstick fracture happens when a bone fractures, not shatters into two pieces. This term comes from the fact that it resembles what occurs when you attempt to tear off a “green” limb from a tree. “Partial fracture” is another term for this fracture.
Why is it called greenstick fracture?
A Greenstick Fracture: What Is It? One kind of fractured bone is a greenstick fracture. A fracture occurs just on one side of the bone, not across the entire structure. Because it might resemble a branch that has broken and split on one side, it is known as a “greenstick” fracture.
What is an example of a greenstick fracture?
A greenstick fracture is a fracture when the bone cracks and bends rather than shattering into individual pieces. The fracture has an appearance akin to what occurs when a tiny, “green” tree limb is broken. The majority of greenstick fractures happen to kids under the age of ten.
How is a greenstick fracture treated?
Greenstick fracture treatments: what are they? The majority of greenstick fractures are treated by providers using a cast to immobilize the bone and prevent it from moving. Your youngster may likely require a cast for around six weeks. Subsequent X-rays will be required to ensure proper healing of their bone.
References
- Greenstick Fracture. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK513279/
- Greenstick Fractures. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17812-greenstick-fractures
- Greenstick fracture. Wikipedia. https://en.wikipedia.org/wiki/Greenstick_fracture
- Greenstick Fractures. Physiopedia. https://www.physio-pedia.com/Greenstick_Fractures