Supracondylar Humerus Fracture
Overview
An injury to the humerus, or upper arm bone, at its narrowest point, directly above the elbow, is known as a supracondylar humerus fracture.
Although they are uncommon in adults, supracondylar humeral fractures are a common elbow injury in children.
The incidence peaks between the ages of 5 and 7. Falling onto an extended hand with the elbow extended is the most frequent mechanism of injury (a small percentage occurs from landing directly onto a flexed elbow).
Pediatric patients are more likely than adults to experience elbow fractures. When children fall, they frequently use their outstretched arms as a safety mechanism, raising the risk of elbow fractures. Supracondylar fractures of the humerus account for up to 18% of all pediatric fractures and 60% of elbow fractures.
Dr. Gartland (1959) discovered that even experienced trauma surgeons experience anxiety and trepidation when treating supracondylar humerus fractures. Orthopedic specialists continue to face significant challenges in treating these fractures, despite advances in their evaluation and treatment.

Treatment guidelines and supracondylar humerus Fracture patterns are frequently described using the modified Gartland classification. Because there is a chance of cerebral injury, vascular injury, and compartment syndrome, these injuries can be quite serious. Malunion and deformity can also result from inadequate reduction and fixation. However, some patients who experience a malunion may eventually function satisfactorily.
Due to the proximity of surrounding neurovascular structures, injuries are common, necessitating a meticulous and comprehensive assessment. Not all cases require surgery. A hard cast may be sufficient in some cases to aid in healing.
A supracondylar humerus fracture may result in malunion, or crooked healing, as well as damage to blood vessels and nerves.
Relevant Anatomy
The elbow joint allows your forearm to rotate by bending like a hinge. Your elbow consists of three main bones. The ulna, radius, and humerus are these. Ligaments, tendons, and muscles hold together every bone in your elbow.
Elbow fractures come in different varieties. Some are large. One of these is a supracondylar fracture of the humerus. Some are more diminutive. An instance of this would be an epicondylar fracture, which affects only the elbow’s tip. If left untreated, any kind of fracture can seriously harm tendons, muscles, and nerves.
The kind of fracture that happens in the humerus is called a supracondylar fracture. The thick bone that joins your elbow to your shoulder is called this. Just above the joint, the fracture happens close to the elbow.
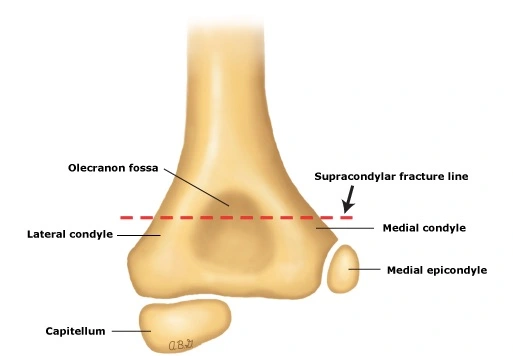
The distal end of the humerus breaks just above the elbow joint, a condition known as a supracondylar fracture. The humerus’s transverse section is roughly round, but it becomes flatter as it descends to meet the distal end of the humerus.
There are both articular and non-articular structures at the distal end of the humerus. The anterior coronoid and radial fossa, posterior olecranon fossa, medial and lateral epicondyles, and anterior coronoid and radial fossa make up the non-articular structure. Whereas the articular structure includes the lateral capitulum articulating with the radial head and the medial trochlea articulating with the ulna.
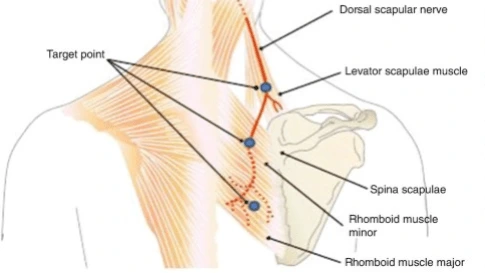
The ulnar nerve runs in a groove on the back of the medial epicondyle, which is the location of the common origin of the forearm flexor musculature. The common origin of the forearm’s extensor musculature is located on the lateral epicondyle. The distal fragment rotates and moves as a result of the attachment of these muscles. Permit the brachial artery and median nerve to pass through the anterior aspect of the distal humerus.
The brachial artery, which is frequently involved in supracondylar humeral fractures, is located just superficial to the brachialis muscle along the anteromedial aspect of the distal humerus. Before passing through the elbow and entering the supinator muscle, the radial nerve passes between the brachialis and brachioradialis muscles.
Epidemiology
The most frequently fractured area in children around the elbow is the supracondylar region of the distal humerus. The majority of the time, they affect kids between the ages of 5 and 7. The incidence steadily declines with age, with the median age being roughly six years old. While some studies report a higher prevalence in females, others report a higher prevalence in males. A recent epidemiological study, however, did not discover any appreciable gender differences. Falls on outstretched hands can result in extension-type fractures, which are far more common than flexion-type fractures.
In children, ligamentous laxity results in hyperextension of the elbow and increases the risk of extension-type fractures. Additionally, it has been noted that these fractures tend to occur more frequently on weekends and in the summer. Older children are more likely to suffer from flexion-type fractures. These wounds frequently affect the upper extremity that is not dominant. Roughly 1% of cases are open supracondylar fractures.
Mechanism of Injury
Predisposed in the pediatric population, particularly in the ages when the cortex of the supracondylar bone is thin and feeble due to skeletal maturation. The distal humerus undergoes ossification at varying ages. The supracondylar region is prone to fracture because it is remodeled between the ages of 6 and 7 and usually has a thinner, more slender cortex.
The distal humerus anatomy is particularly vulnerable to damage because it is arranged in two columns with a thin bone separating them, which creates a zone of weakness.
Supracondylar fractures typically result from falls on an outstretched hand (FOOSH), falls from a height, or falls during sports or leisure.
Extension-type injury (97% to 99%) is more common than flexion type(1-3%).
The olecranon engages on the olecranon fossa during a fall onto the outstretched hand, and if elbow extension continues, the olecranon eventually functions as a fulcrum on the fossa. However, an anterior tensile load from the anterior elbow joint capsule causes an anterior periosteum disruption and fracture.
As a result, the fracture advances posteriorly while the bone initially breaks anteriorly. When the energy level is high, the posterior cortex becomes disrupted, leading to the eventual complete posterior displacement of the distal fragment. The posterior periosteum functions as a hinge during this process. This is how fractures of the extension type work.
The most common cause of flexion-type fractures is direct trauma to the elbow. The injury progresses from the posterior to the anterior region of the distal humerus in these situations, with the anterior periosteum acting as a hinge. In the coronal plane, the distal fragment also tends to translate.
Causes of Supracondylar Humerus Fracture
A bone can break in practically any situation. An elbow fracture typically happens in one of three ways:
- Something gets struck by your elbow: It’s possible to trip and fall right onto your elbow. Alternatively, you might accidentally bump your elbow against something sturdy. A fracture may result from a direct hit.
- Your elbow gets struck by something: Your elbow could break from a blow from something in your environment. This might have happened as a result of a vehicle collision or a football helmet collision during play.
- Striking your outstretched arm: Your arm’s tendons and muscles are taut and flexed when it is fully extended. Should you land on your extended arm, it may cause bone fragments to separate from one another.
Risk Factors
Although they can affect older children as well, supracondylar fractures are most common in children under the age of seven. Additionally, they are the most typical kind of fractures in kids that need to be operated on.
It was once believed that boys were more likely to sustain supracondylar fractures. However, new research (Trusted Source) indicates that girls are equally prone to this kind of fracture as boys.
Summer-time is the most likely season for the injury to happen.
Symptoms of Supracondylar Humerus Fracture
A comprehensive examination of the entire upper extremity should be done because supracondylar fracture frequently presents with associated forearm fractures, soft tissue damage, neurologic injury, and a significant risk of developing compartment syndrome.
Among them are:
History
The onset of pain deserves special attention in the classical history of an outstretched hand fall followed by pain and swelling over the elbow and loss of upper limb function.
It is critical to determine whether the pain is coming from a fracture or the late-onset (hours after the injury) muscle ischemia.
Observation
- Painful swelling in the forearm and elbow, making movement difficult.
- It is, bruises, and skin puckering (which happens when the proximal fragment crosses the brachialis muscle and “puckers” the deep dermis)
- A bleeding puncture wound suggests that there is an open fracture.
- The so-called “S-deformity” is commonly found in displaced extension-type fractures.
Vascular status evaluation
Up to 10% to 20% of displaced fractures have vascular compromise. The injured extremity’s wrist needs to be palpated for both radial and ulnar pulses. Other indicators of perfusion, such as color (the hand should be pink), temperature, capillary refill (less than 2 seconds), and oxygen saturation on the pulse oximeter, must be examined in cases of pulselessness, also known as pulseless hand.
CLASSIFICATION
- Class I: Radial pulse and warm, red, well-perfused
- Class II: well perfused, but there is no radial pulse
- Class III: poorly perfused, with a blanched or cool blue appearance; no radial pulse
Neurologic status
Neuropraxias are common and usually resolve with the restoration of normal alignment and lengths, whereas neuropraxia typically resolves in two to three months. The degree of involvement and potential progression/regression of the nerve’s symptoms is essential both before and after treatment.
- The most likely site of involvement in postero-lateral displacement of the distal fracture fragment is the Anterior Interosseous Nerve Branch (AIN) of the median nerve. A child may present with no sensory loss in the hand but a weak “OK sign” (e.g., more of a pincer grasp than an OK sign) on physical examination.
- A diminished sense in the dorsal aspect of the hand and weak wrist extensors can be used to assess radial nerve impingement, which usually happens when the distal fracture fragment is displaced posteromedially.
- The ulnar nerve is powerless to damage from flexion-type supracondylar fractures, and loss of sensation in its distribution may occur as a result of hand intrinsic muscle weakness.
Compartment syndrome is characterized by severe pain, anterior skin puckering, ecchymosis, and vascular compromise.
Gartland Classification of Supracondylar Fracture
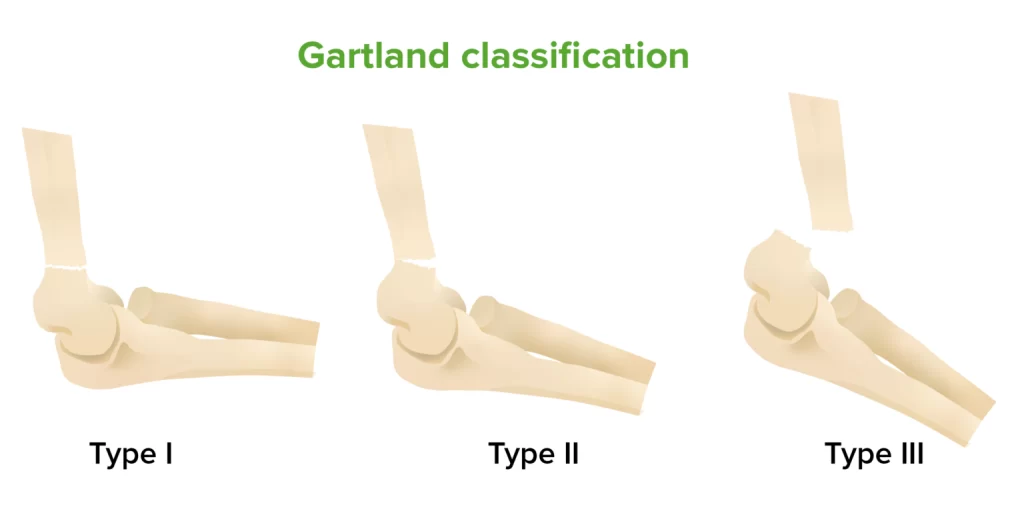
Children’s supracondylar fractures have been categorized based on Gartland’s system. Depending on how the distal fragment is displaced and the mechanism of injury, fractures can be either extension- or flexion-type injuries. The most frequent kinds of fractures are extension-type ones, in which the distal fragment is longer than the proximal fragment. At first, three categories for extension injuries were established: nondisplaced, moderately displaced, and severely displaced.
Wilkins added a division of type II injuries based on the existence or lack of a rotational deformity to Gartland’s original classification. To indicate multiplanar instability with a completely torn periosteum, Leitch added the IV type of fracture. When total instability of the fracture is present, this subtype of the fracture is identified intraoperatively.
The following is the changed Gartland classification:
- Type I: There are either no fractures or very little (less than 2 mm) displacement.
- Type IIA: Posterior hinge intact and displaced fractures (>2 mm)
- Type IIB: Malrotation and displaced fracture with an intact posterior hinge
- Type III: Completely displaced fractures involving the posterior periosteum being disrupted
- Type IV: Fully displaced fractures with multidirectional instability are classified
Diagnosis
Physical Examination
There might be a history of falling on a flexed elbow or an outstretched arm that resulted in an extension-type fracture. As it accounts for less than half of all fractures, a non-accidental injury needs to be ruled out despite its rarity. A history of pain, swelling, or deformity in the affected limb may be provided by the child or caregiver. Young children might not want to use the limb that is injured.
The distal neurovascular status and the integrity of the soft tissue envelope of the affected limb need to be carefully evaluated. Any additional injuries need to be thoroughly assessed and recorded as well.
The arm might be bruised, larger, and malformed. Any bleeding near the elbow requires evaluation as it may indicate an open fracture. An S-shaped deformity is a typical deformity for an “off-ended” Gartland III injury. A “pucker sign” in the antecubital fossa could mean that the brachialis muscle, which indentations the deep dermis, was punctured by the proximal fragment.
This signal should warn the attending clinician about the possibility of a brachial artery or median nerve injury as it indicates a high-energy injury. The surgeon should exercise caution when performing reduction because these structures could become trapped between the fracture fragments. Additionally, these individuals run the risk of developing compartment syndrome.
It is necessary to carefully evaluate and record the functions of the radial, ulnar, anterior interosseous, and median nerves. Documenting each nerve’s motor and sensory abilities is considered best practice. Up to 49% of cases have been reported to involve neurological injuries. It has been reported that 10–20% of displaced supracondylar humerus fractures have vascular compromise. In a similar vein, approximately 11% of fractures have been reported to have traumatic neurapraxia, with the ulnar nerve being most frequently injured in flexion-type injuries and the anterior interosseous nerve most frequently involved in extension-type fractures.
As many as 38% of cases of displaced Gartland III fractures may result in brachial artery injury. It is crucial to check the limb’s perfusion in the area distal to the fracture. Pulses in the ulna and radii should be evaluated. Measure the capillary refill time and take note of the ipsilateral hand’s temperature and color. The “pulseless pink, perfused hand” and the “pulseless, pale, cold hand” need to be distinguished from one another.
Some children have good collateral circulation from the elbow, which explains why their hand is perfused but pulseless. While both cases need immediate attention, the latter requires surgery because there is evidence of an ischemic limb. There will likely be vascular compromise and entrapment of both an artery and a nerve within the fracture site if there is a neurological deficit and a pulseless hand.
Similarly, a thorough neurological evaluation is necessary and should be repeated after each intervention. While a thorough nerve examination on children is difficult to perform, some games, such as rock, paper, scissors, and ok, can help with motor assessment. The child is asked to abduct the fingers (scissors) to test the motor function of the ulnar nerve, make a fist (rock) to test the median nerve and stretch the fingers (paper) to test the radial nerve. Finally, the anterior interosseous nerve is evaluated by having them sign ‘ok’.
Radiographic Evaluation
To make the diagnosis, plain elbow radiographs are needed. Confirming the type of fracture (flexion versus extension), degree of displacement, malrotation, and comminution requires anteroposterior and lateral views. In children, the elbow is primarily cartilaginous. At one year of age, the capitellum is the first epiphyseal center to appear.
Adequate knowledge of the ossified of the distal humerus with the age of look and fusion of all of the epiphyseal centers, like the proximal radius or ulna, is needed to understand elbow radiographs for kids accurately.
Anteroposterior (AP) View
It is possible to observe a transverse or short oblique fracture line in the distal humerus’ supracondylar region. These can be tricky to spot, and in nondisplaced fractures, they might even go unnoticed.
Baumann’s Angle: In the coronal plane, this is also referred to as the humerocapitellar angle. It is the angle formed by a tangential line that crosses the capitellar physis and a line that runs along the humerus’ longitudinal axis. 64–81 degrees from the longitudinal axis line is considered normal. A cubitus varus deformity is suggested by an increased Baumann’s angle. A trustworthy measurement tool for coronal plane alignment is Baumann’s angle.
Radiocapitellar Line: In every view, a line drawn along the radius’s long axis should intersect the capitellum. Unless there is a radial head/neck fracture present, this is typically unbroken in cases of supracondylar fractures.
Lateral View
Posterior Fat Pad Sign: The posterior fat pad is located next to the olecranon fossa when the elbow is bent. Any bone fracture within the elbow that occurs intra-articularly results in bleeding at the fracture site. The hematoma or effusion that results causes the fat pad to separate from the olecranon fossa. A positive posterior fat pad sign is produced as a result. Numerous scholarly investigations have documented the significance of detecting the existence of a posterior fat pad sign in the identification of occult or nondisplaced intra-articular elbow fractures.
Anterior Humeral Line: The middle third of the capitellum must be divided by a longitudinal line drawn on the lateral view along the anterior humeral cortex. In children younger than four, the line may cross the anterior third of the capitellum. An extension-type fracture pattern is indicated if the line is anterior to the capitellum.
Angiography
Before a decrease in the number of cases of vascular compromise, angiography is not advised. Arteriography before reduction is not advised by the Pediatric Orthopedic Society of North America (POSNA) since it postpones treatment.
Different Diagnosis
In children, a sizable section of the distal humerus is cartilaginous. In very young children, there may be uncertainty regarding the diagnosis, despite the ossification centers appearing predictably around the elbow. Among the differential diagnoses are:
- Fractures to the radial head
- Fractures of the distal humeral medial or lateral condyles
- Another differential diagnosis to rule out in cases like these is transphyseal fractures of the distal humerus, which should not be confused with accidental damage.
- The history usually indicates a pulled elbow, and radiographs are rarely taken in these situations.
Treatment of Supracondylar Humerus Fracture
Every patient needs to be evaluated using the Advanced Trauma Life Support (ATLS) guidelines. All pediatric injuries should be classified as non-accidental.
Non-Surgical Treatment
For minimally displaced Gartland IIA fractures and nondisplaced Gartland I fractures, nonoperative management is acceptable. The handling of Gartland II fractures has generated debate. As long as the fracture alignment is satisfactory, non-operative management of Gartland II injuries is possible. When medial column comminution is present, displacement and malunion may happen.
Medial column collapse poses a risk of developing a cubitus varus deformity. If, on lateral radiographs, the anterior humeral line does not cross the capitellum, recurvatum deformity due to malunion may result. Three conditions make non-operative treatment of Gartland II fractures contraindicated: medial comminution, posterior displacement, and excess swelling.
Non-operative management includes immobilization in the neck and grasp or an above-elbow cast that keeps the elbow at 80 to 90° of flexion for a period of three to four weeks. The vascularity of the forearm may be compromised by excessive swelling, which may result in compartment syndrome. For Gartland I fractures, above-elbow casts are more effective at relieving pain than a collar and cuff.
According to one study, patients who were treated with a cast for displaced fractures of the Gartland II type experienced satisfactory functional outcomes, though some of them developed cubitus varus. When a patient has significant elbow swelling, they should avoid excessive flexion as this can lead to compartment syndrome.
In the past, traction was applied to treat displaced fractures. It can be used in low-resource settings in low- and middle-income countries where surgical equipment is restricted.
Surgical Treatment
Displaced Gartland II and Gartland III fractures should be treated surgically. Patients with open fractures, compartment syndrome, and neurovascular compromise should receive urgent surgical care. For closed injuries, surgical management entails closed reduction and percutaneous pinning using K-wires.
For irreducible fractures, vascular exploration, and unsuccessful closed reduction, open reduction may be necessary. When treating complex fracture patterns that may result in concurrent neurovascular injuries, orthopedic surgeons should make sure they are capable of handling the related injuries and have a vascular surgeon available to assist during the procedure.
Open Reduction and Percutaneous Pinning
When the closed method is unable to achieve reduction, open reduction becomes necessary. Specifically, anatomical reduction may be impeded by soft tissue/neurovascular structures that become trapped in the fracture site. Open fractures may also require open reduction.
When perfusion is not established post-operatively after fracture reduction and fixation, an open approach to the brachial artery must be explored. It is still debatable whether open exploration of the brachial artery should occur when there is no radial pulse but the hand is perfused after reduction and fixation.
It is advised to use an anterior technique for open reduction. The medial, lateral, and posterior approaches are examples of alternative strategies.
Closed Reduction and Percutaneous Pinning
For Gartland IIB and III fractures, this is advised. Additionally, it is recommended for Gartland IIA fractures in cases where a cast cannot achieve a satisfactory reduction and non-operative treatment (such as medial column comminution) is contraindicated.
The Technique of Closed Reduction
When a pucker sign is present, closed reduction entails in-line traction combined with “milking” of the soft tissues. ‘Milking’ aids in the release of the soft tissues, while traction pulls the fracture out to length. Applying traction requires slightly flexing the elbow.
Subsequently, the distal fragment’s varus/valgus angulation and medial/lateral translation are performed to correct the coronal plane displacement. It may be necessary to supine while adding a varus force or pronate while applying a valgus-directed force. These movements also aid in correcting rotational deformity.
While supination can aid in correcting posterolateral (external) rotation, pronation helps to correct posteromedial displacement (internal rotation) while tightening the medial periosteum. In extension-type fractures, the hyperflexion of the distal fragment corrects the sagittal plane deformity. In fractures of the flexion type, an extension might be necessary.
The Technique of Percutaneous Pinning
Bicortical constructs such as lateral pins and crossed pins (medial and lateral) can be operated.
The risk of iatrogenic ulnar nerve injury is decreased by the frequent use of lateral pin configurations. You can use one, two, or three lateral pins. The best possible distance between pins must be maintained when inserting them, either parallel or divergent. It is said that the divergent pattern is more stable than the parallel arrangement.
A capitellar starting point, as opposed to a direct lateral entry point, also improves construct rigidity for lateral pins. One method of lateral pinning to improve construct rigidity has been described: a trans olecranon fossa four-cortex purchase. It has been demonstrated that pin size influences fixation stability. It has been discovered that 2 mm pins offer better biomechanical strength than 1.6 mm pins.
When crossed pins are used instead of two lateral pins, the construct’s torsional rigidity is improved, but the risk of iatrogenic ulnar nerve injury is increased. Before placing a medial pin, a sufficient-sized incision on the medial side must be made to protect the ulnar nerve. Because percutaneous medial pin insertion carries a risk of nerve injury, it is best avoided. Extending the elbow during the insertion of the medial pin is another technique to lower the risk of iatrogenic ulnar nerve injury. The nerve is moved further posteriorly by this technique.
Physiotherapy Management
For all patients with a supracondylar fracture, physiotherapy treatment is essential to promote healing and provide the best possible result.
The purpose of physiotherapy care is to include:
- To fully and painlessly mobilize the elbow joint.
- To enhance the healing process.
- To strengthen the weakened muscles.
- For improving children’s general functional abilities.
During the Immobilization Period
- Since the elbow is usually immobilized for three weeks, it is important to keep the surrounding joints—the shoulder, wrist, and hand—moving and perform active or active-assisted exercises several times a day during that time.
- It is improper to move the elbow and to use an arm sling.
- It is important to teach postural training, which includes sitting up straight, retracting the scapula, and relaxing shoulders.
1-2 Weeks after Cast Removal
- Hot fermentation can help reduce joint stiffness.
- Mild soft tissue release can be beneficial to the arm and forearm muscles.
- Use a wand to gently perform active and active-assisted exercises, and learn to exercise painlessly throughout the day.
- Isometric exercises can help to strengthen the arms and forearms.
- Inform the child and parents how to perform routine activities like eating, writing, brushing, and dressing with the affected hand.
- Avoid pushing and weightlifting activities.
Exercise after Cast Removal for Two Weeks
It is important to focus on strengthening exercises and progressive, interactive range of motion exercises, such as passing a ball and dressing and undressing garments.
Complication
The following are immediate effects linked to neurovascular involvement:
The most common association between vascular insufficiency and pink pulseless hand involvement of the brachial artery is with Type II and III supracondylar fractures, which are often found in fractures that are displaced posterolaterally.
Compartment syndrome: 0.1% to 0.3% of cases may experience it. Elbow flexion greater than 90 degrees and related forearm fractures raise compartment pressures. In the emergency room, the elbow should be immobilized at a flexion of about 30°, and after surgery, at a flexion of 60° to 70°, to reduce the risk of compartment syndrome.
The neurologic deficit ranges from 10% to 20% of supracondylar fractures and is primarily linked to Type III fractures.
Because of the remarkable capacity for bone growth and remodeling in this age group, pediatric patients often experience long-term complications. Therefore, the radiological appearance and long-term functional outcome of a fracture may differ significantly from the immediate post-management status.
Cubitus varus deformity, also called “gunstock” deformity, is caused by a malunion. Significant issues with posttraumatic cubitus varus deformity include the shift of the medial head of the triceps, tardy postero-lateral rotatory instability (PLRI), and secondary distal humeral fractures. Contemporary methods of surgery (e.g., closed reduction using percutaneous pinning) have decreased its frequency from fifty-eight percent to approximately three percent for kids treated over supracondylar fractures. Humeral osteotomy is used to treat the condition and stop similar problems in the future.
Volkmann’s ischemic contracture can develop as a result of compartment syndrome if the associated ischemia is not treated promptly. This condition is characterized by fixed elbow flexion, pronation of the forearm, flexion at the wrist, and joint extension of the metacarpal-phalangeal joint. It may also lead to infarction.
Prognosis
The patient’s remodeling potential, injury-specific variables, and bone quality all affect the prognosis.
Remodeling Factors
Remodeled spaces are dependent upon the following:
- The patient’s age and the remaining growth potential
- The separation between a fracture and the physical
- Deformity plane
- Level of Displacement
The distal humerus physis provides 20% of the longitudinal growth of the humerus. Therefore, in cases of malunion, the supracondylar region of the distal humerus does not have a significant ability to remodel. The sagittal plane deformity at the elbow has a greater potential for remodeling than the coronal plane deformity. Younger patients, but only for sagittal plane deformity, have a higher remodeling potential because they have more growth left in them. Deformity of the coronal plane does not remodel.
Patient-Related Factors
Younger children—those under five—have greater remodeling potential than older children. Children’s distal humerus residual growth stops around age five. Obesity is a sign of worse outcomes and more severe injuries.
Injury-Specific Factors
- Level of damage
- Sufficient fixation and reduction
- The limb’s neurovascular status
The long-term prognosis of these injuries is improved by receiving the appropriate treatment on time. Higher-grade injuries may have a worse prognosis; however, results can be improved with anatomical reduction, stable fixation, and proper management of the soft tissues, including neurovascular injuries and compartment syndrome.
Gartland I fractures that are not displaced typically heal well and without incident. If cubitus varus develops in Gartland II fractures with medial comminution, it must be identified, reduced, and stabilized. Although there is a higher likelihood of neurovascular injuries in Gartland III and IV injuries, prompt and appropriate treatment can produce excellent results.
Summary
The most common fractures in children are supracondylar fractures of the humerus, which peak in frequency between the ages of five and eight. FOOSH is the most common mechanism of injury of the Supracondylar fracture of the humerus.
Pre- and post-operative neurovascular assessments are essential. The recommended medical treatment for displaced fractures without neurovascular involvement is a closed reduction with percutaneous pinning. When a child has an elbow fracture, active exercise is advised instead of passive treatment.
FAQs
Which nerve injury is common in supracondylar humerus fracture?
The most frequent initial injury is to the anterior interosseous nerve, but the most frequent postoperative complication is ulnar nerve palsy.
What is a supracondylar fracture called?
Your child’s humerus fractured just above the joint, near the elbow. This is referred to as a supracondylar (pronounced soo-pruh-kaan-duh-lr) humerus fracture. This type of elbow fracture is the most common, affecting children under the age of eight.
What is the operative treatment for supracondylar fracture?
Complications from treating supracondylar humerus fractures in children (SHFC) include residual deformity, functional deficit, and iatrogenic brain damage. Closed reduction and percutaneous Kirschner wire fixation with various configurations are the standard treatments.
What are the clinical features of a supracondylar fracture?
Severe forearm, elbow, or both arches. Swelling in your elbow. Tingling in your hand and loss of elbow function make it impossible to extend your arm.
What is the most common structure injured in supracondylar fracture?
When a supracondylar fracture of the extension type occurs, the most frequently injured nerve is the anterior interosseous nerve palsy. Median Nerve Palsy: It may have an iatrogenic or traumatic cause.
How is a supracondylar humerus fracture treated in children?
For most displaced supracondylar fractures, closed reduction and percutaneous pinning (using two or three lateral pins) are the recommended courses of care. In certain fracture patterns, medial pin placement is required, and surgical techniques are outlined to prevent nerve injuries.
REFERENCES
- Supracondylar Fracture – TeachMeSurgery. (2021, May 16). TeachMeSurgery. https://teachmesurgery.com/orthopaedic/elbow/supracondylar-fracture/
- Hecht, M. (2018, September 18). What Is a Supracondylar Fracture? Healthline. https://www.healthline.com/health/supracondylar-fracture
- Supracondylar Humeral Fracture. (n.d.). Physiopedia. https://www.physio-pedia.com/Supracondylar_Humeral_Fracture
- Hope, N. (2023, August 4). Supracondylar Humerus Fractures. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK560933/
- Clinical Practice Guidelines : Supracondylar fracture of the humerus – Emergency Department. (n.d.). https://www.rch.org.au/clinicalguide/guideline_index/fractures/Supracondylar_fracture_of_the_humerus_Emergency_Department/
- What Is a Supracondylar Fracture? (2021, April 27). WebMD. https://www.webmd.com/a-to-z-guides/what-is-a-supracondylar-fracture