HIP ARTHRITIS
What Is Hip Arthritis?
- Hip Arthritis is one of the most common causes of pain in the hip joint. Arthritis is a progressive disorder, which means that it typically starts gradually and gets worse with time. The term arthritis literally means “inflammation of the joint.”
- Hip arthritis is where cartilage in the hip joint wears down or is damaged, leaving the bone surfaces of the joint to grind together and become rough. This causes pain and stiffness, making it difficult to move the leg.
- There are different forms of hip arthritis, but all involve a loss of cartilage in the hip joint that eventually leads to bone rubbing on bone and destruction of the joint.
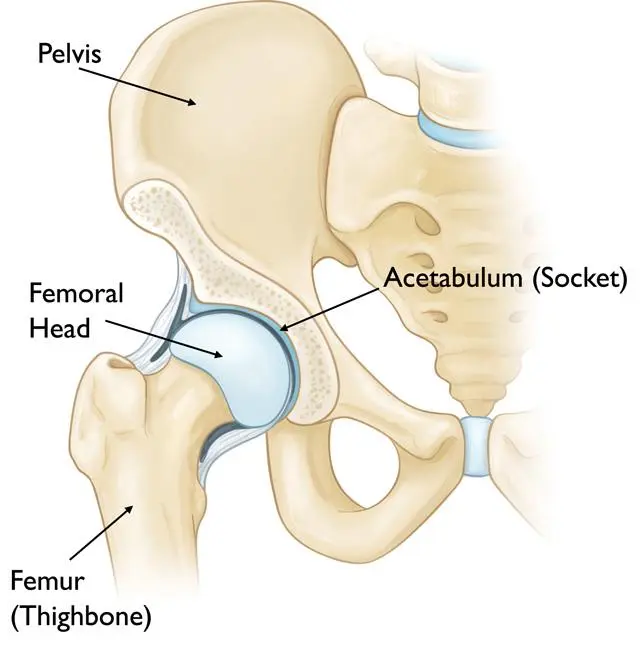
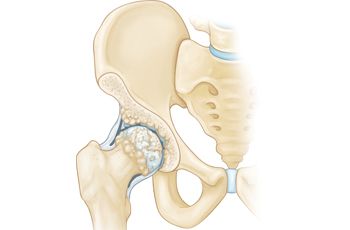
Anatomy Of The Hip Joint:
- The hip joint is a ball-and-socket joint. The ball, at the top of the femur (thighbone) is called the femoral head. The socket, called the acetabulum, is a part of the pelvis.
- The ball moves in the socket, allowing the leg to rotate and move forward, backward and sideways.
- In a healthy hip, the ball and socket are covered by a glistening layer called articular cartilage. This cartilage allows the bones of the hip joint to glide together smoothly with less resistance than ice sliding on ice.
- In addition, there is a special layer of exceptionally strong cartilage in the acetabulum which is called the labrum.
- The structure of the hip joint gives it a wide range of motion.
- It is a very stable joint because of the large area between the femoral head and the labrum-lined acetabulum.
Types Of Hip Arthritis:
There are five main types of arthritis that can affect the hip joint. They are as below:
- Osteoarthritis
- Rheumatoid arthritis
- Ankylosing spondylitis
- Systemic lupus erythematosus
- Psoriatic arthritis
There is no cure for any type of arthritis, but there are many ways to treat the pain and other associated symptoms of hip arthritis.
Osteoarthritis
- Osteoarthritis means “arthritis of the bone” and this is the most commonest form of arthritis. It is often described as the result of wear and tear on the joints, which explains why it is more common in older than younger people.
- If the smooth cartilage of hip joint wears away, the remaining rough surfaces of the ball-and-socket grind against each other, causing pain. Over time, osteoarthritis can degenerate or permanently damage the joint.
Osteoarthritis of the hip (and other parts of the body) has been associated with the following:
- Structural problems with the hip joint such as hip dysplasia, femoroacetabular impingement etc.
- Advancing age
- Obesity
- Previous damage or injury to the hip
However, osteoarthritis may also develop in the people without any of these risk factors.
Rheumatoid Arthritis
- Rheumatoid arthritis is a systemic disorder, that is, it affects your entire body and not just the hip joint. The inflammation is related to an immune system response rather than wear and tear.
- The hip joint, like other joints in the body, is protected by a special capsule that completely surrounds the joint. This capsule has a special lining (the synovial lining) and is filled with lubricant (joint fluid) that helps the joint move smoothly. Rheumatoid arthritis typically causes a swelling of the synovial lining. This causes pain and swelling, but eventually, rheumatoid arthritis can cause the bone and cartilage of the joint itself to deteriorate.
- Rheumatoid arthritis can occur in people of all ages, including children (where it is known as juvenile rheumatoid arthritis), and it is more common in women than men.
- Unlike osteoarthritis of the hip, which may occur only in one hip, rheumatoid arthritis typically occurs in both hips at the same time (and possibly other joints also).
- Rheumatoid arthritis is also associated with overall weakness and fatigue.
Ankylosing spondylitis
- Ankylosing spondylitis is a chronic inflammation of the spine and sacroiliac joint (the joint where the spine meets the pelvis) which can sometimes cause inflammation of the hip joint.
- This condition can occur in people of all ages, including children, and typically starts in a person between the ages of 17 and 35. It is generally more common in men than women.
- It is typical for people with ankylosing spondylitis to experience flares, when the condition is worse, followed by periods of remission with mild to no symptoms.
Systemic Lupus Erythematosus
- Systemic lupus erythematosus or lupus is a systemic autoimmune disorder that can affect any part of the body, including the hip joint. If lupus strikes the hip, inflammation and damage to the joint can occur.
- Lupus can occur in people of all ages but it is most common in women aged 15 to 35.
Psoriatic Arthritis
- As the name sounds, this type of arthritis is related to the skin condition psoriasis.
- Psoriatic arthritis causes joint pain, swelling, and stiffness and can affect any joint in the body, including the hip.
- Most people with psoriatic arthritis have the skin condition first (scaly red patches of skin) but it is possible to develop psoriatic arthritis before the skin condition occurs.
What are the Causes of Hip Arthritis?
Causes of hip arthritis are :
- Previous hip trauma (causing injury or fracture) – mostly resulting in unilateral hip osteoarthritis
- Joint morphology
- Genetics
- Congenital and developmental hip disease such as congenital hip dislocation, Perthe’s disease, slipped upper femoral epiphysis, developmental hip dysplasia etc.
- Subchondral bone defects
- Obesity – mostly resulting in bilateral hip osteoarthritis
- Occupation causing excessive strain on hips such as manual labor causing repeated loading
- Increase in age
- Gender (female > male)
- Sport (higher impact sport at a younger age can cause increase in articular cartilage strength, where low impact sport do not change the composition of the cartilage)
- Menopause
- Metabolic diseases and acromegaly
- Sedentary lifestyle
- Femoroacetabular impingement
- Avascular necrosis
- Overuse of Alcohol
- Steroids overdose – Drugs overdose
- Diet – low Vitamin D, C and K levels
Ethnicity – Osteoarthritis is 80-90% less prevalent in the Asian population when compared to the Caucasian population in the USA
What does hip arthritis look like?
Signs And Symptoms Of The Hip Arthritis :
Regardless of the type of arthritis, the common symptoms of hip arthritis include:
- Pain in the hip joint that may include pain in the groin, outer thigh, or buttocks
- Pain that is typically worse in the morning and lessens with activity
- Difficulty walking or walking with a limp
- Pain that worsens with vigorous or extended activity
- Stiffness in the hip or limited range of motion
- In patients with rheumatoid arthritis or lupus, fatigue and weakness may also occur.
- Arthritis often occurs in flares with remission, but some people experience a relatively stable level of pain without flares.
Any type of arthritis can involve more than one joint in the body, so a person with osteoarthritis of the hands may develop the condition in the hip as well. Rheumatoid arthritis and lupus typically affect both hips at the same time, while osteoarthritis and psoriatic arthritis may occur in one hip but not the other.
Diagnosis
If you suspect you may have arthritis of the hip, the most important first step is an accurate diagnosis. A diagnostic evaluation will likely include the following:
- Your medical history, including where you experience pain and if you limp at times
- A physical examination, in particular to see how well you can move the hip
- Radiographs or X-rays to determine if there are any abnormalities in the joint
- Blood tests to determine antibodies that may be associated with a specific type of arthritis (only if needed).

Hip Arthritis X-ray :
Mostly X-Ray of Hip Joint shows reduced Joint space with arthritic changes eg. Osteophyte formation, Reduced joint space and sclerosis of the subchondral bone plate. Subchondral cyst formation and remodeling of the articular surfaces or deformity seen mostly in advanced stages.
How To Treat The Hip Arthritis?
Treatment for Hip Arthritis: Medical Treatment
Non-Surgical Treatment (Conservative Treatment):
Nonsurgical treatment of arthritis of the hip may include any of the following:
- Anti-inflammatory medications, NSAIDs eg. ibuprofen
- Corticosteroids, injections to block the inflammation in the joint.
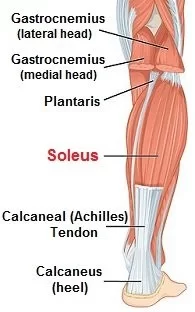
- Physiotherapy exercise programs to improve flexibility, build up strength, and maintain muscle tone. Swimming, in particular, is an excellent exercise for arthritis sufferers.
- Some types of arthritis such as rheumatoid arthritis may respond to new categories of drugs known as symptom-modifying antirheumatic drugs (SMARDs) and disease-modifying anti-rheumatic drugs (DMARDs). These are powerful new drugs, which are not appropriate for everyone with arthritis.
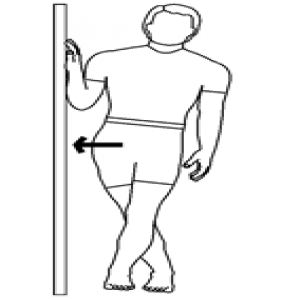
- Use of devices such as canes or walkers to make it easier and safer for you to walk.
Lifestyle modifications can also help to reduce the symptoms of arthritis of the hip. These include:
- Maintaining a healthy weight (and losing weight, if necessary)
- Appropriate pain management
- Changing activities to minimize stress on the hip
- Exercising to build up strength
If the patient doesn’t respond to any of these conservative treatments, he/she can be the candidate for the surgical treatment. Many people with arthritis with the hip are candidates for surgery. Surgery can help to reduce pain, enhance quality of life, and improve your ability to perform everyday activities with fewer or no restrictions.
Surgical Treatment :
The Joint Preservation, Resurfacing and Replacement department will prescribe the type of treatment that is appropriate for your particular type of arthritis and other factors, including your overall health, your age, and your personal preferences.
- Total hip replacement may be appropriate if the hip joint is severely damaged
- Osteotomy surgery may be appropriate in less severe cases. Hip osteotomy surgery cuts and repositions the joint surfaces in such a way that it allows the healthy part of the hip joint to bear most of the body’s weight. Only a select group of patients are candidates for osteotomy surgery.
Physiotherapy Treatment:
I. Treatment Without Surgery
Physiotherapy treatment plays a major role in the management of patients with hip arthritis. The goal is to improve strength, mobility and increase range of motion. Physiotherapy also helps relieve pain and restores normal movement in the hip and legs and also addresses pain management and functional adaptions. Patient-specific exercise programmes has shown to decrease pain and improve function in hip arthritis.
Techniques:
- Manual techniques such as passive movement to increase joint flexibility.
- Exercises
- Ice and heat
- Taping
- Stretching
- Improve stance and balance
- Aid ability to perform the activities of daily living

EDUCATION:
Educate the patient about:
- Pathology and disease process
- Role of Physiotherapy and expected outcomes of physiotherapy interventions
- Importance of weight reduction (combination of diet and exercise)
- Self-management of pain such as:
- Use of modalities such as heat and ice
- Relaxation techniques
- Exercise
WEIGHT MANAGEMENT:
- We strongly recommend weight management for people with knee or hip arthritis.
- For those who are overweight (body mass index [BMI] =25 kg/m2 ) or obese (BMI =30 kg/m2 ), a minimum weight loss target of 5–7.5% of body weight is recommended.
- It is beneficial to achieve a greater amount of weight loss given that a relationship exists between the amount of weight loss and symptomatic benefits.
- Weight loss should be combined with exercise for greater benefits.
MOBILITY ASSISTIVE DEVICES:
- Mobility assistive devices like walking sticks/canes, crutches, or walking frames can improve the mobility and independence of the patient.
- Occupational therapy also plays a role here, as they often also assist the patients with functional assistive devices like a long-handled reacher to pick up low-lying things, which will help to avoid movements that may cause pain.
EXERCISE THERAPY:
- Exercise therapy is an effective treatment modality for hip arthrosis.
- Specific exercises can increase the range of motion and flexibility, as well as strengthen the muscles of the hip and leg.
- Physiotherapists work together with the patient to develop an individualized and customized exercise program that meets the needs and lifestyle of the patient.
- The benefits of exercise can assist patients in their self-management of hip arthritis.
AQUATIC EXERCISES OR HYDROTHERAPY:
- It may be appropriate to offer aquatic exercise or hydrotherapy for some people with hip arthritis.
- This will depend upon personal preference and the availability of local facilities.
- Hydrotherapy is effective in the management of hip arthritis.
- The combination of buoyancy and the reduction of gravity greatly assists patients that are struggling to weight-bear as a result of the pain from hip arthritis.

MANUAL THERAPY:
A range of manual therapies is used in the treatment of hip arthritis:
- Massage therapy
- Soft tissue techniques and stretches
- Mobilization of accessory and physiological movements
- Manipulation
- Research is inconclusive on the effect of manual therapy in the treatment of hip arthritis.
- The immediate effect of manual therapy, specifically joint mobilization decreases pain and improve hip range of motion, especially in the elderly population.
- Joint mobilization might reduce pain, might ‘provide a stretching effect on the joint capsules and muscles, thus restoring normal arthrokinematics or may induce pain inhibition and improved motor control’ and might reduce kinesiophobia
- It may be appropriate to offer a short course of manual therapy for some people with hip arthritis.
- This should be considered only as an adjunctive treatment to enable engagement with active management strategies and only for short-term, cognisant of issues related to cost and access.

Management of hip arthritis varies according to the severity of the condition. A combination of pharmaceutical and non-pharmaceutical modalities is recommended for the optimal management of the condition. Physiotherapy plays an important role in customized exercise programs for patients living with hip arthritis.
II. Treatment After Surgery (Post-Operative Treatment)
PRECAUTIONS
If the surgical approach is posterolateral, avoid:
- Flexion past 90 degrees
- Extreme internal rotation
- Adduction past the body’s midline
If the surgical approach is anterolateral, avoid:
- Extension
- Extreme external rotation
- Adduction past the body’s midline
If the surgical approach is directly anterior, avoid:
- Bridging
- Extension
- Extreme external rotation
- Adduction past the body’s midline
DAY-1 POST-OPERATIVE
- Education of muscle relaxation
- Bed exercises
- Upper limb exercises to stimulate the cardiac function
- Maintenance of the non-operated leg
- controlled mobilization on the operated hip
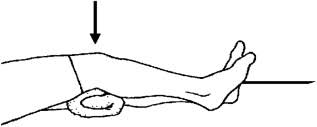
- Isometric quadriceps and gluteal contractions
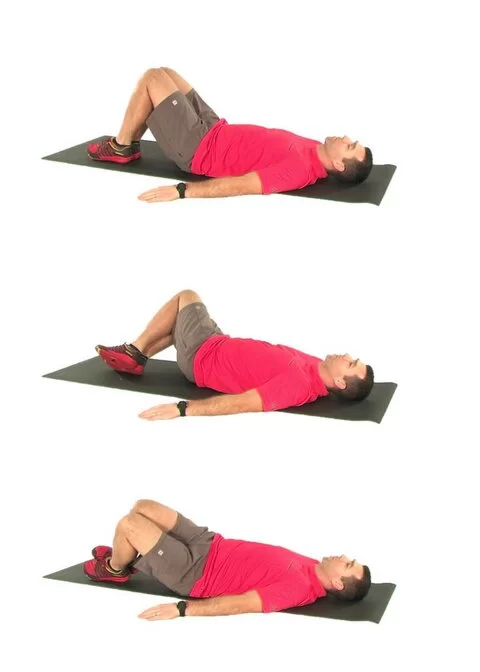
- Active-assisted (progressing to active) heel slides, hip abduction/adduction
- Bed mobilization using unilateral bridging on the unaffected leg
- Getting in and out of bed
- Getting on and off a chair with arms
- Sit to stand with a mobility assistive device (preferably a device giving more support like a walking frame or rollator)
- Gait re-education with mobility assistive device as tolerated (weight-bearing status as determined by a surgeon)
- Sitting out in a chair for a maximum 1 hour
- Positioning when transferred back to bed
DAY-2 POST-OPERATIVE
- Continue with the Day-1 treatment
- Bed exercises progressing repetitions and decreasing assistance given to patient
- Progression of distance mobilized and/or mobility assistive device
- Incorporate balance exercises
- Sitting in chair
DAY-3 POST-OPERATIVE
- Continue with the Day-2 treatment
- Stair climbing (at least 3, or as per home requirements)
- Sitting in chair
- Progression of distance mobilized and/or mobility assistive device.
HOME CRITERIA
- Independent ambulation with an assistive device
- independent transfers and activities of daily living
- stairs with supervision
- appropriate home assistance (spouse, family, visiting nurses)
HOME PLANNING
- Securely fastened safety bars or handrails in shower or bath
- Secure handrails along all stairways
- A stable chair for your early recovery with a firm seat cushion (allows knees to remain lower than hips), a firm back, and two arms
- A raised toilet seat
- Use stable shower bench or chair for bathing
- A long-handled sponge and shower hose
- Use a dressing stick, a sock aid, and a long-handled shoehorn
- A reacher allowing grasping of objects without excessive bending of your hips
- Firm pillows for chairs, sofas, and car enabling client to sit with knees lower than hips
- Removal of all loose carpets and electrical cords from the areas walked in home

6 WEEKS AFTER SURGERY
Patients are normally followed up by orthopaedic surgeon. Surgeon determines if the patient is allowed the following:
- Full range of motion at the hip
- Full weight bearing without mobility assistive device
- Driving
if the patient is allowed for these activities the therapist will progress toward:
- Gain of initial range of motion, stabilization, and proprioception
- Endurance
- Flexibility
- Balance
- Speed, precision, neurological coordination
- Functional exercises
- Return to sport
- Low-impact exercises are preferred
How To Prevent Hip Arthritis?
- Patient education – especially in primary health care
- Do Regular Exercise – Mainly Muscle strengthening and Stretching exercise
- Joint preserving surgery prior to the onset of hip osteoarthritis/early in the disease process
- Reduce or Stop of Use of Steroids if Possible
- Reduce intake of Alcohol- Drugs
- Modification of risk factors:
- Weight control
- Switching from high-impact to low-impact activities
- Minimization of pain-aggravating activities




2 Comments