Hypoglossal Nerve
Introduction
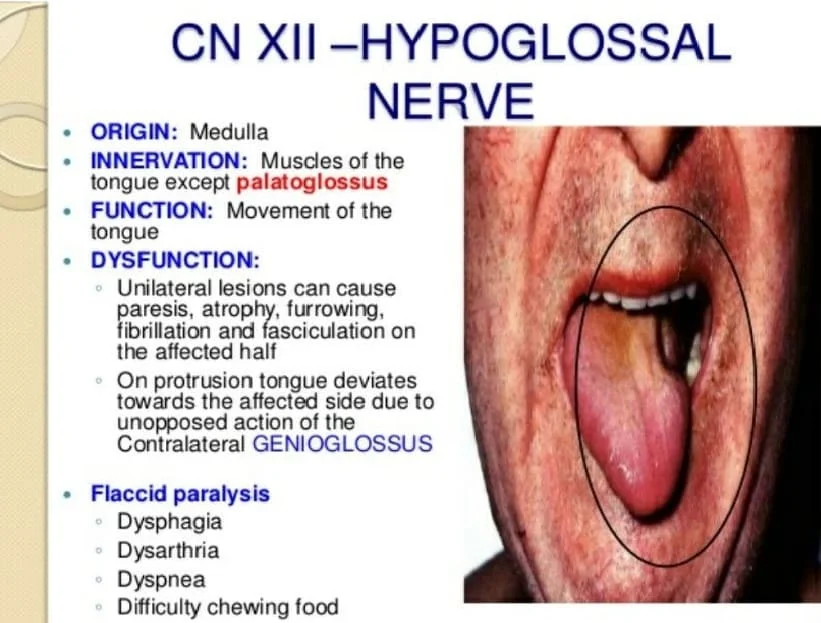
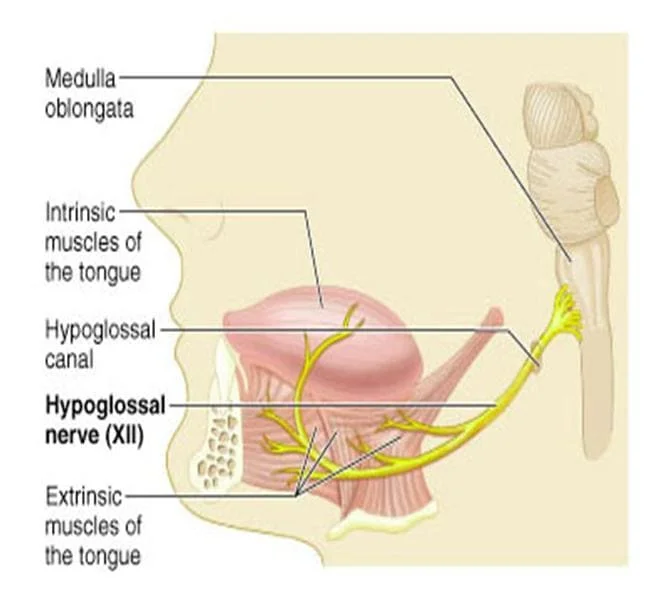
The Hypoglossal nerve is the twelfth cranial nerve, and innervates all the extrinsic and intrinsic muscles of the tongue, except for the palatoglossus which is innervated by the vagus nerve.
It is a nerve with a sole motor function.
Hypoglossal Nerve Anatomy
The nerve arises from the hypoglossal nucleus in the medulla as a number of small rootlets pass through the hypoglossal canal and down through the neck, and eventually passes up again over the tongue muscles it supplies into the tongue.
It then passes laterally across the posterior cranial fossa, within the subarachnoid space. The nerve exits the cranium via the hypoglossal canal.
Now extracranial, the nerve receives a branch of the cervical plexus that conducts fibres from C1/C2 spinal nerve roots.
These fibres do not combine with the hypoglossal nerve – they merely travel within its sheath.
It then passes inferiorly to the angle of the mandible, crossing the internal and external carotid arteries, and moving in an anterior direction to enter the tongue.
The nerve is involved in controlling tongue movements required for speech and swallowing, including sticking out the tongue and moving it from side to side.
Damage to the nerve or the neural pathways that control it can affect the ability of the tongue to move and its appearance, with the most common sources of damage being injury from trauma or surgery, and motor neuron disease.
The name hypoglossus springs from the fact that its passage is below the tongue, from hypo (Greek: “under”) and glossa (Greek: “tongue”).
Structure
- The hypoglossal nerve arises as a number of small rootlets from the front of the medulla, the bottom part of the brainstem, in the anterolateral sulcus which separates the olive and the pyramid.
- The nerve passes through the subarachnoid space and pierces the dura mater near the hypoglossal canal, an opening in the occipital bone of the skull.
- After emerging from the hypoglossal canal, the hypoglossal nerve gives off a meningeal branch and picks up a branch from the anterior ramus of C1.
- It then travels close to the vagus nerve and spinal division of the accessory nerve, spirals downwards behind the vagus nerve, and passes between the internal carotid artery and internal jugular vein lying on the carotid sheath.
- At a point at the level of the angle of the mandible, the hypoglossal nerve emerges from behind the posterior belly of the digastric muscle.
- It then loops around a branch of the occipital artery and travels forward into the region beneath the mandible.
- The hypoglossal nerve moves forward lateral to the hyoglossus and medial to the stylohyoid muscles and lingual nerve.
- It continues deep to the genioglossus muscle and continues forward to the tip of the tongue.
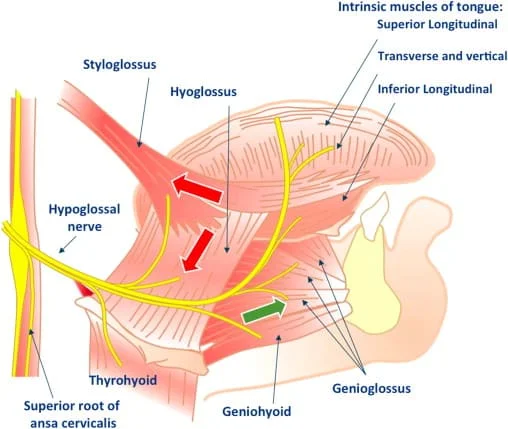
- It distributes branches to the intrinsic and extrinsic muscle of the tongue innervates as it passes in this direction, and supplies several muscles (hyoglossus, genioglossus, and styloglossus) that it passes.
- The rootlets of the hypoglossal nerve arise from the hypoglossal nucleus near the bottom of the brain stem.
- The hypoglossal nucleus receives input from both the motor cortices but the contralateral input is dominant; innervation of the tongue is essentially lateralized.
Development
- The hypoglossal nerve is derived from the first pair of occipital somites, collections of mesoderm that form next to the main axis of an embryo during development.
- The musculature it supplies develops as the hypoglossal cord from the myotomes of the first four pairs of occipital somites.
- The nerve is first visible as a series of roots in the fourth week of development, which have formed a single nerve and link to the tongue by the fifth week.
- The hypoglossal nucleus is derived from the basal plate of the embryonic medulla oblongata.
Function of Hypoglossal Nerve
Motor Function
The hypoglossal nerve is responsible for motor innervation of the vast majority of the muscles of the tongue (except for palatoglossus).
These muscles can be subdivided into two groups:
i) Extrinsic muscles
- Genioglossus (makes up the bulk of the tongue)
- Hyoglossus
- Styloglossus
- Palatoglossus (innervated by vagus nerve)
ii) Intrinsic muscles
- Superior longitudinal
- Inferior longitudinal
- Transverse
- Vertical
- Together, these muscles are responsible for all movements of the tongue.
Role of the C1/C2 Roots:
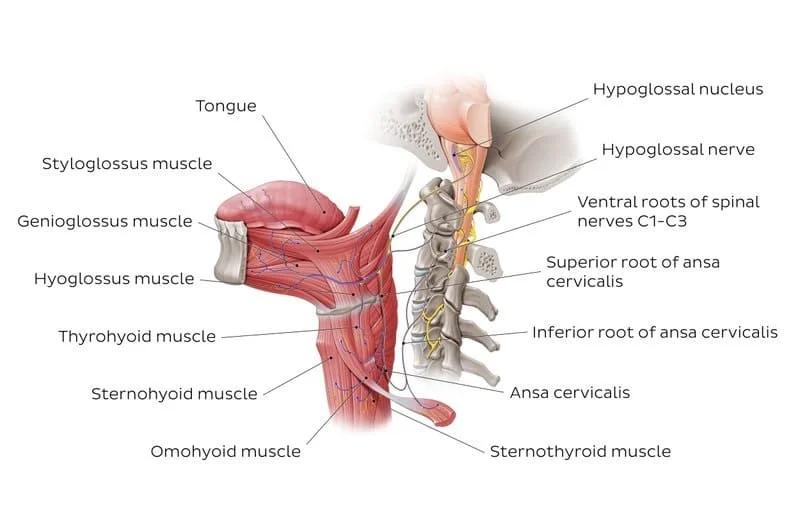
- The C1/C2 roots that travel with the hypoglossal nerve also have a motor function.
- They branch off to innervate the geniohyoid (elevates the hyoid bone) and thyrohyoid (depresses the hyoid bone) muscles.
- Another branch containing C1/C2 fibres descends to supply the ansa cervicalis – a loop of nerves that is part of the cervical plexus.
- From the ansa cervicalis, nerves arise to innervate the omohyoid, sternohyoid, and sternothyroid muscles.
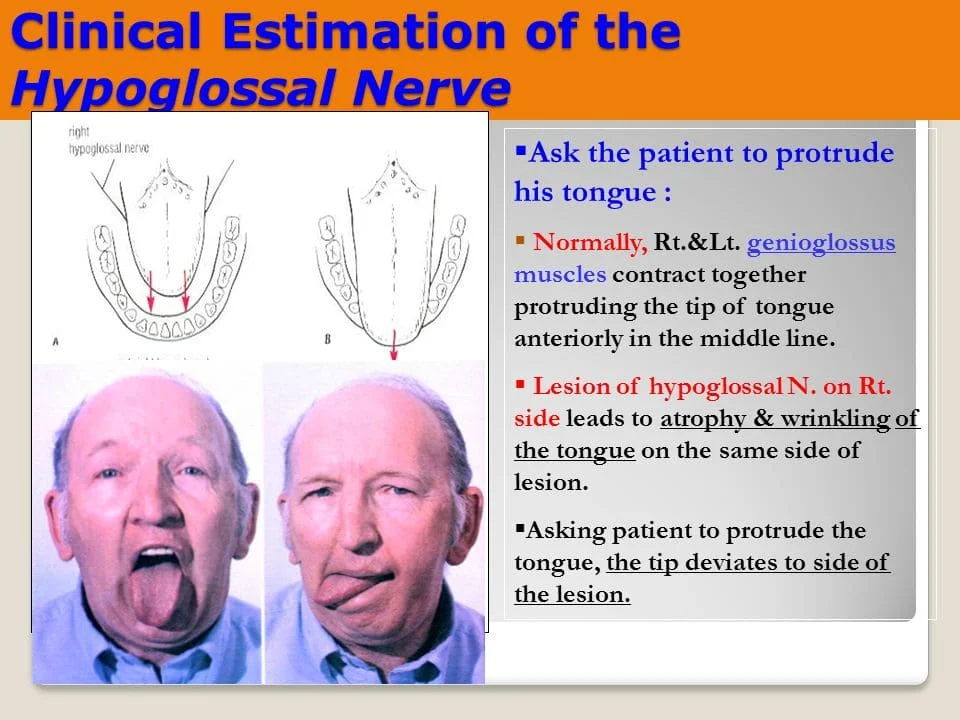
- These muscles are involved in moving and manipulating the tongue. The left and right genioglossus muscles in particular are responsible for protruding the tongue.
- The muscles, attached to the underside of the top and back parts of the tongue, cause the tongue to protrude and deviate towards the opposite side.
- The hypoglossal nerve also supplies movements including clearing the mouth of saliva and other involuntary activities.
- The hypoglossal nucleus interacts with the reticular formation, involved in the control of several reflexive or automatic motions, and several corticonuclear originating fibers supply innervation aiding in unconscious movements relating to speech and articulation.
- These muscles all act to depress the hyoid bone.
CLINICAL RELEVANCE
Damage:
- Reports of damage to the hypoglossal nerve are rare. The most common causes of injury in one case series were compression by tumours and gunshot wounds.
- A wide variety of other causes can lead to damage of the nerve. These include surgical damage, medullary stroke, multiple sclerosis, Guillain-Barre syndrome, infection, sarcoidosis, and the presence of an ectatic vessel in the hypoglossal canal.
- Damage can be on one or both sides, which will affect the symptoms that the damage causes.
- Because of the close proximity of the nerve to other structures including nerves, arteries, and veins, it is rare for the nerve to be damaged in isolation.
- For example, damage to the left and right hypoglossal nerves may occur with damage to the facial and trigeminal nerves as a result of damage from a clot following arteriosclerosis of the vertebrobasilar artery.
- Such a stroke may result in tight oral musculature, and difficulty speaking, eating, and chewing.
- Progressive bulbar palsy, a form of motor neuron disease, is associated with combined lesions of the hypoglossal nucleus and nucleus ambiguus with wasting (atrophy) of the motor nerves of the pons and medulla.
- This may cause difficulty with tongue movements, speech, chewing, and swallowing caused by dysfunction of several cranial nerve nuclei.
- Motor neuron disease is the most common disease affecting the hypoglossal nerve.
Examination:
The hypoglossal nerve is examined by asking the patient to protrude their tongue.
Other movements such as asking the patient to push their tongue against their cheek and feeling for the pressure on the opposite side of the cheek may also be used if damage is suspected.
Hypoglossal Nerve Palsy:
- Damage to the hypoglossal nerve is a relatively uncommon cranial nerve palsy. Possible causes include head & neck malignancy and penetrating traumatic injuries.
- If the symptoms are accompanied by acute pain, a possible cause may be a dissection of the internal carotid artery.
- Patients will present with a deviation of the tongue towards the damaged side on the protrusion, as well as possible muscle wasting and fasciculations (twitching of isolated groups of muscle fibres) on the affected side.
FAQ
What is the function of the hypoglossal nerve?
The tongue may move thanks to the hypoglossal nerve. It regulates the muscles of the genioglossus, styloglossus, hyoglossus, and intrinsic. These muscles facilitate swallowing, speaking, and oral substance movement.
Where is the hypoglossal nerve found?
The medulla, a portion of the brainstem, has olives from which multiple rootlets, here designated as number 12, extend to form the hypoglossal nerve. The hypoglossal canal, which is located close to the foramen magnum, the main opening for the spinal cord, is where the hypoglossal nerve exits the skull.
What controls hypoglossal nerve?
Intrinsic muscles.
The vagus nerve (cranial nerve 10) is responsible for controlling this muscle. The thyrohyoid, omohyoid, sternohyoid, and sternothyroid muscles, which regulate the mandible (lower jaw) and the hyoid bones during speaking and swallowing, are likewise innervated by the hypoglossal nerve.
What is hypoglossal weakness?
Atrophic disorders affecting the hypoglossal nerve, the 12th cranial nerve, result in atrophy or paralysis of the affected side of the tongue. The tongue is moved by this nerve. Amyotrophic lateral sclerosis, tumors, strokes, infections, and injuries can all lead to hypoglossal nerve problems.
What type is hypoglossal nerve?
Somatic efferent
The tongue musculature is innervated by the hypoglossal nerve, which is primarily a somatic efferent (motor) nerve. The sympathetic postganglionic fibers from the cervical ganglia, which innervate several tiny glands in the oral mucosa and the arteries of the tongue, are also present in the nerve.
What is the root of hypoglossal nerve?
Leaving the brainstem through the medulla oblongata’s anterolateral sulcus is the hypoglossal nerve. Its twelve roots converge laterally across the posterior cerebral fossa and unite into the distinct nerve trunk in the hypoglossal canal.
How do you test for hypoglossal nerve?
To assess the hypoglossal nerve, a patient should be asked to stick out their tongue, move it laterally, and press it up against their face to counteract the force of the examiner’s hand resting on their outer cheek.
Where does hypoglossal nerve exit?
These nerves start in the medulla’s motor nuclei and travel to the tongue muscles via the occipital bone’s hypoglossal canals. After emerging from the skull, each hypoglossal nerve curves to connect to the skeletal tongue muscles. It offers tongue movements voluntary motor control.




5 Comments