Knee Joint Effusion
What is a Knee Joint Effusion?
Knee joint effusion, commonly known as “water on the knee,” refers to the abnormal accumulation of fluid in the knee joint space. This condition can result from various underlying causes, such as injury, inflammation, or an underlying medical condition.
The knee is a hinge joint that is at risk for degenerative changes, inflammation, trauma, and infection. Acute or chronic conditions may create a knee effusion. Acute trauma and chronic systemic diseases belong to the causes. The accurate diagnosis of knee effusions needs an understanding of the basic anatomy and pathophysiology of the condition. A thorough history and physical examination are required for a correct diagnosis to be made.
An injury or health problem like arthritis may cause you to develop fluid in your knee. Treatment can depend on the cause but may involve physical therapy, medical procedures, and medication.
Each of our joints includes a tiny amount of fluid. Our unique joint lubrication system reduces friction and aids in the maintenance of smooth joint rotation.
An excessive amount of fluid buildup around a joint causes a joint effusion. It’s commonly known as “water on the knee” or swollen knee when it happens to the knee. It might be a result of a condition, an injury, or an infection.
Anatomy
As with any musculoskeletal evaluation, a thorough knowledge of knee pathoanatomy is essential. The first articulation is between the medial femoral and tibial condyles; the second is between the lateral femoral and tibial condyles; and the third is between the patella and the femur. Together, these three articulations form the compound condylar joint which is the knee. The knee can rotate internally and externally, flex and extend, and glide slightly anteriorly and posteriorly.
Supporting the knee, the largest joint in the body, are four major ligaments. Tibia dislocation on the femur is avoided by the anterior and posterior cruciate ligaments, providing anterior and posterior stability. Stability to lateral and medial stresses is provided by the medial and lateral collateral ligaments, respectively.
As the largest sesamoid bone in the body, the patella gives a greater mechanical advantage when it comes to prolonging the knee. Its posterior surface is covered in articular cartilage, and the medial and lateral retinacula maintain it in place. Through the patellar and quadriceps tendons, the quadriceps muscles apply their force on the knee.
The fibrocartilaginous structures known as the medial and lateral menisci are curved and located between the tibial and femoral articulating surfaces. They connect to the tibia by the coronary ligaments and are connected to the joint capsule at the periphery. Within the knee joint, the menisci act as shock absorbers. They also help to make the joint more elastic and lubricated. Its higher rate of injury can be related to the medial meniscus’s significantly less range of motion than the lateral meniscus.
Etiology
Many bursae, which resemble sac-like structures filled with synovial fluid, occur in the knee. The skin and bony prominences are separated by the bursae. A portion of these bursae are in interaction with the knee.
An effusion is an accumulation of fluid in the bursae and intra-articular space of a joint. Healthy people can acquire small, asymptomatic effusions. Pathology is prompted by larger joint effusions. The effusion in the knee joint may be caused by trauma, overuse, infections, systemic causes, or changes in osteoarthritis. Cysts within the popliteal fossa may also occur from these severe effusions. Hemarthrosis or synovial fluid may cause a knee effusion.
Epidemiology
Due to its weight-bearing nature and lack of stability provided by the joint consistency of the ankle and hip, the knee suffers injuries more frequently than other joints. According to reports, up to 27% of people will have knee swelling at some stage in their lifetime. While it can happen to kids of any age, it usually affects babies and teenagers.
Pathophysiology
A wide differential diagnosis can result in the first sign of a knee effusion due to any condition that may cause knee pathology. An acute or chronic atraumatic or non-traumatic, inflammatory, or non-inflammatory condition may be the cause of a knee effusion. In primary care surroundings, the most common diagnoses are gout, trauma, and osteoarthritis.
Histopathology
The knee joint is comprised of synovial fluid, which is an ultrafiltrate of blood plasma and involves hyaluronic acid, glycoproteins, lubricin, proteinases, and collagenases. An effusion may occur from molecules of about any size passing through the membrane of the inflamed synovium due to its large clefts. Furthermore, plasma and synovial fluid contain the same proteins. The hyaluronic acid in the synovial fluid lubricates and decreases friction in the knee joint. The antibacterial properties of synovial fluid aid to keep the joint’s environment sterile.
History and Physical
A detailed history and examination of the affected and contralateral knees are crucial initial steps in the evaluation of an acutely swollen knee. An internal abnormality like a meniscal tear or ligament tear may be confirmed by a knee effusion in conjunction with a recent injury history. An atraumatic effusion, on the other hand, would be more likely to be an infection or systemic disease.
Every patient who presents with knee swelling should have a history of prior surgery determined. Patients frequently mention stiffness and swelling along with a restricted range of motion. The knee might be difficult to extend fully due to a large effusion; in this case, the knee will usually rest with 15 degrees of flexion.
Red Flags
Red flags involve fever, non-weight bearing, loss of distal pulses, loss of sensation distal to the knee, open fractures, and cellulitis overlying the knee. These red flags typically require immediate evaluation.
Exam
Swelling around the patella and distention of the suprapatellar bursa are signs of a knee joint effusion. Patients might have pain while walking and a limited range of motion. The exam should involve evaluation of the skin, observation of gait, palpation of the external knee structures, active and passive range of motion, joint line tenderness, and special testing. For the medial and lateral meniscus, special tests involve the McMurray and Thessaly tests; for an ACL tear, the Lachman’s and anterior drawer tests; for a PCL tear, the posterior drawer test; and for an MCL injury, the varus and valgus stress tests. The patellofemoral joint test (compression test) shows pathology in the patellofemoral compartment.
The bulge test and the ballottement test are used to test for knee effusion. The ballottement test involves tapping the lateral patella to see if it floats outward due to effusion after pressing upward on the medial aspect of the knee two or three times. Always compare the exam to the knee that is not injured. The only symptoms of septic arthritis that affect more than 50% of patients are fever, joint pain, and a history of joint swelling.
Evaluation
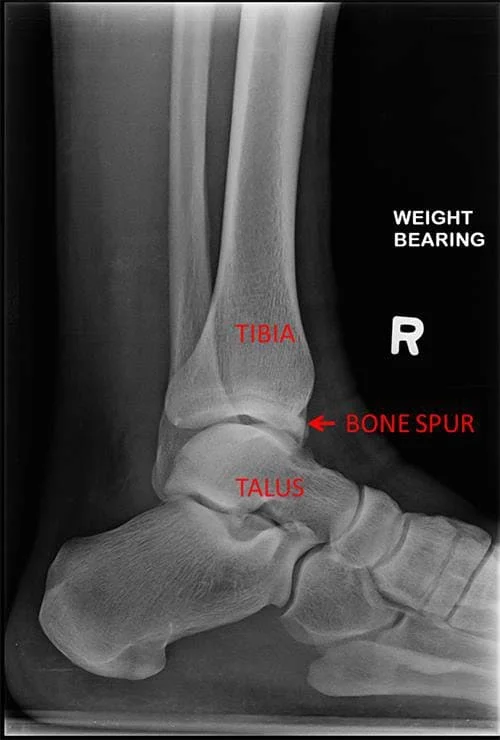
Weight-bearing radiographs in three planes should be ordered for patients who present with an acutely swollen knee to exclude trauma-related fractures. This involves AP, lateral, and axial views. An x-ray could show the fabella, a sesamoid bone inside the gastrocnemius. It is a radio-opaque marker for the synovium’s posterior border in the knee.
Popliteal mass and synovial effusion are signs of the fabella sign or displacement of the fabella. If the fabella sign is present, the suprapatellar bursa should be evaluated as it may exhibit increased opacity and widening on the same lateral knee radiograph. The finding of erosive disease, which occurs in rheumatoid arthritis (RA), or joint space narrowing, which is present in both osteoarthritis and RA, is another use for plain radiographs.
An ultrasound of the effusion can be used to perform arthrocentesis and assist in determining between a simple and complicated effusion. A simple method to find out if a wound close to a joint communicates with the joint is to use a saline load test. In the knee, 155 mL of saline is required to reach 95% sensitivity.
Arthrocentesis and a synovial fluid analysis should occur in any case of unexpected knee effusion. The Aspirated fluid requires to be examined for crystal analysis, bacterial cultures, Gram stain, and cell counts. Joint trauma is a common cause of hematuria. Fat droplets (detected by polarized microscopy) also show an articular fracture. Hemarthrosis in the absence of trauma can also be caused by other clotting disorders such as hemophilia.
Analysis of Synovial Fluid Aspirate
- The total leukocyte count with differential (polymorphonuclear leukocytes, WBC).
- evaluation of synovial fluid crystals.
- culture of bacteria and synovial fluid stained with Gram.
- Viscosity (RA: expect reduced viscosity and poor mucin clot formation).
Glucose
- Although low glucose levels are suggestive of an infected joint, they are only seen in approximately 50% of patients with septic joints, however, they can also occur in patients with rheumatoid arthritis.
- Fasting glucose levels are usually decreased to less than half of the simultaneously obtained blood levels.
It is not possible to definitively rule out septic arthritis in the presence of crystals. Less than 5% of cases include septic arthritis coexisting with gout or pseudogout.
- Joint fluid has a murky or odorous appearance.
- For septic arthritis, a cell count with a WBC of above 50,000 has been considered as diagnostic. Lower counts, however, might still be a sign of an infection (not sensitive).
- When the WBC is above 1100, a prosthetic joint becomes septic.
- Gram staining is only a third of the method used to identify infectious organisms.
- Less than 50% of the serum level will be glucose.
Non-Inflammatory Synovial Fluid
- Less than 60 to 180 cells per milliliter are present; the majority should be mononuclear.
- Less than 2000 cells/mL is the threshold reached for non-inflammatory synovial fluid, however, the majority of patients with osteoarthritis have less than 500 cells per milliliter in their synovial fluid samples.
- Non-inflammatory effusions of the knee (synovial fluid white blood cell count < 2000 cells/mcL) are usually related to osteoarthritis; other causes include acromegaly, osteonecrosis, sarcoidosis, Charcot arthropathy, amyloidosis, hypothyroidism, and sarcoidosis. Synovial fluid white blood cells higher than 2000 cells/mL are suggestive of inflammatory arthritis, which can be brought on by infection, autoimmune diseases, and arthritis-caused crystals. Pigmented villonodular synovitis should be suggested as a possibility if dark brown serosanguinous fluid is removed.
Inflammatory Synovial Fluid
More than 2000 cells per milliliter
- Traumatic: 5000 or less (w/RBCs).
- Toxic Synovitis: Less than 25% and between 5000 and 15,000 polymorphs.
- Acute Rheumatic Fever: 50% polymorphs and 10,000–15,000 polymorphs.
- Polymorphs: 75%, JRA 15,000 to 80,000.
Greater 50,000 leukocytes/mL
- WBC cells in joint fluid can be produced by various diseases, such as trauma, but infectious arthritis is usually the result of levels higher than 50,000/mm3.
- causes the most severe leukocytosis in synovial fluid, usually with 50,000–200,000 cells/mL and more than 90% PMNs.
- In patients with disseminated gonococcal infection and bacterial arthritis, lower leukocyte counts are more common in the early stages.
- A significantly inflammatory synovial effusion can be called on by non-infectious diseases like reactive arthritis, gout, pseudogout, acute rheumatic fever, and RA. Concern about infection or crystal-induced disease should arise if more than 90% of PMNs occur despite a relatively low total leukocyte count. It is not possible for certain to rule out septic arthritis despite the presence of crystals.
More than 75% of polymorphs of septic arthritis, with 80,000–200,000 cases
- The most important signs of septic arthritis in synovial fluid are the percentage of polymorphonuclear cells from arthrocentesis and the WBC count. The synovial fluid WBC count increases with an increase in the LR.
- For counts more than 100,000/microL (LR, 28.0; 95% CI, 12.0-66.0) and above 50,000/microL (LR, 7.7; 95% CI, 5.7-11.0). A polymorphonuclear cell count of at least 90% on the same synovial fluid sample suggests septic arthritis with an LR of 3.4 (95% CI, 2.8-4.2), whereas a PMN cell count of less than 90% decreases the likelihood (LR, 0.34; 95% CI, 0.25-0.47).
Other Labs
Blood Work
Infectious processes:
- Lyme disease, especially in children who have a unilateral atraumatic knee effusion.
- For post-streptococcal infection, use antistreptolysin-O.
- For syphilis, utilize rapid plasma reagin (RPR).
- Elevated WBC for inflammation, cancer, and osteomyelitis in a complete blood count (CBC).
C-reactive protein and sedimentation rate are typical signs of inflammation.
ANA to check for potential autoimmune diseases.
Studies on urine look for sexually transmitted illnesses such as trichomonas, chlamydia, and gonorrhea, which can lead to reactive arthritis, as well as urinary tract infections.
Furthermore, gonorrhea and chlamydia polymerase chain reaction tests of the affected mucosal sites ought to be taken into regard.
Reactive arthritis can be associated with shigella, campylobacter, yersinia, and salmonella, all of which can be found in stool cultures.
Causes of Knee Joint Effusion
According to statistics, 27% of people will eventually develop fluid in their knees. A traumatic injury, arthritis, or infection may result in inflammation and swelling. Fluid on the knee can be uncomfortable and is typically a sign of a problem.
The underlying illness, disease, or kind of traumatic injury that resulted in the excess fluid determines the kind of fluid that collects up around the knee. A doctor might take out a portion of the fluid and send it to a lab for testing. What caused the issue and how to fix it will be shown by the findings.
Possible causes may involve:
- A severe injury that results in a fracture or tears a ligament.
- rheumatoid arthritis.
- osteoarthritis.
- gout.
- pseudogout.
- septic arthritis.
- tuberculous arthritis.
- juvenile rheumatoid arthritis.
- exhaust, due to certain physical activities or sports.
- infections, such as Lyme disease or syphilis.
- reactive arthritis.
- inflammatory bowel disease.
- hemarthrosis, or bleeding into the joint.
- Excess weight and obesity may also raise the risk by placing strain on the knee.
Symptoms of Knee Joint Effusion
Puffiness around the knee’s bone regions is caused by excess fluid. You may feel and see one knee as greater than the other. Keeping or bending the knee can be challenging.
Typical symptoms involve:
- swelling.
- stiffness.
- a decreased range of motion.
The following symptoms require urgent medical attention:
- inability to apply force to the joint.
- not having any pulse in the feet.
- loss of feeling below the knee.
- fever.
- sweats.
- feeling sick.
The underlying reason may cause more symptoms. For example:
- Osteoarthritis: Usually worse in the morning, pain and stiffness typically get more than 30 minutes after waking up.
- Rheumatoid arthritis: Many joints are frequently affected symmetrically by pain and swelling. It could feel warm to the touch in the joint. more than thirty minutes after waking up, pain is still present.
- Traumatic injury: Bruising, severe discomfort, and trouble bearing weight on the knee are possible.
- Infection: In addition to the risk of fever, the knee could be hot. It might be recommended to visit the emergency department if there is a risk of an infection.
Diagnosis
A sore knee can last for several days for anyone. Elevation, rest, ice, and over-the-counter painkillers can often reduce symptoms.
Symptoms that warrant a visit to your doctor involve:
- You know that your knee was severely injured.
- Knee flexion and extension are not possible.
- It is uncomfortable for you to stand or walk for longer than a few minutes.
- Your left knee feels hot to the touch, it’s swelling, or both.
- Knee pain and tenderness are not getting better.
Your medical history is something your doctor will want to know. Involve any previous problems with your knees and physical activities you are involved in, like sports, that can stress the knees. A complete physical examination, which involves a range of motion examination, will also be performed.
Your doctor might then want to perform a knee aspiration to remove fluid. A long, thin needle is inserted into the joint to collect fluid to accomplish this. The process can be done in a few minutes in the doctor’s office.
One can test the fluid for:
- bacteria that could be a cause of a disease.
- glucose, protein, and crystals that could be signs of gout or other diseases.
- blood cells that might be signs of damage.
- Removing a portion of the fluid might also help your knee feel less compressed.
Imaging tests: MRIs, CT scans, ultrasounds, and X-rays can all be used to identify the source of an issue.
Diagnostic tests include:
Joint aspiration
This procedure, also referred to as arthrocentesis, involves taking a knee fluid sample for analysis, counting cells, growing bacteria, and looking for crystals like uric acid or calcium pyrophosphate dihydrate ram crystals, which are found in gout or pseudogout.
Imaging
This male 12-year-old’s knee X-ray shows a medium-severity knee effusion, marked by black arrows. It extends into the suprapatellar bursa and goes to the patella anteriorly. When there has been a history of trauma, an X-ray can determine that there is no break or dislocation. show osteoarthritis symptoms.
MRI
The phenomenon of magnetic resonance Imaging shows abnormalities in the knee joint or bones, like cartilage, ligaments, or tendons that have been damaged.
Blood tests
A doctor may be concerned about inflammation from rheumatoid arthritis, crystalline arthritis (such as gout or pseudogout), or joint infection if one knee is more swollen, red, and warm to the touch than the other. Blood tests may be performed to determine the amount of uric acid or C-reactive protein, as well as the white blood cell count and erythrocyte sedimentation rate, in addition to sending the joint fluid to a laboratory for analysis. Blood tests may identify the condition if they show the formation of antibodies to Lyme disease.
Risk factor
Anyone can overstress their knee or sustain an unexpected injury. But some things can raise your risk, such as:
- Age: In general, as you age, the likelihood of knee problems rises.
- Sports: Sports like basketball, soccer, and wrestling may cause knee strain or twisting.
- Job: Prepatellar bursitis, or a buildup of fluid in the bursa, is more frequent in activities involving extended kneeling, such as carpet layering and gardening.
- Weight: Being overweight puts strain on your knee joints, which can cause degeneration.
- Health conditions: Knee problems can be related to osteoarthritis and rheumatoid arthritis; the risk rises if you are overweight.
Treatment of Knee Joint Effusion
A majority of knee joint effusion treatments are based on the underlying cause, and each patient will need a different course of care. Options can involve:
- Aspiration, or drainage: A majority of knee joint effusion treatments are based on the underlying cause, and each patient will need a different course of care.
- Corticosteroid injections: These can decrease inflammation and support ease pain.
- Non-steroidal anti-inflammatory drugs (NSAIDs): Over-the-counter or prescription NSAIDs can give pain relief.
- Antibiotics: These can be used to treat an infection.
- A knee brace or splint: It can help to stabilize a joint.
- DMARDS: These drugs are for long-term use and can support the management of rheumatoid arthritis.
- Knee surgery or knee replacement: Sometimes surgery is the best choice for treatment.
Treatment for acute pain and swelling requires to be specific. This involves splints, cold or ice packs, partial or non-weight-bearing braces, non-steroidal anti-inflammatories (NSAIDs), or other analgesics. Treatment with drainage may be effective if there is a large effusion in the joint that is causing pain.
Before providing antibiotics, the fluid sample is required to be collected, examined, and cultured. Steroids given intraarticularly should be delayed until infection or other contraindications are eliminated.
- Septic joint: Start intravenous (IV) antibiotics for the suspected effective agent when the lab studies are sent. Staphylococci (40%), streptococci (28%), gram-negative bacilli (19%), mycobacteria (8%), gram-negative cocci (3%), gram-positive bacilli (1%), and anaerobes (1%), are the most common bacterial causes. Furthermore, an orthopedic evaluation might be required. Joint drainage is related to a rapid recovery and minimal morbidity. The advantages of arthroscopy involve joint visualization, adhesion lysis, purulent pocket drainage, and, if necrotic tissue requires to be removed, help with debridement.
- Ligamentous injuries: An outpatient referral to an orthopedic surgeon can result in the patient being put in a knee brace.
- Fractures: The severity of these might need a referral to a surgeon. For pediatric growth plate fractures, the Salter-Harris classification can be used.
- Rheumatologic conditions: The patient should be referred to a rheumatologist and treated with acetaminophen or nonsteroidal anti-inflammatory medications (NSAIDs).
- Reactive Arthritis: Antibiotics appropriate for the primary infection should be given. Acetaminophen and NSAIDs can be used to treat pain.
Differential Diagnosis
- Infection.
- Bacterial.
- Mycobacterial.
- Spirochete (Lyme, syphilis).
- Viral.
- Crystal (gout and pseudogout).
- Spondyloarthritis.
- Reactive arthritis.
- Inflammatory bowel disease.
- Hemarthrosis.
- Acute injury.
- Osteoarthritis.
- Osteonecrosis.
- Malignancy.
- Autoimmune disorders.
Home remedies for Knee Joint Effusion
In addition to medical attention, self-care practices can assist in decreasing knee joint effusion.
They can involve:
- resting the leg.
- raising the leg.
- covering the knee with a towel-wrapped portion of ice.
- use a knee brace.
- apply a mobility aid, such as a cane.
- choosing weight-management methods can decrease the burden on the knee joint in arthritis sufferers.
- taking part in low-impact activities, such as yoga, tai chi, and swimming, especially for arthritis sufferers.
Self-management
The market is flooded with knee braces. Some are designed to avoid injuries to your knees while taking part in specific sports. Following a medical procedure, some are used to support the knee or keep it from moving. Others aim to offer some temporary comfort when you’re in pain.
It is recommended to consult your physician before purchasing a knee brace. Severe injury could result from using the wrong kind or using it improperly.
Self-care measures should involve:
- When you have pain and swelling in your knee, take it easy and avoid bearing any weight.
- Would this be a chronic issue, think about avoiding physically demanding activities or bending exercises.
- Use over-the-counter pain relievers or anti-inflammatories as required.
- Raise your leg and use ice on your knee for fifteen to twenty minutes, or even for two to four hours.
- Raising your knee above your heart is the ideal position.
- Maintain a healthy weight to spare your knees needless strain.
- Exercise your legs to support and build the supportive muscles around your knees.
- Try low-impact exercises like swimming and water aerobics that won’t strain your knees.
Preventing knee effusion
Tips for preventing water on the knee may involve:
- Preventing activity by doing low-impact sports like swimming and walking.
- Avoid away from sudden movements and rough surfaces when running.
- Avoid away of repetitive movements when you can.
- Maintaining a healthy weight.
- Seeking treatment for chronic conditions like arthritis.
Recovery time
The time it takes to recover from knee effusion depends on the reason for the problem and the suggested treatment course. The cause and other factors, like the patient’s age and general health, will affect the method of treatment and recovery period. Experts suggest starting treatment 24 to 48 hours after symptoms appear to avoid complications.
Many knee effusions can be healed with treatment. But if they are the result of an ongoing condition like arthritis, they may come back.
Summary
Water or fluid on the knee also referred to as a knee effusion, can be caused by a variety of conditions, from traumatic injuries to systemic or chronic illnesses like rheumatoid arthritis.
if anyone experiences sudden, severe, or new knee swelling, they should see a doctor right away because waiting could lead to complications.
If a person’s knee feels unstable, cannot bend, cannot support their weight, or have a fever, they should get medical help right away.
FAQs
How do you treat knee joint effusion?
Rest. Try to stay away from activities that need lifting weights.
Ice and elevation. Ice your knee for 15 to 20 minutes every two to four hours to help with discomfort and swelling.
Compression. Wrapping your knee with an elastic bandage can support and control the swelling.
Pain relievers.
What are the causes of knee effusion?
Ligamentous, osseous, and meniscal injuries as well as overuse problems are the most frequent traumatic causes of knee effusion. Arthritis, infection, crystal deposition, and tumors are examples of atraumatic aetiologies. Considering the injured knee to the undamaged knee is essential.
Is walking good for fluid on the knee?
Walking and various kinds of exercise can assist in mobilizing joint fluid and lubricating the joints if you have mild to moderate osteoarthritis trouble in your knees. Walking and other knee-joint exercises are advised. With exercise, you probably notice an improvement in stiffness, soreness, and fatigue.
Is knee effusion permanent?
Many kinds of knee effusions come with treatment. However, if they’re the result of a long-term illness like arthritis, they can come back.
Does joint effusion go away?
However, there can be additional reasons for your knee swelling. An acute knee joint effusion will completely heal with the initiation of suitable treatment and knee relief.
What foods are good for knee effusion?
For those suffering from knee effusion and arthritis, dairy products particularly the low-fat variety-may be effective. Sterols and stanols: These substances, which are useful for those with knee arthritis, can be found in dairy products. These compounds also can decrease blood cholesterol levels.
How can I naturally drain fluid from my knee?
The swelling knee should be above the level of the heart and the person is at rest. This assists in draining excess fluid from the joint and decreases blood flow to it. Both decrease swelling. Although leg elevation pillows are available, regular cushions or pillows often work just as well.
How do you stop joint effusion?
Your doctor may advise rest, ice, and raising the joint (elevation) to assist with pain and swelling. The fluid could be removed from the area. Your doctor might advise using NSAIDs (over-the-counter anti-inflammatory medicines) or having a steroid injection. Or you may require surgery to repair the damage.
Is knee effusion harmful?
Fluid in the knee may reduce muscle function and lead to atrophy and weakness of the thigh muscles. Baker cyst, a sac filled with fluid. A Baker cyst in the back of your knee could grow as a result of fluid accumulation in your knee. Although a bloated Baker cyst might be unpleasant, compression and cooling usually help.
Is knee effusion bad?
Healthy people can develop small, asymptomatic effusions. Greater joint effusions are symptomatic of the disease. There are several possible reasons for knee joint effusions, involving trauma, overuse, infections, systemic causes, and changes in osteoarthritis. Cysts within the popliteal fossa are another possible outcome of these massive effusions.
What kind of doctor treats knee effusion?
Knee joint diseases are diagnosed and treated by orthopedic surgeons. Injuries like ligament rips or fractures as well as degenerative conditions like osteoarthritis may fall under this group. The knees are initially extensively examined by an orthopedic surgeon. Imaging tests like MRIs and X-rays could be performed by them.
How do you test for knee effusion?
Method 2: By placing one hand above the patella and gently pressing downward to milk the suprapatellar pouch, which drains into the knee joint, you can check for fluid retention.Then, press on the patella with your other hand. The patellar will bounce off the underlying bone if there is an effusion (patella tap test).
Does ice help knee effusion?
For the first two to three days following a knee injury, apply ice to the knee for 15 to 20 minutes every two to four hours. This will support control of the pain and decrease the swelling. To prevent your skin from getting hurt, always place a towel between the ice pack and your skin.
Is heat or ice better for knee effusion?
Heat relieves pain and muscle spasms by helping in the release of tight muscles and joints. Using ice for 24 hours and then switching to heat is the best plan of action if you have swelling. Applying heat when you initially feel knee pain is OK if swelling isn’t an issue.
Which type of exercise helps to lessen knee edema?
Depending on the underlying reason. Ask about physical therapy as soon as you get a diagnosis so you can learn suitable exercises. Stretches that improve range of motion and exercises to build muscle are two common ones.
Can fluid on the knee get worse?
Yes, if treatment is not given it may worsen. A chronic bacterial infection can spread. Meniscus tears can result in severe discomfort and limited movement if left untreated.
How can I reduce fluid in my knees naturally?
Eight Natural Ways to Quickly Reduce Knee Swelling
Rest.
Ice.
Compress.
Elevate.
Take an anti-inflammatory.
Switch to heat.
Try massage.
Do knee exercises.
What is the duration of healing for a knee effusion?
The full recovery from a knee effusion may take several weeks or months. On the other hand, more severe circumstances might require more time or care.
What is a Grade 2 effusion knee?
When only one or two joint recesses were slightly expanded by fluid, there was a small effusion (grade 1); when more than two recesses were partially enlarged, there was a moderate effusion (grade 2); and when all of the joint recesses were fully removed, there was a massive effusion (grade 3).
How can water on the knee be removed the quickest?
Methods for Draining Fluid from the Knee: You might be able to take care of this illness at home. Pain and swelling can be reduced by using the RICE technique (rest, ice, compression, and elevation). Aim to avoid placing excessive weight on your knee.
What happens if a joint effusion is left untreated?
The joint may suffer irreversible damage if treatment is avoided.
What is knee effusion on MRI?
A continuous and sensitive measure that has been related to cartilage volume loss, the development of ROA, and the risk of total knee replacement is the knee joint effusion volume as determined by magnetic resonance imaging (MRI). This could offer a means to recognize those
with an inflammatory OA phenotype who are more likely to experience the progression of the disease.
What is rice for knee effusion?
RICE—Rest, Ice, Compression, and Elevation—can be used as soon as possible after an injury, such as a sprain of the knee or ankle, to decrease pain and swelling and promote healing and flexibility.
What is the fluid called in knee effusion?
When excessive synovial fluid collects up inside or around the knee joint, it is referred to generally as “water on the knee” or knee effusion. Many common causes can lead to it, such as meniscus or ligament damage, arthritis, or prepatellar bursitis, a condition where fluid accumulates in the bursa.
Does physical therapy help knee effusion?
In the treatment of edema and effusion, physical therapy can also be essential. Initially, the physical therapist aims to determine the underlying cause of the effusion or edema. The therapist can improve the exercise regimen to reduce the quantity of extra fluid in the area with the help of
this diagnosis.
What are the stages of effusion?
Three progressive stages can be determined by the evolution of parapneumonic effusion: (I) exudative stage; (II) fibrinopurulent stage; and (III)organizing stage with pleural peel formation.
Can joint effusion return?
The accumulation of fluid in a joint is called an effusion. Following the removal of an important amount of fluid, an effusion usually develops again.
What is the recovery time for knee effusion?
The cause of a joint effusion affects how long it takes to heal. Joint effusion may last for weeks or months if one of the bones that make the joint breaks. Whenever you have joint effusion as a result of osteoarthritis, you may never fully recover from swollen joints.
How bad is a knee effusion?
You might not be able to fully bend or straighten your leg if your knee joint is overly swollen. Pain. Depending on what caused the fluid accumulation, your knee may become so painful that you cannot put any weight on it.
How long does knee effusion last?
The recovery period from a knee effusion might take a few weeks to a few months. More serious cases, however, can take longer or call for more involvement in medical care.
References
Gerena, L. A. (2022, November 15). Knee Effusion. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK532279/#:~:text=The%20knee%20contains%20multiple%20bursae,joint%20is%20called%20an%20effusion.
Image- Redirect Notice. www.google.com/url?sa=i&url=https%3A%2F%2Fhealthjade.net%2Fjoint-effusion%2F&psig=AOvVaw39u9YS9Ro1bQxGm9-EUBja&ust=1703051952504000&source=images&cd=vfe&opi=89978449&ved=0CBIQjRxqFwoTCMigja_pmoMDFQAAAAAdAAAAABAl.
Morales-Brown, P. (2023, October 12). What is water on the knee? https://www.medicalnewstoday.com/articles/187908.
Johnson, M. W. (2000, April 15). A Systematic Approach to Diagnosing Acute Knee Effusions. AAFP. https://www.aafp.org/pubs/afp/issues/2000/0415/p2391.html.
Knee effusion. (2023, October 3). Wikipedia. https://en.wikipedia.org/wiki/Knee_effusion.
Pietrangelo, A. (2023, April 17). What is Joint Effusion, or Water on the Knee? Healthline. https://www.healthline.com/health/water-on-the-knee.
Macpherson, R. (2023, June 29).Causes and Treatments of Water on the Knee (Effusion). Verywell Health. https://www.verywellhealth.com/how-to-get-rid-of-fluid-on-the-knee-5093727.




4 Comments