Knee Pain: Physiotherapy Management
What is a Knee Pain?
Knee Pain are the most common condition seen in India. People in India highly uses knee joint, This high usage may lead to more wear and tear around the Knee joint. Knee joint is also weight-bearing joint, so on relieving pain takes more time.
The knee is a complex structure and one of the most stressed joints in the body. It is the largest joint, vital for movement, playing a major role in performing day to day activity and vulnerable to injury.
The knee is the most commonly injured joint by adolescent athletes with an estimated 2.5 million sports-related injuries annually.Knee pain can be caused by a sudden injury, an overuse injury, or by an underlying condition, such as arthritis. Treatment will vary depending on the cause. Symptoms of knee injury can include pain, swelling, and stiffnes.
Knee Joint Anatomy
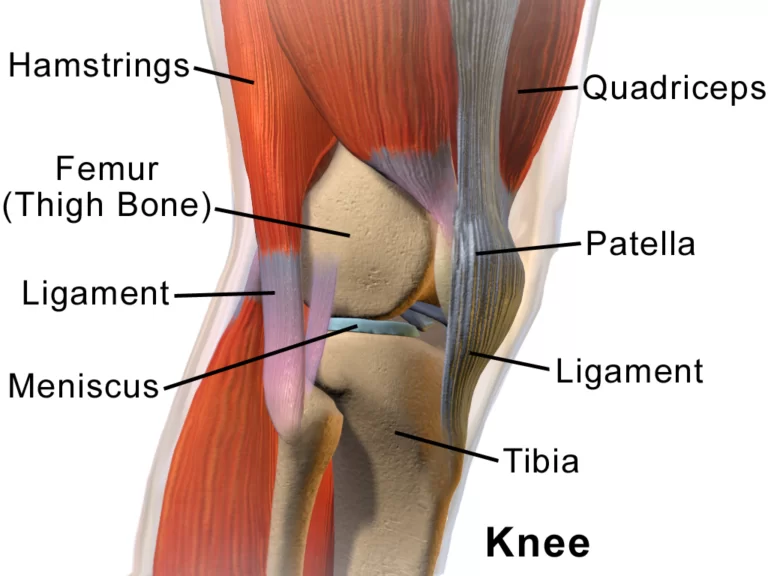
The knee joint is a hinge joint that is responsible for weight-bearing and movement. It consists of bones, meniscus, ligaments, and tendons.
The knee is designed to fulfill a number of functions.
- support the body in an upright position without the need for muscles to work
- helps to lower and raise the body.
- provides stability.
- acts as a shock absorber.
- allows twisting of the leg.
- makes walking more efficient.
- helps propel the body forward.
BONE:
The femur (thigh bone),tibia (shin bone),and patella (kneecap)make up the bones of the knee.The knee joint keeps these bones in place.
The patella is a small,triangle shaped bone that sits at the front of the knee, within the quadriceps muscle.It islined with the thickestlayer of cartilage in the body because it endures a great deal of force.
CARTILAGE:
There are two types of cartilage in the knee:
MENISCUS:
These are crescent-shaped discs that act as a cushion, or “shock absorber” so that the bones of the knee can move through their range of motion without rubbing directly against each other. The menisci also contain nerves that help improve balance and stability and ensure the correct weight distribution between the femur and tibia.
The knee has two menisci :
- medial – on the inner side of the knee, this is largest of the two.
- lateral – on the outer side of the knee.
- Articular cartilage: found on the femur, the top of the tibia, and the back of the patella; it is a thin, shiny layer of cartilage. It acts as a shock absorber and helps bones move smoothly over one another.
LIGAMENTS:
Ligaments are tough and fibrous tissues; they act like strong ropes to connect bones to other bones, preventing too much motion and promoting stability.
The knee has four ligaments :
- ACL (anterior cruciate ligament) – prevents the femur from sliding backward on the tibia, and the tibia from sliding forward on the femur.
- PCL (posterior cruciate ligament) – prevents the femur from sliding forward on the tibia, or the tibia from sliding backward on the femur.
- MCL (medial collateral ligament) – prevents side to side movement of the femur.
- LCL (lateral collateral ligament) – prevents side to side movement of the femur.
TENDON:
These tough bands of soft tissue provide stability to the joint. They are similar to ligaments, but instead of linking bone to bone, they connect bone to muscle. The largest tendon in the knee is the patellar tendon, which covers the kneecap, runs up the thigh, and attaches to the quadriceps.
MUSCLES:
Although they are not technically part of the knee joint, the hamstrings and quadriceps are the muscles that strengthen the leg and help flex the knee.
The quadriceps are four muscles that straighten the knee. The hamstrings are three muscles at the back of the thigh that bend the knee.
The gluteal muscles – gluteus medius and minimus – also known as the glutes are in the buttocks; these are also important in positioning the knee.
JOINT CAPSULE:
The joint capsule is a membrane bag that surrounds the knee joint. It is filled with a liquid called synovial fluid, which lubricates and nourishes the joint.
BURSA:
There are approximately 14 of these small fluid-filled sacs within the knee joint. They reduce friction between the tissues of the knee and prevent inflammation.
What are the Causes of Knee Pain?
Being active is one of the best things you can do for your joints and the rest of your body. But injuries can happen, and they often involve the knees.
Some of the most common problems are sprained ligaments, meniscus tears, tendinitis, and runner’s knee. If you have an old knee injury that wasn’t properly treated, it may flare up now and then or hurt all the time.
Several other things can also cause knee pain, such as:
BURSITIS:
A bursa is a sac that holds a small amount of fluid that’s under the skin above your joint. It helps prevent friction when the joint moves. Overuse, falls, or repeated bending and kneeling can irritate the bursa on top of your kneecap. That leads to pain and swelling. Doctors call this prepatellar bursitis. You may also hear it called ”preacher’s knee.”
DISLOCATED KNEECAP :
This means that your kneecap slides out of position, causing knee pain and swelling. Your doctor may call this “patellar dislocation.”
IT (iliotibial) BAND SYNDROME:
The iliotibial (IT) band is a piece of tough tissue that runs from your hip down to the outer part of your knee. When you overdo activity, it can become inflamed over time. That causes pain on the outer side of the knee. It’s common among runners when going downhill.
MENISCAL TEAR:
Sometimes, a knee injury can cause cartilage to rip. These rough edges can get stuck in the joint, which causes pain and swelling. Many times, people will have the sensation of “catching” in the joint when they are active.
OSGOOD -SCHLSTTER DISEASE :
This condition happens when you’re young, when bones and other parts of the knee are still changing. It can cause a painful bump below the knee, where a tendon from the kneecap connects to the shin. Overdoing exercise, and irritation at a point on the bottom of your knee called the tibial tubercle, often make this area hurt. The ache may come and go over time. It’s especially common in teenage boys and girls.
OSTEOARTHRITIS:
This is the “wear and tear” type of arthritis. It’s a top cause of knee pain after age 50. This condition causes the knee joint to ache or swell when you’re active. Joints affected by osteoarthritis can also be stiff early in the day.
PATELLAR TENDINITIS:
This means you have inflammation in the tendon that connects the kneecap to the shinbone. Tendons are tough bands of tissue that connect muscles to your bones. When you overdo exercise, they can become inflamed and sore. You may also hear it called “jumper’s knee” because repetitive jumping is the most common cause.
PATELLO-FEMORAL PAIN SYNDROME :
Muscle imbalance, tightness, and alignment problems of the legs usually cause this condition. It causes knee pain and occasional “buckling,” meaning your knee suddenly can’t bear your weight. It’s not due to an injury. It’s more common for women than for men.
FRACTURES :
With severe knee trauma, such as motor vehicle accidents and impact traumas, bone breakage (fracture) of any of the three bones of the knee can occur. Bone fractures within the knee joint can be serious and may require surgical repair as well as immobilization with casting or other supports.
CHONDROMALACIA PATELLAE (CMP):
Chondromalacia patellae (CMP) is referred to as anterior knee pain due to the physical and biomechanical changes . The articular cartilage of the posterior surface of the patella is going though degenerative changes which manifest as a softening, swelling, fraying, and erosion of the hyaline cartilage underlying the patella and sclerosis of the underlying bone.
GOUT :
Gout is a painful form of inflammatory arthritis that usually affects the big toe, but can develop in any joint, including one or both of the knees. It forms when your body has high levels of uric acid. This acid forms sharp crystals that cause sudden bouts of pain, swelling, and tenderness.
TUMORS involving the joint are extremely rare. They can cause problems with local pain.
The collateral ligament on the inside of the knee joint can become calcified and is referred to as PELLEGRINI-STIEDA SYNDROME. With this condition, the knee can become inflamed.
What Does a Knee pain symptoms ?
Knee pain symptoms are vary depending upon Diagnosis and cause, few common symptoms are as per following.
- Pain, usually when you bend or straighten the knee (including when you go down stairs)
- Swelling
- Trouble putting weight on the knee
- Problems moving your knee
- Knee buckling or “locking”
If you have these symptoms, Consult your doctor. They will check your knee. You may also need X-rays or an MRI to see more detail of the joint. What Does a Knee Injury Feel Like?
Diagnosis
Clinical Examination:
Subjective :
Patient Intake:
History of present condition (HPC) (Was there trauma or was it insidious onset? Mechanism of Injury?)
Special Questions (Region-specific historical examination):
- Any back or leg pain? (Is pain in a dermatomal region – pain in the knee can be referred from the back)
- Is there hip or ankle pain? (Knee pain can be referred from the hip or biomechanically affected by the ankle)
- Did the patient hear a pop/click at time of injury?
- Does the knee give way? (instability/rupture of ligaments)
- Does the knee lock? (meniscus, true locking associated with bucket handle tears)
- Did the knee swell? How quickly? Where is the swelling? (Intra articular/ extra articular; immediate swelling usually indicates trauma within the knee such as ligament damage)
- Was there bruising? (Immediate bruising indicates significant trauma)
- Cough/sneeze cause pain?
- Age – The following conditions are not exclusive to these age groups but a higher prevalence is noted in these populations (elderly – OA? young – osgoods schlatters, middle aged- meniscal).
- Type of shoes ( wear patterns/age of shoes/proper design)
Additional Information :
- Past Medical History (PMH) (Pre-existing medical conditions)
- Drug history (DH) (Any relevant medications?)
- Social History (SH) (Work/sports/hobbies affected?)
- Investigations
- Radiological Considerations – any previous X-Rays or scans
- Other investigations – any recent blood test
- General Observation:
- Posture
- Movement Patterns
Movement Testing:
- AROM, PROM, and Overpressure
- Muscle Strength and length
- Clear hip and ankle with full AROM + overpressure
- If lumbar spine suspected add passive intevertebral mobilisations (PA spinous processes, PA transverse processes).
SPACIAL TESTS FOR KNEE PAIN :
- patella: patellar grinding
- ACL: anterior drower test
- PCL: posterior drower test
- MCL:valgus stress test
- LCL:varus stress test
- MENISCUS: MecMurry’s test
- Apley’s grinding
- PATELLAR GRINDING TEST: compression of patella against the femur by cupping the knee.
- ANTERIOR DROWER TEST: Patient supine with knee bend 90 degree. examiner stabilize foot withand places thumbs over the anterior knee joint line and pull the tibia anteriorly.
- POSTERIOR DROWER TEST:Patient supine with knee bend 90 degree. examiner places the thumb over the anteromedial and anterolateral knee joint line. examinor push the tibia postiriorly.
- VALGUS STRESS TEST :patient supine wiyh leg straight. examiner stabilize the medial ankle& apply lateral to medial ( valgus) force at the knee . procedure is repeat that slightly knee flexed ( 25 degree).
- VARUS STRESS TEST :patient supine with leg straight.Examiner stabilizes lateral ankle and applies medial to lateral (varus) force at the knee. procedure is then repeat the knee flexed at 25 digree.
- APLEY’S GRINDING TEST: Paitent prone with knee flexed 90digree.Examiner applied downward force on the foot and rotate internally / externally.
- MECMURRY’S TEST : patient in supine wiyj the hip and knee flexed 90 digree.examiner stabilized the patient knee over distal quadriceps muscles and grips patient heel with the other hand and apply long axis compration . examiner then rotates the tibia internally while applying varus force.examiner then rotates the tibia laterally while applying the valgus force .
X-RAY FINDINGS :
- radiographs taken to investigate knee joint pathology, often in the context of trauma. It usually comprises an AP and lateral projection, although other non-standard, modified projections can be used for specific indications.
- Projections: Standard projections:-
- :AP view
- demonstrates the distal femur, proximal tibia/fibula and the patella in the AP position
- ideal projection to assess the tibial plateau and tibiofemoral alignment
- :horizontal beam lateral view
- orthogonal projection to the AP, routinely done in trauma horizontal beam to better ~demonstrate any joint effusions
- ideal projection to assess lipohaemarthrosis
- used to examine the location of the patella and the patency of the patella tendon
Additional projections:-
- rolled lateral view:
- often performed on bed-bound patients with suspected arthritis
- orthogonal view of the AP projection:
- demonstrate the joint space, yet sacrifices any assessment of fluid levels
- skyline (Merchant view):
- superior-inferior projection of the patella; this is an ideal projection for patients that are better suited in the supine position
- skyline (Laurine view):
- inferior-superior projection of the patella; this projection is best suited to patients able to maintain a semi-recumbent position on the examination table
- knee AP weight-bearing view:
- often used in the context of orthopaedic appointments to obtain images of the knees in their natural anatomical position
- knee intercondylar view:
- view utilised to demonstrate intercondylar space, often used for OA and suspected tibial plateau fractures
- Rosenberg’s view:
- weight-bearing projection used to assess joint space-related pathology such as osteoarthritis
- oblique view:
- two views (internal and external) better demonstrating the knee joint in the absence of CT
Differential Diagnosis of Knee pain:
Differential diagnosis of knee pain based on location. Knee pain is a common complaint and has a wide differential diagnosis. The location of pain relative to the patella can hint at the etiology of the pain. The left side of the image represents the lateral side of the leg, and the right side of the image represents the medial side of the leg.
Each colored circle indicates an area of the knee that encompasses a distinct differential diagnosis. This list is not all-inclusive, as other pathologies may exist. The pathologies listed may also present atypically and cause pain at different territories of the knee.
- (A) Pain located in the area marked by the cyan circle, or at the patella, is typically worse when walking down stairs and can reveal the presence of chondromalacia, patellofemoral syndrome, patella maltracking, arthritis, or bursitis. Pain behind the knee at this location may suggest a Baker’s cyst.
- (B) Pain located in the area marked by the pink circle, or the lateral margin of knee, suggests iliotibial band syndrome. This pain can stretch up the side of the leg all the way to the hip. More rarely, pain at the lateral margin of the knee may also indicate a lateral meniscus tear, lateral collateral ligament injury, or arthritis.
- (C) Pain located in the area of the yellow circle, or above the patella, is suspicious for quadriceps tendinopathy.
- (D) Pain located in the area marked by the blue circle, or the medial margin of the knee, can indicate medial meniscus tear, medial collateral ligament injury, pes anserine bursitis, or arthritis.
- (E) Pain located in the area marked by the red circle, or the medial aspect of the knee below the joint line, is the classic location of intermittent pain associated with plica syndrome. (F) Pain located in the area marked by the green circle, or below the patella, can indicate osteochondritis dessicans, Osgood-Schlatter disease, patellar tendinitis, Sinding-Larsen and Johansson syndrome, or patellofemoral instability.
- ACL SPRAIN:
- Injury to the ACL usually occurs because of noncontact deceleration force ,as when a runner plants one foot and sharply turns in opposite direction . resultant valgus stress on the knee leads to anterior diaplacement of tibia and sprain or rupture of the ligament.
- The patient uasually reports hearing or feeling “pop” at the time of injury and must cease activity or compition immediately.swelling of the knee within two hours after the injury indicates rupture of the ligament and consequent hemarthrosis.
- Radiographs are indicates to detect possiblr tibial spine avulsion fracture. MRI of the knee is indicated as a part of presurgical evaluation.
- MCL SPRAIN:
- The patient reports a miss steps or collision that places valgus stress on the knee , followed by immediate onset of pain and swelling at the medial aspect of the knee.
- LCL SPRAIN :
- Lateral collateral ligament sprain usually results from varus stress to the knee, as occurs when runner plants on foot and then turns towerds the ipsilateral knee.
- The patient reports acute onset of lateral knee pain that requires prompt cessation of the activity.
- MENISCAL TEAR :
- The meniscus can be torn acutly with a sudden twisting injury of the knee, such as may occure when a runner suddenly changes direction.
- The patient usually reports recurrent knee pain and episodes of catching or locking of the knee joint , especially with squatting or twisting of the knee.
- MRI is a rediological test of choice because its demonstrates most significant meniscal tears.
- PATELLAR SUBLUXATION :
- Occurs more often in teenage girls.
- presents with giving- way episods of knee.
- pain is reproduced by patellar apprehension test.
- OSGOOD -SCHLSTTER DISEASE :
- The typical patient is a 13-14 years old boys / 10-11 years old girls who has recently gone through a growth spurt.
- presents with anterior knee pain localized to the tibial tuberosity. the pain wortsen with squatting , walking up or down stairs , or forcefull contraction of the quadriceps muscles.
- radiographs are usually negative.
- OA AND RA:
- OA of the fingers typically affects the distal interphalangeal joints and is frequently associated with Heberden’s nodes in this area. In contrast, RA typically affects the MCP and proximal interphalangeal (PIP) joints and is not associated with Heberden’s nodes.
- The carpometacarpal joint of the thumb is typically involved in OA.
- Swelling of the joints is hard and bony in OA. In contrast, soft, warm, boggy, and tender joints are typical of RA.
- Stiffness of the joint is a very common feature of RA but is relatively uncommon in OA. Furthermore, the stiffness of RA is characteristically worse after resting the joint (eg, morning stiffness), while the stiffness of OA, if present, is typically worse after any effort and is often described as evening stiffness. Morning stiffness in OA, when present, is usually transient or lasts no more than a few minutes, unlike the more sustained stiffness typical of RA.
- Radiographs also help distinguish RA from OA. OA is characterized by narrowing of the joint space due to cartilage loss and osteophytes due to bone remodeling, but not erosions or cysts.
- OA is classically associated with the absence of RFs and normal levels of acute phase reactants. However, RFs may be present, usually in low titer, consistent with the patient’s (older) age.
- Erosive or inflammatory osteoarthritis can cause severe and rapidly progresive arthritis in the small joints of the hands, often at middle age. Swelling in the PIPs with central joint erosion may be present. Distinction from RA can be made by characteristic findings on radiographs as well as a lack of systemic inflammation and serologic markers.
Treatment of Knee Pain:
Treatment are mainly Medical treatment in which Orthopedic surgeon examine the patient and according to which treatment are carried out. Physiotherapist are also able diagnosis the condition and accroding to Treament plan are designed.
Medical Treatment :
Medical treatment mainly done in India by Orthopedic surgeon, according to Sign/Symptoms/Diagnosis treatment plan are started. Pain relieving analgesic mainly NSAID and symptomatic other medicines are prescribed. If Orthopedic doctor’s feels that Knee Supporting brace is required they also prescribed. Sometimes they recomended Physiotherapy treatment if neded.
Physiotherapy Treatment in Knee pain :
Physiotherapists are movement experts who improve quality of life through mainly Pain relieving Electrotheray modalities and hands-on care, patient education, and prescribed exercise.
After an assessment, a physiotherapist will design an individualized comprehensive treatment program to address the specific factors causing your knee pain.
Stretching exercises:
- Doing regular lower body muscles stretching exercises may help improve the range of motion and flexibility in your knee joint. This can make it easier to move your knee.
- Before you start stretching, it’s important to spend at least 5 to 10 minutes warming up. Low-impact activities like cycling on a stationary bike, walking, or using an elliptical machine are good warmup options.
- Once you’re warmed up, do the following three stretches, and then repeat them once you’ve completed the knee strengthening exercises.
- Try to do these stretches and exercises at least four to five times a week.

Heel and calf stretching exercise :
- Calf stretching helps in improve flexibility of leg and overall function of knee joint. Calf muscle tightnes seen more in woman as compared to man due to High Heel.
Steps of Calf Muscles stretching :
- Stand facing a wall.
- Place your hands on the wall and move one foot back as far as you can comfortably. Toes on both feet should be facing forward, heels flat, with a slight bend in your knees.
- Lean into the stretch and hold for 30 seconds. You should feel the stretch in your back leg.
- Change legs and repeat.
- Do this stretch twice for both legs.
Quadriceps Muscles stretching exercise :
This stretch specifically targets your quadriceps, the muscles at the front of your thighs. Performing this move can help improve the flexibility in your hip flexors and quadricep muscles.

Steps of Quadriceps Stretching :
- Stand next to a wall or use a chair for support. Your feet should be shoulder-width apart.
- Bend one knee so your foot goes up toward your glutes.
- Grab your ankle and gently pull it toward your glutes as far as you can comfortably.
- Hold for 30 seconds.
- Return to the starting position and change legs.
- Repeat 2 times on each side.
Hamstring stretching Exercise :
This stretch targets your hamstrings, the muscles in the back of your thigh.
You should feel this stretch in the back of your leg and up to the base of your glutes. If you flex your foot, you may also feel the stretch in your calves.
Steps of Hamstring Stretching Muscles

- For this stretch, you can use a mat to add cushioning under your back.
- Lie down on the floor or mat and straighten both legs. Or, if it’s more comfortable, you can bend both knees with your feet flat on the floor.
- Lift one leg off the floor.
- Place your hands behind your thigh, but below the knee, and gently pull your knee toward your chest until you feel a slight stretch. This shouldn’t be painful.
- Hold for 30 seconds.
- Lower and change legs.
- Repeat 2 times on each side.
Muscles Strengthening exercises:
- According to the Indian Association of Physiotherapist, you can help reduce the stress on your knee joint by regularly working the muscles around your knee.
- To help strengthen your knees, focus on moves that work your hamstrings, quadriceps, glutes, and hip muscles.
Half squatting :
- Half squats are an excellent way to strengthen your quadriceps, glutes, and hamstrings without straining your knees.
- To do this exercise:
- Get into a standing squat position with your feet shoulder-width apart. Place your hands on your hips or out in front of you for balance.
- Looking straight ahead, slowly squat down about 10 inches. This is the halfway point to a full squat.
- Pause for a few seconds, then stand up by pushing through your heels.
- Do 2 to 3 sets of 10 repetitions.
Heel raises :
- This exercise strengthens the back of your lower legs, which includes your calf muscles.
- To do this exercise:
- Stand with your feet shoulder-width apart. Position yourself next to a wall or hold on to the back of a chair for support.
- Lift both your heels off the ground so that you’re standing on the balls of your feet.
- Slowly lower your heels to the starting position. Control is important with this exercise for strengthening your calf muscles.
- Do 2 to 3 sets of 10 repetitions.
Hamstring curl :
- The standing hamstring curl targets your hamstrings and glutes. It also requires good core strength to keep your upper body and hips steady.
- To do this exercise:
- Stand facing a wall or use a chair for support. Your feet should be hip-width apart.
- Lift one foot up, bend your knee, and raise your heel toward the ceiling. Go as far as you can, while keeping your upper body still and hips pointing forward.
- Hold for 5 to 10 seconds.
- Relax and lower to the starting position.
- Do 2 to 3 sets of 10 repetitions for each leg.
Knee extensions :
Using your own body weight, rather than a weighted machine, to strengthen your quadriceps helps keep added pressure off your knees.
Steps :
- Sit up tall in a chair.
- Put your feet flat on the floor, hip-width apart.
- Look straight ahead, contract your thigh muscles, and extend one leg as high as possible without raising your buttocks off the chair.
- Pause, then lower to the starting position.
- Do 2 to 3 sets of 10 repetitions for each leg.
Straight leg raises (SLR) :
The straight leg raise strengthens your quadriceps as well as your hip flexor muscles. If you flex your foot at the end of the move, you should also feel your shins tighten.
As this exercise gets easier to do, you can add a 5-pound ankle weight and gradually work up to a heavier weight as you build strength in your legs.
Steps of SLR :
- For this exercise, you can use a mat to add cushioning under your back.
- Lie down on the floor with one leg bent and one leg straight out in front of you.
- Contract the quadricep of your straight leg and slowly raise it up off the floor until it’s the same height as your bent knee.
- Pause at the top for 5 seconds, then lower to the starting position
- Do 2 to 3 sets of 10 repetitions for each leg.
Side leg raises :
- This exercise works your hip abductor muscles as well as your glutes. Your hip abductor muscles, located on the outside of your hips, help you to stand, walk, and rotate your legs with ease. Strengthening these muscles can help prevent and treat pain in the hips and knees.
- As this exercise gets easier to do, you can add a 5-pound ankle weight and gradually work up to a heavier weight as you build strength in your leg muscles.
Steps :
- Lie on your side with your legs stacked on top of each other. Cradle your head in your hand, and place your other hand on the floor in front of you.
- Raise your top leg as high as you comfortably can. You should feel this on the side of your hips.
- Pause briefly at the top, then lower your leg.
- Do 2 to 3 sets of 10 repetitions for each leg.
Prone leg raises :
- This exercise works your hamstrings as well as your glutes. As this exercise gets easier to do, you can add a 5-pound ankle weight and gradually work up to a heavier weight as you build strength in your leg muscles.
Steps :
- For this exercise, you can use a mat to add cushioning beneath you.
- Lie on your stomach with your legs straight out behind you. You can let your head rest on your arms.
- Engage your glute and hamstring muscles in your left leg and lift your leg as high as you comfortably can without causing pain. Be sure to keep your pelvic bones on the floor throughout this exercise.
- Hold your leg in the lifted position for 5 seconds.
- Lower your leg, rest for 2 seconds, then repeat.
- Do 2 to 3 sets of 10 repetitions for each leg.
Home Care of Knee Pain:
Posture and support:
Measures that can help to minimize knee strain include:
avoiding low chairs and couches that you “sink” into
sitting on a pillow to raise your seating level, if necessary
checking that you have a good sitting posture, without slouching or leaning
wearing supportive shoes and avoiding those with broken arches, as they can result in abnormal force and wear on the knee
avoiding prolonged sitting and long periods without moving, as joints may become stiff and painful without movement
2.Weight loss and diet
A Mediterranean diet can help people maintain a healthy weight and may have anti-inflammatory properties.
People who have excess weight or obesity have a higher risk of knee pain.
Carrying extra weight gives the joints more work to do. Losing it helps to reduce long-term knee pain, including pain caused by arthritis.
Extra weight on your body increases inflammation throughout the body and the knees are affected.
Eating well helps with keeping weight off.
A healthful diet means a balanced one that is:
high in fruit, vegetables, and fiber
low in meat, animal fat, and other fat
The Arthritis Foundation recommend a Mediterranean-style diet that is rich in fresh produce.
Experts urge people with OA of the knee to lose weight if they have overweight or obesity. A doctor or dietitian can help decide how much weight a person needs to lose. They can also help plan a suitable diet.
Protection, rest, ice, compression, and elevation (PRICE)
Use compression to support the knee and relieve pain.
Rest, ice, compression, and elevation may help treat mild knee pain that results from a soft tissue injury, such as a sprain.
3.Protection refers to protecting the knee from further injury, for example, by taking a break from the activity that caused it.
Rest can reduce the risk of further injury and give tissues time to heal. However, stopping all movement is not advisable, as this can lead to stiffness and, in time, muscle weakness.
Ice can help reduce swelling and inflammation. It should be wrapped in a cloth and applied for 20 minutes several times on the first day of injury. Never put ice directly the skin, as this can lead to further damage.
Compression with a knee support, for example, can increase comfort levels. The support or bandage should be firm but not tight.
Elevation, or keeping the leg raised, will encourage circulation and reduce swelling. Ideally, the knee should be above the level of the heart
Heat and cold
Heat and cold can be effective Trusted Source in treating pain in the lower back, and it has been recommended to ease joint pain that results from arthritis.
Heat relaxes muscles and improves lubrication, leading to a reduction in stiffness. Use a hot water bottle or a warm pad.
Ice, wrapped in a cloth, can reduce pain, inflammation, and swelling.
Some people may use heat to improve mobility in the morning and reduce swelling later in the day.
Remember to test any hot item before applying it, especially if it is for an older person or someone who cannot communicate easily.
FAQ
How can I relieve pain in my knee?
To relieve Knee pain
Use hot or ice packs over the Knee 2 times a Day.
Avoid activities that cause pain and alter them with other alternative activities.
Do simple stretches and strengthening exercises of the Knee Muscles.
Use Pain relieving Medicine such as ibuprofen or acetaminophen.
Use pain-relieving Cream.
Use a Knee-brace to support the knee during day-to-day activities.
How do I know if my knee pain is serious?
If your knee discomfort was brought on by a particularly harsh impact or if it’s followed by: Considerable swelling, Redness, Tenderness, or Warmth around the joint, schedule an appointment with your doctor.
How can I relieve knee pain naturally?
Following Natural Home remedies can help with many forms of knee pain.
Strengthening exercises
Stretching Exercise
Use of Correct Posture
Knee support Brace
Weight loss and diet
Pain relieving Medications
Massage around the Knee
Aromatherapy
Rest, ice, compression, and elevation(RICE)
Alternative Physical activity
Why does knee pain start?
An injury, such as a ligament or cartilage injury, may lead to knee pain. Knee discomfort can also be brought on by illnesses including arthritis, gout, and infections. Other knee pain-related conditions relieve effectively with conservative treatment and with self-care techniques. Physical therapy treatment with Knee exercise and braces is also important for permanent solution of Knee pain.
What age is knee pain common?
Knee pain is a weight-bearing joint, so it is a most common condition and it affects anyone at any age, people with more than 50 are the most frequently affected. Your knee may mostly feel joint pain, waking difficulties, and stiffness if you have osteoarthritis of the knee.
Will knee pain go away?
Even if you believe your injury is not very serious, don’t wait longer than 3–7 days for your knee pain to go away. Less severe knee pain-related conditions mostly relieve with rest and conservative treatment. One of the most frequent causes of visits to an orthopaedic physician is certainly knee discomfort.
Is Ayurvedic treatment good for knee pain?
Ayurveda offers a variety of efficient treatments and medications to treat and manage knee pain. Here are some of them: Eat some fenugreek seeds. It has a warm climate and helps treat joint problems.






30 Comments