Knee Ligament
Introduction
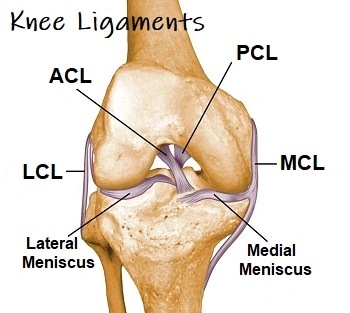
The knee joint is a complex joint that is stabilized by several ligaments. These ligaments involve the medial collateral ligament (MCL), anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), and lateral collateral ligament (LCL).
The ACL and PCL are located inside the knee joint and provide stability by preventing excessive forward and backward movement of the tibia (shinbone) in relation to the femur (thighbone). The MCL and LCL are located on the sides of the knee and provide stability by preventing excessive side-to-side movement. understanding the anatomy and function of the ligaments in the knee joint is essential for preventing injuries, managing acute injuries, and facilitating a successful recovery.
Ligaments of the knee joint
Knee ligaments are strong bands of connective tissue that connect bones to other bones in the knee joint. They play a crucial role in providing stability and support to the joint during movement. There are 4 major ligaments located in the knee joint:
- anterior cruciate ligament (ACL)
- posterior cruciate ligament (PCL)
- medial collateral ligament (MCL)
- lateral collateral ligament (LCL)
- Anterior Cruciate Ligament (ACL): The ACL is located inside the knee joint and runs diagonally from the back of the femur (thighbone) to the front of the tibia (shinbone). It prevents excessive forward movement of the tibia in relation to the femur and provides rotational stability to the knee. The ACL is commonly injured during sports activities that involve sudden stops, changes in direction, or direct impact on the knee.
- Posterior Cruciate Ligament (PCL): The PCL is also located inside the knee joint, crossing with the ACL. It runs from the front of the femur to the back of the tibia. The PCL prevents excessive backward movement of the tibia in relation to the femur and plays a role in rotational stability. PCL injuries are less common than ACL injuries but can occur during activities that involve a direct blow to the front of the knee or hyperextension of the knee joint.
- Medial Collateral Ligament (MCL): The MCL is located on the inner side of the knee joint, connecting the femur to the tibia. It provides stability and prevents excessive inward movement of the knee. MCL injuries often occur due to a direct blow to the outer side of the knee or from a twisting motion.
- Lateral Collateral Ligament (LCL): The LCL is located on the outer side of the knee joint, connecting the femur to the fibula (a bone in the lower leg). It provides stability and prevents excessive outward movement of the knee. LCL injuries are less common than MCL injuries and can occur from a direct blow to the inner side of the knee or from a twisting motion.
moreover, to these main ligaments, there are other smaller ligaments and structures within the knee joint that contribute to its stability and function. These include the menisci (cartilage pads that act as shock absorbers), the patellar ligament (connecting the patella or kneecap to the tibia), and the iliotibial band (a thick band of connective tissue that runs through the outer side of the thigh).
Functions of the knee joint ligament
The knee joint ligaments play several important functions in maintaining the stability and function of the knee joint. These functions include:
- Stability: The ligaments of the knee joint provide stability by preventing excessive movement of the bones within the joint. They act as strong bands of connective tissue that hold the bones together and limit their range of motion. This stability is crucial for maintaining proper alignment and preventing abnormal or excessive movements that could lead to injury.
- Joint Reinforcement: The ligaments reinforce the knee joint by providing additional support to the surrounding structures, such as the muscles, tendons, and cartilage. They help distribute forces evenly across the joint, reducing the stress placed on individual structures and minimizing the risk of injury.
- Joint Guidance: The ligaments guide the movement of the knee joint by controlling its range of motion. They set boundaries and limits for movement, ensuring that the joint moves within its normal physiological range. This guidance helps maintain proper alignment and prevents excessive or abnormal movements that could result in injury.
- Shock Absorption: Some ligaments, such as the menisci, act as shock absorbers within the knee joint. They help cushion the joint and absorb the impact forces generated during weight-bearing activities, such as walking, running, or jumping. This shock absorption function helps protect the bones and cartilage within the joint from excessive wear and tear.
- Proprioception: Ligaments also play a role in proprioception, which is the body’s ability to sense its position and movement in space. Specialized nerve endings within the ligaments provide feedback to the brain about the position and movement of the knee joint. This information is essential for maintaining balance, coordination, and overall joint stability.
so in the end, the knee joint ligaments work together to provide stability, reinforcement, guidance, shock absorption, and proprioception to the knee joint. These functions are crucial for maintaining proper joint alignment, preventing injuries, and allowing for efficient movement and function of the knee joint.
Injuries of knee joint ligament
Injuries to the knee joint ligaments can occur due to various reasons, including trauma, overuse, or degenerative changes. The most common ligament injuries in the knee joint include:

- Anterior Cruciate Ligament (ACL) Injury:
ACL injuries are common in sports activities that involve sudden stops, changes in direction, or direct blows to the knee. These injuries can range from mild sprains, where the ligament is stretched but not torn, to complete tears, where the ligament is completely ruptured. ACL injuries often result in pain, swelling, instability, and difficulty with weight-bearing and movement. - Posterior Cruciate Ligament (PCL) Injury:
PCL injuries are less common than ACL injuries and often occur due to direct blows to the front of the knee or from landing on a bent knee. Symptoms of PCL injuries include pain, swelling, instability, and difficulty with activities that require bending or straightening the knee. - Medial Collateral Ligament (MCL) Injury:
MCL injuries commonly occur due to a direct blow to the outer side of the knee or from twisting or bending motions. Symptoms of MCL injuries include pain, swelling, tenderness along the inner side of the knee, and instability. - Lateral Collateral Ligament (LCL) Injury:
LCL injuries are less common than MCL injuries and often occur due to a direct blow to the inner side of the knee or from twisting or bending motions. Symptoms of LCL injuries include pain, swelling, tenderness along the outer side of the knee, and instability. - Meniscal Tears:
The menisci are C-shaped parts of cartilage situated in between the femur and tibia bone that work as shock absorbers and give stability to the knee joint. Meniscal tears can occur due to sudden twisting or pivoting motions, repetitive stress, or degenerative changes. Symptoms of meniscal tears include pain, swelling, catching or locking sensation in the knee, and difficulty with movement.
Test for knee joint ligament injuries
Knee joint ligament tests are physical examination techniques used by medical professionals to assess the integrity and stability of the ligaments in the knee joint. These tests help determine if there is any damage or tearing of the ligaments and can assist in diagnosing specific ligament injuries.
- The Anterior Drawer Test
- The Lachman Test
- The Pivot Shift Test
- The Posterior Drawer Test
- The Valgus Stress Test
- The Varus Stress Test
The Anterior Drawer Test

The Anterior Drawer Test is a physical examination technique very useful to assess the continuum of the anterior cruciate ligament (ACL) in the knee joint. The ACL is one of the major ligaments that helps stabilize the knee and prevent excessive forward movement of the tibia (shin bone) in relation to the femur (thigh bone).
To perform the Anterior Drawer Test, the patient lies on their back with their knee flexed at approximately 90 degrees. The examiner stands on the affected side of the patient’s leg and stabilizes the lower leg with one hand, placing their fingers around the upper part of the calf muscle. The other hand is used to grasp the upper leg just below the knee joint.
The examiner then applies a forward force on the tibia, attempting to pull it forward. It is important to ensure that the hip and ankle are kept in a neutral position during the test, as any movement in these joints can affect the accuracy of the results. The examiner assesses for any excessive forward movement or “drawer-like” motion of the tibia compared to the unaffected knee.
If there is increased anterior translation of the tibia compared to the unaffected knee, it may indicate an ACL tear. The degree of movement and the presence of any associated symptoms, such as pain or instability, are taken into consideration when interpreting the test results.
It is important to note that the Anterior Drawer Test should be performed with caution and only by trained healthcare professionals. Improper technique or excessive force during the test can potentially cause further injury or discomfort to the patient. Additionally, this test should be used in conjunction with other clinical assessments and imaging studies for a comprehensive evaluation and accurate diagnosis of ACL injuries.
so in the end, the Anterior Drawer Test is a valuable tool for assessing ACL integrity and can assist in diagnosing ACL tears. However, it should be interpreted in conjunction with other clinical findings and imaging studies to ensure an accurate diagnosis and appropriate treatment plan.
The Lachman Test

The Lachman Test is another physical examination technique used to assess the integrity of the anterior cruciate ligament (ACL) in the knee joint. It is considered to be one of the most reliable tests for diagnosing ACL tears.
To perform the Lachman Test, the patient lies on their back with their knee flexed at approximately 20-30 degrees. The examiner stands on the affected side of the patient’s leg and stabilizes the lower leg with one hand, placing their fingers around the upper part of the calf muscle. The other hand is used to grasp the upper leg just below the knee joint.
The examiner then applies a forward force on the tibia, attempting to move it forward while simultaneously stabilizing the femur. It is important to ensure that the hip and ankle are kept in a neutral position during the test, as any movement in these joints can affect the accuracy of the results. The examiner assesses for any excessive forward movement or “soft endpoint” of the tibia compared to the unaffected knee.
The Lachman Test is different from the Anterior Drawer Test in that it assesses the ACL in a more isolated manner. It specifically evaluates the amount of anterior translation of the tibia compared to the femur, without any rotational component. This makes it a more sensitive test for detecting partial ACL tears or injuries that may not be evident during the Anterior Drawer Test.
The Lachman Test is graded on a scale from 0 to 3, with 0 indicating a firm endpoint and no anterior translation, and 3 indicating significant anterior translation and a soft endpoint. Grade 1 indicates mild anterior translation, while grade 2 indicates moderate anterior translation.
It is very important to take in mind that the Lachman Test should be performed with caution and only by a trained medical person. Improper technique or excessive force during the test can potentially cause further injury or discomfort to the patient. Additionally, this test should be used in conjunction with other clinical assessments and imaging studies for a comprehensive evaluation and accurate diagnosis of ACL injuries.
so in conclusion, the Lachman Test is a valuable tool for assessing ACL integrity and can assist in diagnosing ACL tears. It is considered to be more sensitive than the Anterior Drawer Test and is often used in combination with other tests to ensure an accurate diagnosis and appropriate treatment plan.
The Pivot Shift Test
The Pivot Shift Test is a diagnostic test used to evaluate for the presence of an anterior cruciate ligament (ACL) injury in the knee joint. The ACL is one of the major ligaments that helps stabilize the knee joint, and an injury to this ligament can cause pain, instability, and difficulty with movement.
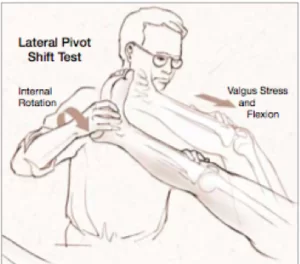
To perform the Pivot Shift Test, the patient is positioned lying on their back with their leg extended. The medical person then bends the patient’s knee to 90 degrees and applies a valgus force (outward pressure) to the knee while simultaneously rotating the tibia bone internally.
As the medical person continues to apply pressure and rotate the tibia, they will also extend the patient’s knee. If there is an ACL injury present, the tibia bone will shift or “pivot” out of its normal position, causing a noticeable “clunk” or “click” sensation as it returns to its original position.
The Pivot Shift Test is often performed in conjunction with other diagnostic tests, such as X-rays or MRI, to confirm a diagnosis of an ACL injury. Treatment options for this type of injury may include rest, physical therapy, or surgical intervention.
It is very necessary to take in mind that the Pivot Shift Test should only be performed by a trained medical person and interpreted in conjunction with other diagnostic tests and clinical findings. Additionally, this test may cause discomfort or pain for patients with an ACL injury, so it should be performed with caution and care.
The Posterior Drawer Test
The Posterior Drawer Test is a diagnostic test used to evaluate for the presence of a posterior cruciate ligament (PCL) injury in the knee joint. The PCL is one of the major ligaments that helps stabilize the knee joint, and an injury to this ligament can cause pain, instability, and difficulty with movement.
To perform the Posterior Drawer Test, the patient is positioned lying on their back with their leg extended. The healthcare provider then bends the patient’s knee to 90 degrees and sits on the patient’s foot to stabilize it.
The doctor then places their hands on the patient’s tibia bone and applies a posterior force (backward pressure) to the tibia while simultaneously pushing the femur bone forward. If there is a PCL injury present, the tibia bone will move backward more than it should, indicating a positive test result.
The Posterior Drawer Test is often performed in conjunction with other diagnostic tests, such as X-rays or MRI, to confirm a diagnosis of a PCL injury. Treatment options for this type of injury may include rest, physical therapy, or surgical intervention.
It is very crucial to take in mind that the Posterior Drawer Test should only be performed by a trained medical person and interpreted in conjunction with other diagnostic tests and clinical findings. Additionally, this test may cause discomfort or pain for patients with a PCL injury, so it should be performed with caution and care.
The Valgus Stress Test
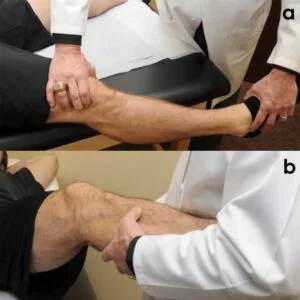
The Valgus Stress Test is a physical examination test that can be used to determine whether the medial collateral ligament (MCL) in the knee joint has been injured. The MCL is one of the major ligaments that helps stabilize the knee joint, and an injury to this ligament can cause pain, instability, and difficulty with movement.

To perform the Valgus Stress Test, the patient is positioned lying on their back with their leg extended. The healthcare provider then bends the patient’s knee to 30 degrees and places one hand on the lateral side of the knee joint and the other hand on the medial ankle.
The medical person then applies a valgus force (sideways pressure) to the knee joint while simultaneously stabilizing the ankle. If there is an MCL injury present, there will be excessive movement or gapping on the medial side of the knee joint, indicating a positive test result.
The Valgus Stress Test is often performed in conjunction with other diagnostic tests, such as X-rays or MRI, to confirm a diagnosis of an MCL injury. Treatment options for this type of injury may include rest, physical therapy, or surgical intervention.
It is very necessary to take in mind that the Valgus Stress Test should only be performed by a trained healthcare provider and interpreted in conjunction with other diagnostic tests and clinical findings. moreover, this test may cause discomfort or pain for patients with an MCL injury, so it should be performed with caution and care.
The Varus Stress Test is another diagnostic test used to evaluate for the presence of a lateral collateral ligament (LCL) injury in the knee joint. The LCL is one of the major ligaments that helps stabilize the knee joint, and an injury to this ligament can cause pain, instability, and difficulty with movement.
To perform the Varus Stress Test, the patient is positioned lying on their back with their leg extended. The medical person then bends the patient’s knee to 30 degrees and places one hand on the medial side of the knee joint and the other hand on the lateral ankle.
The healthcare provider then applies a varus force (sideways pressure) to the knee joint while simultaneously stabilizing the ankle. If there is an LCL injury present, there will be excessive movement or gapping on the lateral side of the knee joint, indicating a positive test result.
The Varus Stress Test is often performed in conjunction with other diagnostic tests, such as X-rays or MRI, to confirm a diagnosis of an LCL injury. Treatment options for this type of injury may include rest, physical therapy, or surgical intervention.
It is very necessary to take in mind that the Varus Stress Test should only be performed by a trained medical person and interpreted in conjunction with other diagnostic tests and clinical findings. moreover, this test may cause discomfort or pain for patients with an LCL injury, so it should be performed with caution and care.
The Varus Stress Test
The Varus Stress Test is another diagnostic test used to evaluate for the presence of a lateral collateral ligament (LCL) injury in the knee joint. The LCL is one of the major ligaments that helps stabilize the knee joint, and an injury to this ligament can cause pain, instability, and difficulty with movement.
To perform the Varus Stress Test, the patient is positioned lying on their back with their leg extended. The medical person then bends the patient’s knee to 30 degrees and places one hand on the medial side of the knee joint and the other hand on the lateral ankle.
The healthcare provider person then applies a varus force (sideways pressure) to the knee joint while simultaneously stabilizing the ankle. If there is an LCL injury present, there will be excessive movement or gapping on the lateral side of the knee joint, indicating a positive test result.
The Varus Stress Test is often performed in conjunction with other diagnostic tests, such as X-rays or MRI, to confirm a diagnosis of an LCL injury. Treatment options for this type of injury may include rest, physical therapy, or surgical intervention.
It is very necessary to take in mind that the Varus Stress Test should only be performed by a trained medical person and interpreted in conjunction with other diagnostic tests and clinical findings. moreover, this test may cause discomfort or pain for patients with an LCL injury, so it should be performed with caution and care.
Treatment of knee joint ligament
The treatment of knee ligament injuries depends on the severity and type of injury.
- Rest and Physical Therapy: For mild to moderate knee ligament injuries, rest and physical therapy may be recommended. Resting the affected knee and avoiding activities that cause pain or discomfort can help reduce inflammation and promote healing. Physical therapy may include exercises to improve strength, flexibility, and range of motion in the affected knee.
- Bracing: In some cases, a brace or splint may be recommended to provide support and stability to the affected knee. This can be useful in preventing further injury and promoting healing.
- Medications: Over-the-counter pain relievers such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) may be recommended to help manage pain and reduce inflammation.
- Surgery: In severe cases of knee ligament injuries, surgery may be necessary to repair or reconstruct the damaged ligament. This is typically reserved for injuries that do not respond to other treatments or for athletes or individuals who require full knee function for their daily activities.
- Rehabilitation: After surgery or more severe injuries, rehabilitation is an important part of the recovery process. This may include physical therapy, exercises, and stretches to help restore strength, flexibility, and range of motion in the affected knee.
Physiotherapy
Physiotherapy treatment for knee joint ligament injuries may include a combination of exercises, stretches, and other modalities to help reduce pain, inflammation and promote healing. Here are some common physiotherapy treatments for knee joint ligament injuries:
Range of Motion Exercises: These exercises help improve the flexibility and range of motion in the affected knee. Examples include heel slides, knee extensions, and knee flexion exercises.
Strengthening Exercises: Strengthening exercises help improve the strength and stability of the knee joint. Examples include squats, lunges, leg presses, and resistance band exercises.
Balance and Proprioception Exercises: These exercises help improve balance and coordination, which are important for preventing further injury. Examples include single-leg balance exercises, wobble board exercises, and agility drills.
Manual Therapy: This may include massage, joint mobilization, and stretching techniques to help reduce pain and improve mobility in the affected knee.

Modalities: Modalities such as heat therapy, ice therapy, ultrasound, and electrical stimulation may be used to help reduce pain and inflammation in the affected knee.
Bracing: A physiotherapist may recommend a brace or support to provide additional stability and support to the affected knee during activities.
Education: A physiotherapist may provide education on proper body mechanics and movement patterns to help prevent further injury and promote healing.
so in the end, physiotherapy treatment for knee joint ligament injuries is designed to promote healing, reduce pain and inflammation, and improve function and mobility in the affected knee. A physiotherapist will develop a personalized treatment plan based on the individual’s needs and goals for recovery.
Risk factors
Knee ligament injuries can occur due to a variety of risk factors, including:
- Sports Participation: Knee ligament injuries very commonly result in sports that involve changes in direction, sudden stops, and jumping, such as soccer football, and basketball.
- Age and Gender: Older individuals and females are more prone to knee ligament injuries due to decreased muscle strength, joint stability, and hormonal factors.
- Previous Injury: Individuals who have previously injured their knee ligaments are at a higher risk of re-injury.
- Poor Conditioning: Poor physical conditioning, including weak muscles and poor flexibility, can increase the risk of knee ligament injuries.
- Overuse: Repetitive stress on the knee joint from activities such as running or jumping can increase the risk of knee ligament injuries.
- Improper Technique: Poor body mechanics and improper technique during physical activity can increase the risk of knee ligament injuries.
- Environmental Factors: Environmental factors such as uneven terrain or poor playing surfaces can increase the risk of knee ligament injuries.
It is important to identify and address these risk factors to prevent knee ligament injuries and promote overall knee health. This may include proper conditioning, technique training, and the use of appropriate protective gear during physical activity.
How to prevent the knee joint ligament injuries
Preventing knee ligament injuries involves a combination of strategies that address the risk factors mentioned above. Here are some ways to prevent knee ligament injuries:
- Proper Conditioning: Maintaining good physical conditioning, including regular exercise and strength training, can help improve muscle strength and flexibility, which can reduce the risk of knee ligament injuries.
- Warm-Up and Cool-Down: Before engaging in physical activity, it is important to warm up and stretch to prepare the muscles and joints for the activity. Afterward, cooling down and stretching can help prevent muscle soreness and injury.
- Proper Technique: Using proper body mechanics and technique during physical activity can help reduce the stress on the knee joint and prevent knee ligament injuries.
- Use of Protective Gear: Wearing appropriate protective gear such as knee pads or braces during physical activity can help absorb shock and reduce the risk of injury.
- Gradual Progression: When starting a new physical activity or increasing intensity, it is important to progress gradually to allow the body to adapt and reduce the risk of injury.
- Rest and Recovery: Allowing for adequate rest and recovery between physical activities can help prevent overuse injuries and reduce the risk of knee ligament injuries.
- Addressing Environmental Factors: Addressing environmental factors such as uneven terrain or poor playing surfaces can help reduce the risk of knee ligament injuries.
By implementing these strategies, individuals can reduce their risk of knee ligament injuries and promote overall knee health.
FAQs
What are knee ligaments?
Knee ligaments are strong bands of tissue that connect the bones of the knee joint and provide stability to the joint.
What are the very common types of knee ligament injuries?
The most common types of knee ligament injuries are ACL (anterior cruciate ligament), PCL (posterior cruciate ligament), MCL (medial collateral ligament), and LCL (lateral collateral ligament) injuries.
What are the characteristics of a knee ligament injury?
Symptoms of a knee ligament injury may include pain, swelling, stiffness, instability, and difficulty bearing weight on the affected leg.
How are knee ligament injuries diagnosed?
Knee ligament injuries are typically diagnosed through a physical examination, medical history, and imaging tests such as X-rays, MRI, or CT scans.
What is the treatment for knee ligament injuries?
Treatment for knee ligament injuries may include rest, ice, compression, elevation, physical therapy, bracing, and in some cases, surgery.
Can knee ligament injuries be prevented?
Yes, knee ligament injuries can be prevented by maintaining good physical conditioning, using proper technique during physical activity, wearing appropriate protective gear, progressing gradually with new activities, allowing for adequate rest and recovery, and addressing environmental factors.