Limb Length Discrepancy
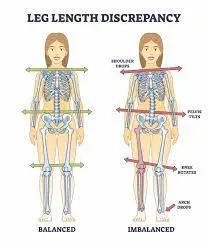
What is Limb Length Discrepancy (LLD)?
What causes Limb Length Discrepancy?
Signs and symptoms of Limb Length Discrepancy
Diagnosis of Limb Length Discrepancy
In most cases, additional imaging studies will be ordered to confirm the diagnosis, establish baseline measurements for both legs and guide treatment recommendations. These may include:
- X-rays: These produce images of the bones. X-rays of the legs are typically taken, but additional X-rays of the hand and hip may also be required to assess skeletal maturity or remaining growth potential.
- EOS imaging: This technology generates 3-dimensional models from two flat images. EOS images are captured while the child is standing upright, enabling improved diagnosis due to weight-bearing positioning.
- Computed tomography (CT) scan: This imaging technique combines X-rays and computer technology to examine bones, producing cross-sectional images (“slices”) of the body.
- Magnetic resonance imaging (MRI): Using strong magnets, radio frequencies, and computer processing, MRI delivers elaborate images of organs, soft tissues, muscles, ligaments, and other formats within the body. MRI poses no radiation disclosure to the child.
Imaging studies and physical examinations may need to be repeated every six to twelve months while your child is still growing. This periodic reassessment is necessary to monitor any changes in the limb-length discrepancy, determining whether it is progressing or remaining stable.
Measurement of Limb Length Discrepancies
Direct Methods
Measuring limb length using a tape measure between two defined points while standing is a common method. Two commonly used points are the anterior iliac spine and the medial malleolus, or the anterior inferior iliac spine and lateral malleolus.
However, it is important to be cautious as there is a significant amount of criticism and debate regarding the accuracy of tape measure methods. If you opt for this method, consider the following topics and potential errors:
- Always take the mean of at least two or three measurements.
- Whenever possible, compare measurements taken by two or more clinicians.
- Iliac asymmetries can either conceal or exaggerate a limb length inequality.
- Unilateral divagations in the elongated axis of the lower extremity, for example, genu varum, can mask or emphasize a limb length inequality.
- The asymmetrical position of the umbilicus can affect measurements.
- Joint contractures can also impact the accuracy of measurements.
Indirect Methods
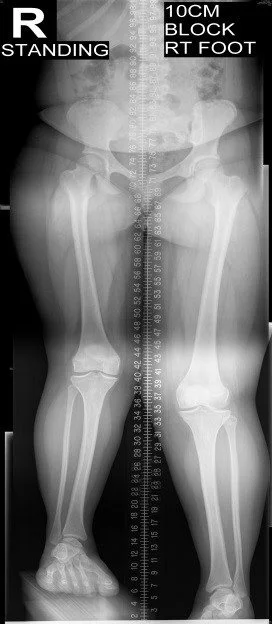
The palpation of bony landmarks, such as the iliac crests or anterior iliac spines, while standing, is commonly used to assess limb length. These methods involve determining if the bony landmarks are at the same level horizontally or if there is a limb length inequality.
Among these processes, the mixture of palpation and illustrated analysis of the iliac crest or anterior superior iliac spine along with the usage of blocks or general-thickness book pages beneath the shorter extremity to adjust the level of the iliac crests (or ASIS) appears to be the most accurate and precise clinical approach for assessing limb inequality.
Regardless, it’s essential to regard that asymmetrical pelvic rotations in planes other than the frontal plane may be related to limb length imbalance. Therefore, it is recommended to palpate and compare multiple pelvic landmarks, including the greater trochanter, when using the block correction method.
To ensure the accuracy and reliability of limb length assessment, it is essential to follow these guidelines and consider the broader literature on the subject
The PALM (Pelvic Limb Alignment Method)
The PALM (Pelvic Limb Alignment Method) is an accurate and reliable tool for measuring pelvic height differences. It offers a convenient and cost-effective alternative to radiographic measurements.
Here is the correct and unique description of the measurement procedure:
- Two tape strips are positioned on the ground, with a separation of 15cm between them. These tape strips serve as markers of where patients should place their feet.
- Patients are instructed to take 10 steps while ensuring that the medial borders of their feet align with the outer edges of the tape strips.
- Patients are required to stand in an upright position with no bending of the knees, hips, or spine.
- The PALM device is then positioned on the most superior element of the iliac crest.
- The distance between the caliper heads is measured, recording the measurement to the nearest millimeter.
- Additionally, the inclinometer ball, which is designed to move towards the side of the shorter limb, is used to measure the angle of inclination. The inclination is documented to the closest half-degree.
By following this procedure, the PALM provides precise measurements of pelvic height differences. It is a reliable method that eliminates the need for radiographic measurements, offering a practical and cost-effective approach to assessing limb length discrepancies.
Measurement Using Blocks
The patient stands with their feet approximately 10 cm apart, knees extended, and equal weight distributed on both feet. The clinician places their hands on bilateral anatomical structures such as the posterior superior iliac spine, anterior superior iliac spine, or left and right iliac crest. The clinician visually assesses for any apparent limb length inequality. If a discrepancy is observed, a wooden board with a thickness of 0.5 cm is placed under the foot of the shorter side.
The process continues by gradually increasing the thickness of the plank under the shorter side until equal limb lengths are achieved. The final thickness of the plank corresponds to the measured leg length difference.
The reliability of this method largely depends on the accurate measurements taken by the clinician. However, studies have shown promising results regarding inter-examiner agreements between highly trained clinicians and medical students. It is important to consider confounding variables that can affect the accuracy of measurements, including pelvic asymmetry, incorrect foot positioning, obesity, joint contractures, scoliosis, and potential measurement errors.
While this method offers a practical approach to assessing limb length inequality, attention to detail and consideration of potential influencing factors are essential for obtaining reliable and accurate results.
How are limb-length discrepancies treated?
Limb-length discrepancies can be addressed through various treatment options, including both surgical and non-surgical approaches. The choice of treatment for your child will depend on several factors, such as their age, overall health, medical history, the affected limbs (legs or arms), the extent of the discrepancy, your child’s tolerance for specific interventions, and your preferences.
Non-surgical treatments for leg-length discrepancies:
- Shoe lifts: Placing lifts inside the shoe of the shorter leg can help equalize leg lengths, improving walking and reducing back pain.
- Physical therapy: Special stretches and exercises can be employed to alleviate pain and enhance overall function.
- Occupational therapy: This therapy focuses on developing fine motor skills, such as handwriting.
- Adaptive devices: Assistive devices can aid your child in performing everyday activities like tying shoes, buttoning shirts, or holding books.
- Prosthetics: Custom-designed prosthetics can be utilized to fit over a shorter limb or replace a limb that has been amputated partially or entirely.
Surgical treatments for limb-length discrepancies:
- Leg-shortening surgery: If the leg-length discrepancy is expected to be moderate (between two and six centimeters) when your child reaches an adult height, the longer leg may be shortened. This procedure slows down the growth of the longer leg, allowing the shorter leg to catch up.
- Epiphysiodesis: The growth plate is fused temporarily or permanently to control the growth in the longer limb.
- Epiphyseal stapling: Staples are surgically inserted on either side of the growth plate. Once the desired length is achieved, the staples are removed.
- Bone resection: A section of bone is surgically removed from the longer leg. This procedure is suitable for adults or adolescents who have reached their adult height.
- Limb-lengthening surgery: This procedure stimulates new bone growth in the shorter leg or arm and is typically reserved for significant limb-length discrepancies that significantly impact daily activities. It is usually performed during late teens or early adulthood.
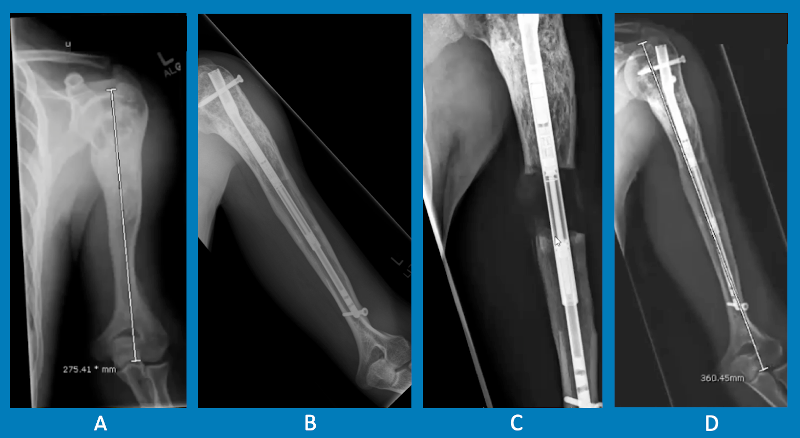
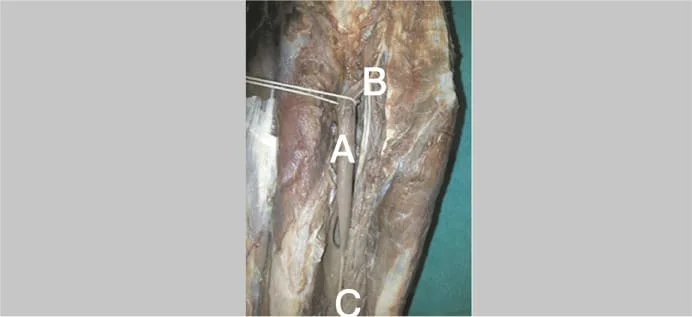
Limb-lengthening surgeries involve a multi-stage process. In the initial stage, an orthopedic surgeon performs an osteotomy, cutting the bone to be lengthened. A lengthening device is then attached, which your child will wear for several months. This device can be external (worn on the outside of the limb) or internal (surgically inserted within the bone).
During the lengthening period, adjustments are made to the device to gradually increase the gap between the bone ends, promoting the growth of new bone. Regular visits to the orthopedic surgeon are necessary to monitor progress and address any potential complications.
The 2 kinds of limb-lengthening instruments are external fixators & internal fixators. External fixators are worn on the outside of the limb, attached to the bone with pins. The device is adjusted by the patient or their family to increase the gap until the desired length is achieved. Once the bone has healed, the device is surgically removed. Internal fixators, such as the PRECICE Nail, are inserted into the bone and gradually expanded using an external magnet, allowing precise lengthening. Like external fixators, internal fixators are removed after lengthening and bone formation.
Left humerus: A. initial to lengthening; B. one year after prior elongation of ~4.5 cm utilizing a precise nail; C. instantly after 2nd elongation of ~4.5 cm; D. 6 months after 2nd elongation.
It’s important to note that the choice of treatment and specific procedures will be determined by your child’s healthcare team based on individualized assessments and discussions with you.
FAQ
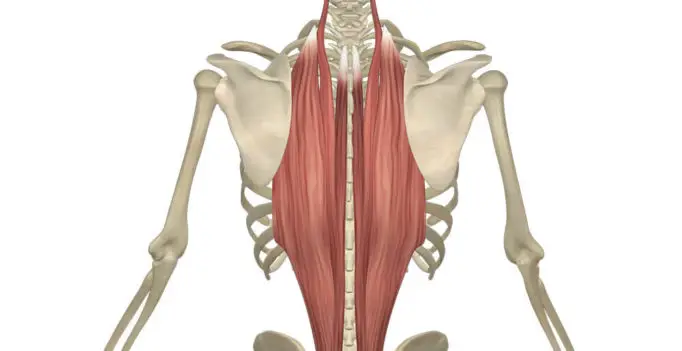
What muscles are affected by leg length discrepancy?
Tight muscles in the abdomen and lower back can laterally tilt the pelvis and hike one side up more elevated than the other side. Tight gluteal muscles & hip rotators can even contribute to one leg emerging to be more elongated than the other leg.
What is the most common cause of leg length discrepancy?
Most patients with unequal leg length are congenital disorders (those individuals are born with them). But further, developed patients may be generated by traumas and illnesses that impair bone maturation plates, inadequately healed bone fractures, and bone tumors, all of which can impact growth and generate one leg to be shorter than the other leg.
What are the two kinds of leg length discrepancies?
There are three kinds of LLD: structural, functional, & environmental. The structural/anatomic kind is because of a contrast in the exact stature of the tibia or femur bone. This may be of congenital, post-trauma, and post-surgery etiology as leg length discrepancy generally happens to obey hip/knee replacement.
What is the best test for leg length discrepancy?
The most normally acknowledged approach for the clinical assessment of leg length discrepancy is the direct way of tape measurement between the bony junctures of the anterior superior iliac spine (ASIS) to the medial/lateral malleolus of the tibia.
What is the limb length ratio?
A ratio of extremity is estimated by separating the forelimb length (humerus length and radius length) by the length of the hindlimb (femur length and tibia length). This ratio is named an intermembral index (“inter” means “between”, & “member” means “limb”).



One Comment