Mallet Finger
Introduction
Mallet finger is also known as “baseball finger,” It is an injury to the narrow tendon that straightens the distal interphalangeal joint of a finger or thumb. This injury can occur to anyone when a stiff object (like a ball) hits the tip of a finger or thumb and forces it to flex further than it is intended to go. As an outcome, you are not able to straighten your fingertip or tip of your thumb actively.
Injuries with mallet finger
The most common injuries associated with mallet finger include:
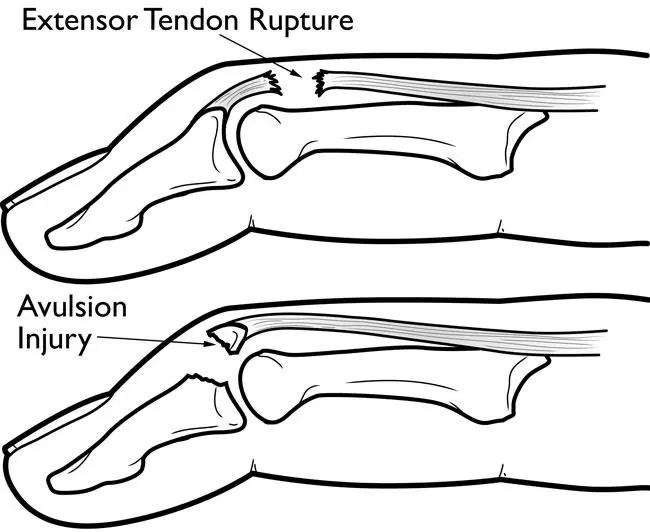
- Torn or ruptured extensor tendon
- Avulsion fracture of distal phalanx
- Joint dislocation of the distal interphalangeal joint(DIP)
Causes of Mallet Finger
- In sports, any immediate hit to your extended fingers from a ball or any stiff object can rupture the tendon that straightens the tip of your finger. This is known as the extensor tendon. Other immediate impacts, even those of lower force, can have the same effect.
- An effective injury to the extensor tendon will control you from straightening your fingertip.
- A tendon is like a rope made up of collagen (protein) fibers that connect your muscles to your bones. An adequate injury to the finger can tear only the soft tissue of the tendon. Or it may pull the tendon out from the fingertip bone (distal phalange). Sometimes a fragment of bone will pull out from the tendon.
- Mallet finger happens the most often trusted source among young men in sports activities. In children, the injury happens more often trusted source from a direct shock, like crushing a finger in a door.
- Even though a tough hit to the tendon is the cause of mallet finger injuries, sometimes a minimal force may injure the soft tissue tendon. Injuries caused by a low impact happen more often trusted source in older women, during activities such as arranging socks or making a bed.
Symptoms of Mallet Finger
Your finger may experience pain after the injury, and your fingertip will droop. You will still be able to operate your hand. Pain is usually associated with a bone fracture.
You may experience the following symptoms:
- Swelling.
- Bruising.
- Redness.
- An inability to straighten your fingertip.
- Tenderness.
- A detached fingernail.
- Redness under the fingernail bed.
Diagnosis of Mallet Finger
After realizing that you’re unable to straighten your finger, your doctor may require an:
- History of injury at the affected finger.
- Physical examination of the affected finger.
- X-ray.
On rare occurrences, supplemental imaging studies such as an ultrasound or MRI may provide further information.
Treatment of Mallet Finger
Treatment for a mallet finger depends on the severity of the injury and the extent of the damage to the tendon. In mild cases, simply immobilizing the affected finger with a splint or brace may be enough to allow the tendon to heal.
To treat the pain and inflammation of a mallet finger instantly:
- Apply ice.
- Elevate your hand by using a pillow so that your fingers are above your heart level.
- Take nonsteroidal anti-inflammatory drugs (NSAIDs)
It is better to consult a doctor as soon as you can. Mallet finger injuries are generally treated without surgery unless the injury is chronic.
Even if you don’t have more pain and your hand still works, it’s better to get treatment as soon as possible. But even postponed treatment with splinting can be successfully Trusted Source.
If a mallet finger is ignored and left without any treatment, your finger can become tough. Or the finger may have more chances to develop a swan neck deformity, where the joint flexes the wrong way.
A mallet finger in children includes additional trouble. The injury may involve the cartilage in the finger that holds bone growth. If it’s untreated, the child’s finger may become little or not grow appropriately.
Splinting
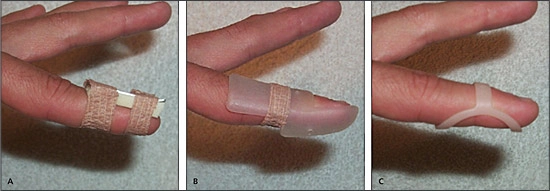
- Splinting is the most useful treatment for a mallet finger. The goal is to uphold the fingertip straight in the splint until the tendon recovers.
- A physiotherapist may prescribe a custom-made splint to immobilize the fingertip and allow the tendon to heal. The splint is usually worn for 6-8 weeks.
- The most frequently used splint is a plastic stack type. Your doctor may guide you to a physical therapist to custom-make a splint for you.
- There are many types of splints available. Some stick to your fingernail. Some may be. None has been established to be a superior Trusted Source to the others.
- Two current studies found that a thermoplastic custom-made splint was less likely Trusted Source to be included in treatment failure, and had a higher rate Trusted Source of compliance.
- You wear the splint when bathing or showering. Afterward, be attentive to keep the finger straightforward on a flat surface while you take off the splint to wash and dry it because if you flex it, you can pull out the tendon again and have to repeat the therapeutic process.
- It’s important to fully obey the splinting routine. If the distal interphalangeal joint is permitted to flex throughout the six weeks, you will have to start the splinting process again.
Exercises
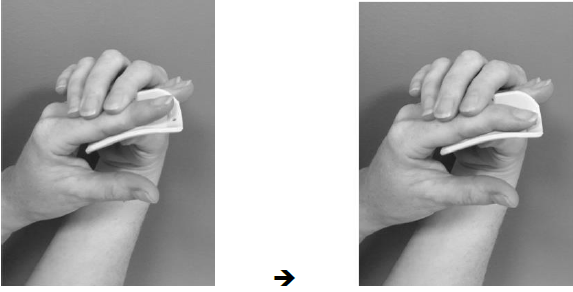

- Finger passive range of motion: Gently flex the injured finger with your other hand. Then kindly try to straighten the injured finger with an asset from your other hand. Repeat gradually, keeping for 5 seconds at the end of individual motion. Do this 10 times. Do these exercises regularly 3 to 5 times per day.
- Fist making: Make your hand into a fist. If the injured finger will not flex into the fist, try to help it with your other hand. Maintain the position for 5 to 10 seconds. Repeat 10 times.
- Object pick-up: Practice gathering up small objects, such as marble, coins, buttons, or pins, with your injured finger and thumb.
- Finger extension: With your palm flat on a surface and your fingers straight, Raise each finger straight up one at a time. Maintain each finger up for 5 seconds and then place it down. Restart until you have done all 5 fingers. Do repeat 10 times.
- Grip strengthening: Squeeze a smooth rubber ball and keep the squeeze for 5 seconds. Do 2 sets of 15.
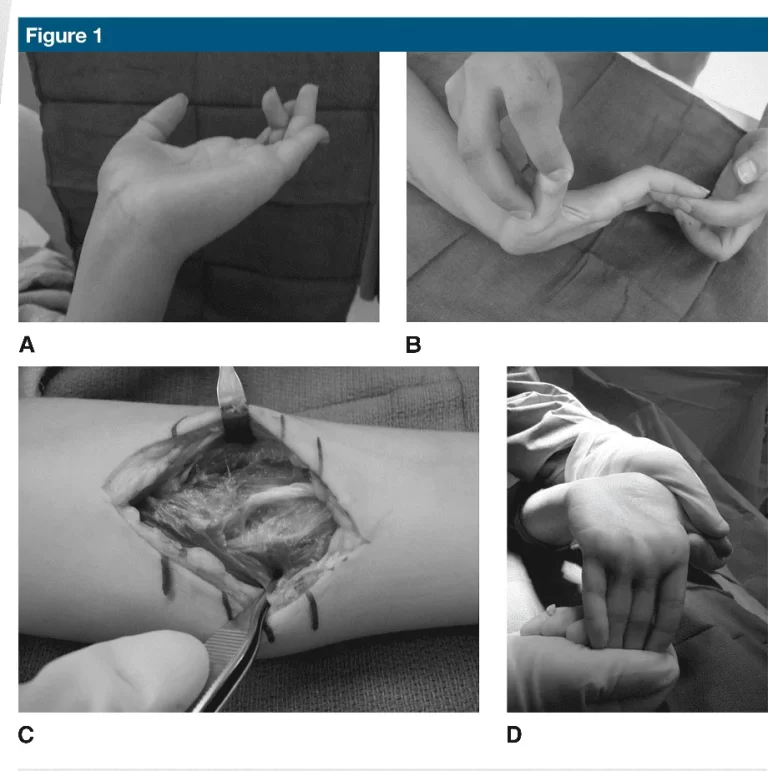
Surgery
Surgery is usually instructed for complex mallet finger injuries. These contain injuries where:
The joint is not properly aligned.
The tendon needs a graft of tendon tissue from somewhere else on your body.
Surgery may be open, where the skin is cut to disclose the tendon, or done with a needle puncture (percutaneous). Hardware will be inserted to hold the fingertip straight until the tendon is cured. Hardware options include:
- pin
- wire
- screw
- plate
In some cases, a suture may be used to correct torn tendons. The hardware is released once the finger has been cured.
At issue is that surgery usually included complications, such as infection, stiffness, or osteoarthritis. A conclusion for open surgery generally is made trusted Source if the benefits of surgery for proper healing overpower the potential risks.
Each individual is different. Discuss with your doctor and a specialist whether surgery is essential for your finger to recover its function.
Conclusion
Mallet finger is a common hand injury. It can cause pain, swelling, and a drooping or bent fingertip. It is caused by a traumatic injury to the fingertip but also be caused by the result of arthritis, genetics, or age. Treatment may include immobilization, surgery, physical therapy, and medications. If you find symptoms of a mallet finger, you must consult a doctor to get proper treatment.
FAQs
Can the mallet finger be corrected?
Yes, a mallet finger can be corrected with non-surgical or surgical treatment. It is depending on the severity of the injury of the mallet finger. Non-surgical treatment involves immobilizing an affected finger by using a splint for 6-8 weeks. surgical treatment may involve repairing the damaged soft tissues, repositioning the affected bones, or fusing the joint in some cases. With treatment, most people who have mallet fingers can recover from this injury.
What tendon is involved in a mallet finger?
The Mallet’s finger involves the extensor tendon of a finger at the DIP joint, which is doing straightens the finger at the distal interphalangeal (DIP) joint. When the extensor tendon is damaged, the fingertip is unable to fully extend, resulting in a deformity known as a mallet finger.
How long does it take for a mallet finger fracture to heal?
Mallet finger should take 6 to 8 weeks to recover, after which time you will be able to use it again. You may be recommended to continue to only wear the splint at night for up to 4 more weeks. In some cases, you may only need to consult a hand physiotherapist who may help to recover your hand function.
Which splint is best for a mallet finger?
There are multiple varieties of splints in the market, but the best splint is an aluminum splint to keep the DIP joint straight. Particularly, the tip of the finger should be maintained straight to let free PIP and MP motions.
What are the complications of a mallet finger?
If left without treatment, a mallet finger can conduct a swan neck deformity from PIP joint hyperextension and DIP joint flexion.




3 Comments