Pseudo-volkman contrcture
What is the Pseudo-Volkmann’s contracture?
Pseudo-Volkman contraction, also known as “Pseudo-Volkman syndrome” or “Pseudo-Volkman ischemic contracture,” is a rare and serious medical condition characterized by the development of muscle contractures in response to prolonged or severe ischemia (lack of blood flow) to a specific area of the body. The term “pseudo” is used to differentiate it from the classic Volkman’s contracture, which results from compartment syndrome.
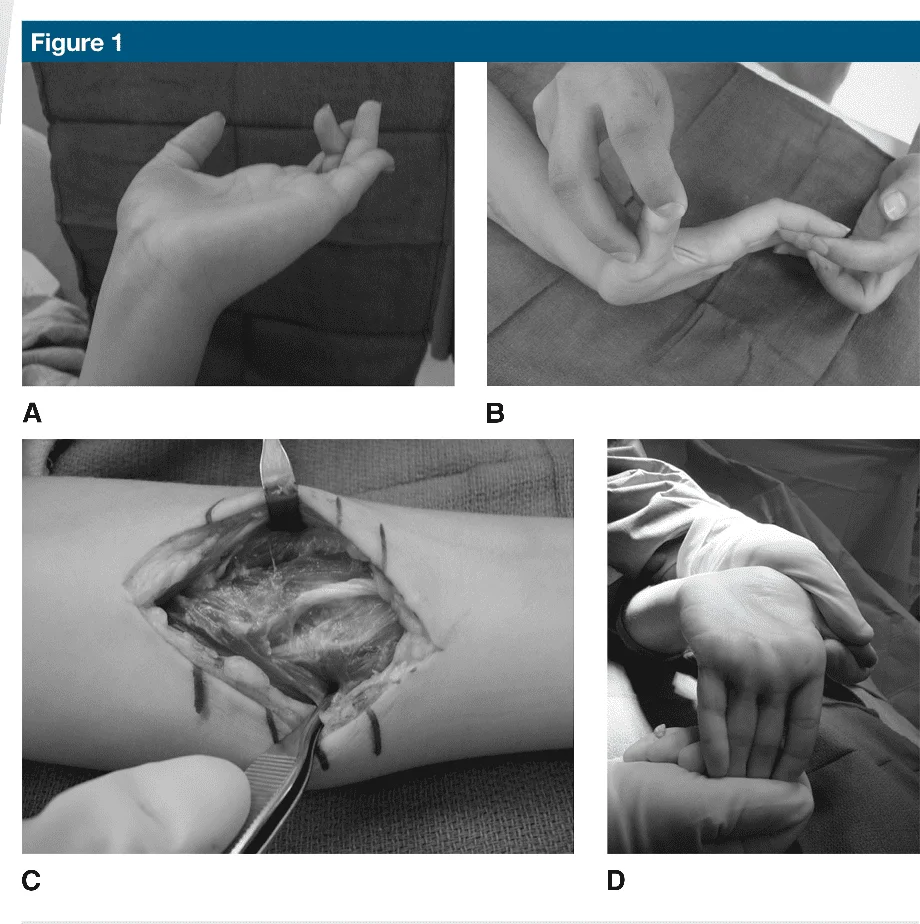
Due to the child’s flexor digitorum profundus muscle being attached to ulna fractures, pseudo-Volkmann’s contracture resulted. Unlike the usual Volkmann contracture as a complication of a pediatric forearm fracture, pseudo-Volkmann contracture is not a sequela of ischemia but rather a mechanical entrapment of the flexor myotendinous units in the fracture or adhesions.
Pseudo-Volkmann contracture is well described but uncommon. It most generally involves the ring finger flexor digitorum superficialis muscle but can happen in all fingers. This entrapment could be identified acutely with an intentional examination by confirming full passive motion of the phalanges (or finger) after the preferred treatment of both-bone forearm fractures in the pediatric patient. When the contracture is recognized on examination, surgical intervention to clear an entrapment from a fracture is effective and produces excellent outcomes.
Pediatric forearm fractures could be complicated by compartment syndrome and Volkmann ischemic contracture. Tsuge classified an ischemic contracture into mild, moderate, and severe. Despite surgical intervention, a patient rarely recovers full function.
In contrast, pseudo-Volkmann contracture, as a complication of pediatric forearm fractures, is not a sequela of ischemia but rather a mechanical entrapment of the flexor myotendinous units in the fracture or adhesions. In pseudo-Volkmann contracture, ischemic clinical findings are absent, such as pain out of proportion at the time of an injury or treatment and no ischemic muscle found at the time of surgical treatment. the clinical findings involve the unable of the fingers extension passively or actively when a wrist is in extension. The patient could fully extension of the fingers when the wrist is flexion. This type of condition has an outstanding prognosis for full recovery if diagnosed and treated early. When treated after a patient develops joint contractures, a good outcome is more problem to achieve.
This phenomenon is reported in the literature utilizing the terminology of entrapment of the flexor muscles and pseudo-Volkmann contracture. The review of the literature reveals these conditions to be equivalent. However the clinical entity is still uncommon, it might be more prevalent than previously thought. Hopefully, this clinical entity will gain improved recognition because diagnosis continues to be delayed, and early intervention outcomes in excellent results.
What is the Treatment of the Pseudo-Volkmann’s contracture?
Physical therapy has not been shown to adequately manage these contractures once established. If the contracture is diagnosed acutely, as with entrapment, then r-manipulation is indicated and might occasionally be successful at resolving entrapment. The success of manipulation declines after 2 weeks. If the full passive motion of the fingers (or phalanges) after remanipulation is not successful. and the surgical release must be performed. Typically, the myotenolysis at an area of adhesion provides recovery of full ROM (range of motion). Occasionally, lengthening the musculotendinous unit assists acquire full motion.
We agree with the recommendations of previous authors that every patient be confirmed to have full painless passive motion of the fingers (or phalanges) and thumb at the time of initial fracture treatment. We also propose that full passive motion be confirmed at seven days and each subsequent appointment. The delay of diagnosis might be specifically detrimental in older patients because patients nearing adulthood might develop contracture of the myotendinous unit or the proximal interphalangeal joints faster and be more difficult to treat with simple myotenolysis.
DISCLAIMER
The materials contained on this website are provided for your general information purposes only and do not constitute legal or/and other professional advice on any subject matter. Physiotherapy Treatment or Technique or Approach does not accept any responsibility for any loss which may arise from reliance on information contained on this site. A few or any actions you take upon the information presented in this article are strictly at your own risk and your responsibility.
FAQs
What is a pseudo-contracture in the central nervous system?
Pseudomyostatic Contracture – a constant state of contraction giving excessive resistance to passive stretching. Associated with hypertonicity of spastic or rigid nature – the central nervous system lesion such as the CVA, spinal cord injury, traumatic brain injury.
Which nerve causes Volkmann’s contracture?
All these muscles are innervated by a median nerve. The exceptions are flexor carpi ulnaris (innervated by the ulnar nerve) and flexor digitorum profundus muscle sharing a dual nerve supply from both ulnar nerves and median nerves. Both these groups are involved in the development of the Volkmann ischemic contracture.
Which artery is involved in Volkmann’s contracture?
The condition might be caused by obstruction on the brachial artery near the elbow, possibly from improper use of a tourniquet, improper use of a plaster cast, or compartment syndrome.
What is the earliest indication of Volkmann’s ischemia?
History and Physical Examination. The clinical presentation of Volkmann contracture includes what is generally referred to as the five Ps: pain, pallor, pulselessness, paresthesias, and paralysis. Of these pain is the earliest sign.
How can you reduce the risk of contractures?
Contractures frequently develop after prolonged bed rest, inactivity, or lack of use of certain muscle groups. To decrease the risk of muscle tightness and to prevent contractures from developing, it is important to move daily and stretch common areas like the fingers, arms, and legs.