Meninges of the Brain and Spinal cord
Introduction
The brain and spinal cord divide from the walls of their bony enclosures or illustrations (the skull and spinal column) by three membranes called meninges. Based on their position, meninges are mentioned as the cranial meninges which cover the brain, and spinal meninges which protect the spinal cord. Notwithstanding the fact that they share the same three meningeal layers and are continuous, the cranial and spinal meninges.
The meninges are listed as follows, in order of depth:
- Dura mater
- Arachnoid mater
- Pia mater
The epidural, subdural, and subarachnoid spaces are three clinically important potential regions that are surrounded by these layers. The meninges have three main purposes: to aid the flow of blood, protect the brain and spinal cord from mechanical trauma, and provide a continuous canal through which the cerebrospinal fluid (CSF) flows. The CSF particularly travels between the leptomeninges, which are made up of the mixed arachnoid and pia meningeal layers.
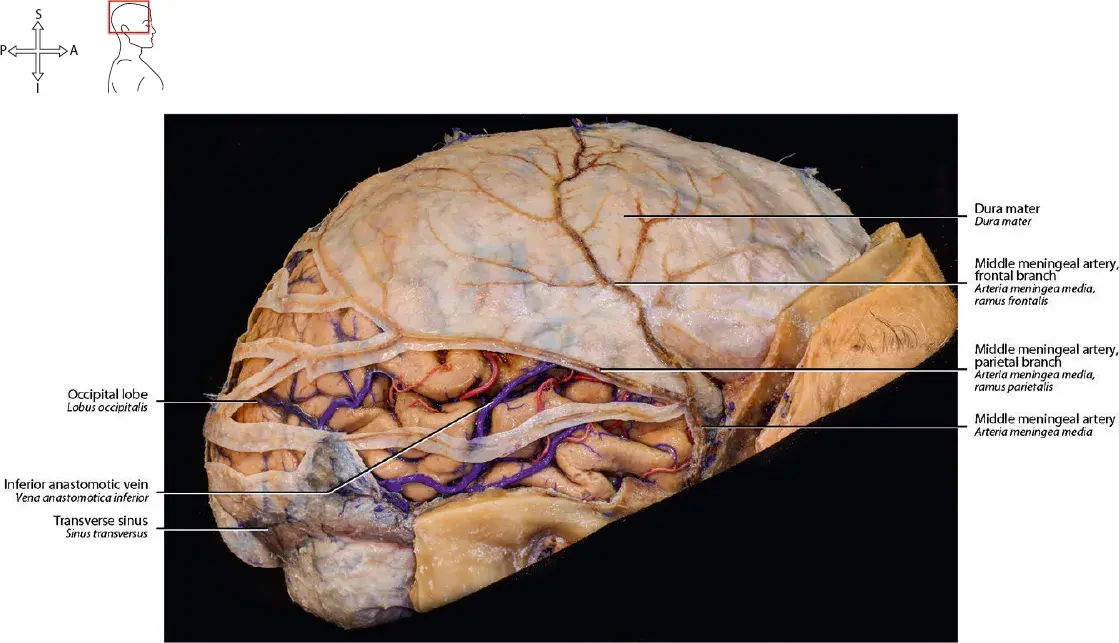
Dura mater
The superficial layer or coating is the periosteal cranial dura. It overlaps the inner table of the cranial vault bones and works as the periosteal layer or coating of the cranium.
- The meningeal cranial dura, which situated superficial to the arachnoid mater.
- The two dural layers are firmly attached or fixed to each other, except in places where they separate to surround the dural venous sinuses.
- The fibrous septa that partially divide the brain cavity develop when the meningeal barrier predicts inward, towards the cerebral tissue.
- The fibrous septa within the cranium are the: Falx cerebri, the largest or most substantial of fibrous septa. It extends across the midline on the inner region of the calvaria, from crista galli to the internal occipital protuberance.
- It divides the left and right cerebral hemispheres and residence the superior sagittal and inferior sagittal sinuses. Posteriorly, the falx mix with tentorium cerebelli.
- Tentorium cerebelli, which range in a transverse plane from the inner region of the occipital bone.
- It divides the cerebrum from the cerebellum and comprises the transverse, straight, and superior petrosal sinuses. The forebrain and hindbrain are separated by the tentorium into supratentorial or infratentorial divisions, respectively. Falx cerebelli, which predicts from the midline of the occipital bone.
- It divides the hemispheres of the cerebellum and the residence of the occipital sinus. Diaphragma sellae is a flat membrane that adjoins the pituitary stalk and forms the roof over the hypophyseal fossa.
- It accommodates the anterior and the posterior intercavernous sinuses.
- The meningeal dura mater overlaps the trigeminal ganglion and surrounds it in a compartment known as the trigeminal cave (Meckel’s cave).
Arachnoid mater
- The cranial arachnoid mater is a cobweb-like meningeal layer or coating, that interferes with the dura and pia mater. Some authors claim that the subdural space—a possible space between the arachnoid and dura—contains a very thin fluid layer or coating. Cerebrospinal fluid (CSF) is present in the subarachnoid space, which is the region between the arachnoid and pia mater. in addition, all cerebral arteries and veins are situated in this space.
- Cerebrospinal fluid (CSF) leakage into the subdural space is prevented or limited by the outer area of the arachnoid’s attachment to the dura mater. The arachnoid mater exhibits projections that resemble mushrooms termed arachnoid granulations at the locations where the dura mater creates the venous sinuses. The inner area of the arachnoid shows a thin fibrous projection called the arachnoid trabeculae that transfer the subarachnoid space and gets attached to the outer surface of the pia mater. Leptomeninges is a collective term for the pia mater and arachnoid because of their embryological and cellular similarity.
- The arachnoid granulations are projections of the arachnoid mater that penetrate the meningeal dura and predict the lumina of the dural venous sinuses. The center of each arachnoid granulation is continuous with the subarachnoid space, therefore, comprising the cerebrospinal fluid (CSF).
- The CSF spread through the lining of the arachnoid granulations into the dural venous sinuses. The cerebrospinal fluid (CSF) can thus continuously drain from the subarachnoid space into the vascular system thanks to the arachnoid granulations. It is very important that the cerebrospinal fluid (CSF) drainage is held in balance with the manufacture of new cerebrospinal fluid (CSF) from the choroid plexus, permitting a continuous amount of the cerebrospinal fluid (CSF) in the brain (normally about 150 milliliters). Since the skull is an inflexible case, any increase in the quantity of cerebrospinal fluid (CSF) in the brain elevates the intracranial pressure and can cause different neurological disorders (e.g. hydrocephalus)
subarachnoid cisterns
The arachnoid mater does not observe precisely the contours of the brain. Moreover, in some sites, it completely separates from the pia mater, thus forming the expansions of the subarachnoid termed, the subarachnoid cisterns. There are ten major subarachnoid cisterns of the brain that are constant with each other via the general subarachnoid space. These include the:
- Cerebellopontine cistern
- Interpeduncular cistern
- Pontine cistern
- Cisterna magna (cerebellomedullary cistern)
- Chiasmatic cistern
- Quadrigeminal cistern
- Ambient cistern
- Crural and carotid cisterns
- Cistern of lateral cerebral fossa (Sylvian cistern)
- Cistern of lamina terminalis
Pia mater
The cranial pia mater is an extremely vascular membrane that closely follows the shape of the brain. It doesn’t present on the surface of the brain directly but rather is detached from it by a thin gap called the subpial space formed by the end-feet of the astrocytes (glia limitans). numerous superficial blood vessels of the brain are connected to the pia mater. However, given that it is a very thin membrane, these blood vessels are partially implanted within the thickness of the pia, while partially suspended or drooping by the arachnoid trabeculae.
The brain and spinal cord are distinguished from the walls within their bony casings or representations (the skull and spinal column) by three coverings called meninges.
Spinal meninges
Spinal dura mater
The dura mater of the spinal cord part from that of the brain by having only one layer or coating; the meningeal layer. Although the spinal canal possesses its own, real periosteum, opposite the skull, the outermost layer of bone is absent. The spinal dura mater gets attaches to the tectorial membrane & posterior longitudinal ligament superiorly. Inferiorly, it expands up to S2 (sacral) vertebral level, thus expanding below the spinal cord termination (L1/L2).
The epidural cavity is the region between the spinal dura mater and the cartilage of the vertebral column. It runs over the anterior and posterior internal vertebral venous plexuses and is packed with loose connective and adipose tissues.
Spinal pia mater
The spinal pia mater continues onto the cranial pia mater at the region of the foramen magnum. It closely covers the spinal cord and comprises a vascular plexus for the spinal cord tissue. The pia mater produces a fibrous protuberance that’s called the filum terminale from the apex (tip) of the conus medullaris. The filum terminale runs downhill about 20 centimetres until reaching the first coccygeal vertebra’s periosteum.
Starting from the region of the foramen magnum to the region of vertebra T12(thoracic vertebrae), the spinal pia shows 21 pairs of ligamentous lateral predictions that pass via the arachnoid and gets attached to the spinal dura mater. These predictions are termed the denticulate ligamentsThe successive pairs of spinal neurons are placed halfway apart by every pair of denticulate ligaments. The function of denticulate ligaments is to position and stabilize the spinal cord in place.
Meningeal spaces
The meningeal space is the gap between the meningeal layers. There are three clinically remarkable meningeal spaces; epidural, subdural, and subarachnoid.
Epidural space
epidural space is a prospective space between the superficial layer of the dura mater and the calvarium. On another side, the spinal epidural space is present in between the spinal dura mater and the tissues that line the vertebral canal.
The spinal epidural space is a region for applying local epidural anesthesia. The procedure may be performed at any vertebral region and the choice relies on the body area that is preferred to be anesthetized for an upcoming surgical/obstetric procedure. The applied anesthetics (e.g. lidocaine) anesthetize the local spinal nerve rootlets following analgesia (pain relief).
Subdural space
subdural space is a prospective space between the dura mater and the beneath the arachnoid mater. The spinal subdural space is sustained with the cranial subdural space. Both are extremely narrow or tiny, and they probably have a thin film of fluid inside.
Subarachnoid space
The space in between the arachnoid mater and the pia mater is termed the subarachnoid space. The subarachnoid space comprises cerebrospinal fluid (CSF) and major blood vessels and gives expansions known as cisterns. The subarachnoid spaces of the cranium and vertebral column are ongoing with each other, creating a closed route for the cerebrospinal fluid(CSF) circulation.
The CSF is made by the cells of the choroid plexus within the walls of the brain ventricles. The fluid conveys from the lateral to the third ventricle, and then it passes to the fourth ventricle.
From the fourth ventricle, the cerebrospinal fluid (CSF) passes into the central canal of the spinal cord and into the interpeduncular and quadrigeminal subarachnoid cisterns.
The cerebrospinal fluid (CSF) then extends the subarachnoid space of the brain and spinal cord, circulating via them.
Finally, the CSF is reabsorbed into the dural venous sinuses by diffusing or spreading through the subarachnoid granulations in the cranial subarachnoid space.
Clinical relations
Meningitis.
Your meninges are infected, according to this. Bacteria, fungi, or viruses are all potential culprits for the infection. Typically, a lumbar puncture to get a sample of cerebrospinal fluid is necessary to diagnose this illness. Meningitis can very rarely result from non-infectious causes such as cancer, inflammatory conditions, brain surgery, or specific medications.
Epidural bleeding
age is an uncommon condition caused by the rupture or break of one of the meningeal vessels. Usually, one of the dural venous sinuses or the middle meningeal artery serves as the source or origin of bleeding. Epidural bleeding normally occurs due to a fracture of the parietal-temporal area of the skull which frequently causes a rupture or breaks of the previously mention blood vessels. The hemorrhage divided the periosteal dura mater from the skull, forming the epidural hematoma between the calvaria (dome of the skull) and the dura mater.
Since the periosteal dura becomes more tightly coupled to the Diplo, epidural hemorrhage typically affects younger people. The epidural hematoma is examined with CT, on which it is detected as a biconvex hyperdense formation. Normally, a solid connection of the dura mater to the cranial sutures, restricting the bleeding, causes the bilateral convex shape. If treated surgically and on time, the individual normally recovers fully within a couple of days.
Subdural bleeding
Subdural hemorrhage mentions to the process of receiving blood within the subdural space, between the dura and arachnoid mater. It is typically brought on by a head trauma that breaks the bridging veins that link the brain’s surface veins with its dural venous sinuses. The subdural hematoma is normally situated in the convexities of the skull. They are normally diagnosed by head CT, in which they are encountered as high-density semicircular-shaped formations. Subdural hematomas are divided into two types acute and chronic, relying on the timeframe of their formation.
Acute subdural hematoma is mainly caused by a very strong force that tears the bridging veins, has developing growth, and is frequently associated with underlying brain injury. If it’s compressing or constricting the brain it is surgically treated by evacuation or clearance. Small asymptomatic cases, however, may be treated actively.
A chronic subdural hematoma can occur from even a negligible or weak trauma of the head. It normally occurs in the elderly. Additional risk factors include epilepsy, alcoholism, cerebrospinal fluid (CSF) shunts, coagulopathies, and patients who are at risk for falling (such as the elderly). hemiparesis from a stroke). The patients often don’t even remember any trauma or injury that might have caused the subdural bleeding, as it normally happens during falls which they don’t consider as significant. The chronic subdural bleeding and the development of the hematoma are quite slow. Only once the hematoma reaches a crucial size and starts squeezing the underlying brain tissue do symptoms start to appear. Chronic subdural bleeding is diagnosed normally with a CT, on which it appears as a semi-circular-shaped formation with a fibrous capsule. The treatment is the same as for the acute phase of the subdural hematoma, i.e. neurosurgical procedure.
Subarachnoid bleeding
Subarachnoid hemorrhage (SAH) is common post-traumatic bleeding. observe that it can also be non-traumatic, interrelated to the rupture or break of an intracranial aneurysm or arterial malformation.
The key symptom of this condition is a sudden or abrupt onset of a headache which patients describe or represent as the worst they’ve ever had in their life. Other symptoms include deterioration or worsening of consciousness (confusion, stupor, or even coma) and positive meningeal signs. It is diagnosed with classical angiography, Angio-CT, or lumbar puncture. The treatment is oriented or positioned toward three key principles;
Support of vital functions – heart rate and breathing.
Treating the cause of bleeding – neurosurgical closing of the ruptured or broken blood vessel.
Avoiding vasospasm due to the humiliation of the blood and reflexive vasoconstriction.
Physiotherapy Relevance
In the central nervous system (CNS), the meninges serve as a protective layer, and when they sustain damage, significant diseases can develop. Including:
Bacterial Meningitis
Meningitis is a dangerous or risky condition that causes inflammation of the meninges. Meningitis is typically precipitated or occasioned by an infection of the cerebrospinal fluid (CSF).
Hematomas:
Blood can collect in brain cavities and develop hematomas in the brain tissue when blood arteries in the brain are damaged or injured. Brain hematomas can harm or hurt the tissue by causing swelling and inflammation. These consist of:
Extradural hematoma
A medical emergency where blood builds up in the epidural space as a result of blood spilling from the middle meningeal artery, compressing the dura mater and the brain. If an epidural hematoma extends rapidly the injury is potentially fatal.
Subdural hematoma is an accumulation of blood in the space between the outer layer (dura) and the arachnoid mater. It is most frequently caused by torn, bleeding veins on the inside of the dura as a result of a blow to the head. This bleeding can be slow and gradual or rapid, with the latter being a medical emergency.
The collection or merging of blood brought on by bleeding in the subarachnoid space is known as a subarachnoid hematoma. This can get arise due to trauma or can take place due to spontaneous ruptures at weak points in vessels. This condition is frequently associated with cases of a brain aneurysm, in which a cerebral artery balloons or even bursts or ruptures due to structural insufficiency.
Meningioma:
tumor of meninges and meningeal cells, which is common in middle-aged women and may take place in a background of neurofibromatosis type 2. Metastases, florid mitotic activity, and bone degradation are signs of aggressive meningiomas.
FAQ
Which of the meninges is the strongest?
The dura mater is the strongest or most powerful of the three layers, with some animal studies manifesting that the thickness of the dura decreases as it descends(goes down) towards the coccyx.
What would happen if we didn’t have meninges?
The brain is soft and pulpy and without structural support, it would not be able to sustain its normal shape.
What do meninges protect the brain from?
trauma injury
The meninges serve as a shock absorber for the central nervous system (CNS) and shield it from severe brain injury, such as a head injury. They hold the CNS in place and prevent the brain from shifting inside the skull.
What do meninges protect the brain from?
trauma injury
The meninges serve as a shock absorber for the central nervous system (CNS) and shield it from severe brain injury, such as a head injury. They present the CNS and keep the brain from moving around within the skull
What happens if the meninges is damaged?
Meningeal damage or injury can result in cell death in the underlying brain areas. Meningeal damage or injury can cause meningitis, hematoma, etc.
Can the meninges feel pain?
there is an absence of pain receptors in the brain itself. But the meninges (outer coverings of the brain), periosteum (outer coverings of the bones), and the scalp or skull all have pain receptors. Surgery can be done on the brain and mechanically the brain does not feel that pain.
Do the meninges have a blood supply?
The blood supply of the meninges normally concerns or analyses the blood supply of the outer layer of the dura mater rather than the inner layer of the dura mater, arachnoid, or pia mater which do not need a large blood supply. The front, middle, and posterior cranial fossae all have separate arteries supplying the dura mater.
What causes damage to the meninges?
Inflammation of the protective membranes covering the brain and spinal cord, altogether known as the meninges, may develop in response to a number of causes, most apparently bacteria and viruses, but also fungi, parasites, radiation, or neoplasm.
What do meninges attach to?
The brain and spinal cord are separated from the walls of their bony casings (the skull and vertebral column) by three membranes called meninges. Based on their area, meninges are mentioned as the cranial meninges which envelope or cover the brain, and spinal meninges which envelope or cover the spinal cord.
What are meninges made of?
Meninges are formed by or made up of three tissue membranes that are primarily known as the covering of the brain. They are made up of the pia mater, the arachnoid mater, and the dura mater. The outer membrane, known as the dura mater or pachymeninx (patchy-thick), creates a sac that encloses the other meningeal layers.
Does meninges have a blood-brain barrier?
The meninges occupies the space between the skull and the brain parenchyma’s glial limitans, the outer layer of the blood–brain barrier (BBB).
What are spinal meninges?
Three layers of tissue known as the meninges surround the spinal cord and the brain. The spinal meninges, which extend from the brainstem to the filum terminale, specifically encase the spinal cord. The pia mater, arachnoid mater, and dura mater are the meninges’ layers, going from deep to thin.