Meningitis
What is meningitis?
- Meningitis is an inflammation of the fluid and three MENINGES surrounding your brain &spinal cord.
- The most common causes of meningitis are viral & bacterial infections. Other causes may include:
- cancer
- fungi
- drug-induced reactions
- Some viral and bacterial meningitis are contagious. They can be spread by coughing, sneezing, or close contact.
What are the types of meningitis?
- Viral & bacterial infections are the most general causes of meningitis. There are several other forms of meningitis. for example- cryptococcal, which is caused by a fungal infection, &carcinomatous, which is cancer-related. These types are less common.
Viral meningitis
- Viral meningitis is the most general type of meningitis. Viruses in the picornavirus category cause about 52 % of cases in adults & 58 % of cases in infants. These are more common during the summer & fall, & they include:
- coxsackievirus A
- coxsackievirus B
- echoviruses
- Viruses in the Enterovirus category cause about 10 to 15 million infections trusted Source per year, but only a small percentage of people get infected & develop meningitis.
Other viruses can cause meningitis. These include:
- West Nile virus
- influenza
- mumps
- HIV
- measles
- herpes viruses
- Coltivirus, which causes Colorado tick fever
- Viral meningitis typically goes away without treatment. However, some causes do require to be treated.
Bacterial meningitis
- Bacterial meningitis is contagious & caused by infection from some bacteria. It can be destructive if left untreated. About 1 in 10 people trusted Sources who get bacterial meningitis die, & 1 in 5 Trusted Sources have serious complications. This can be true even with retreatment.
- The most common types of bacteria that cause bacterial meningitis to add:
- Streptococcus pneumonia, which is typically found in the respiratory tract, sinuses, & nasal cavity & can cause what’s called “pneumococcal meningitis”
- Neisseria meningitides, which is spread through saliva & other respiratory fluids & causes what’s called “meningococcal meningitis”
- Listeria monocytogenes, which are foodborne bacteria
- Staphylococcus aureus, which is typically found all over the skin & in the nasal passages, & causes “staphylococcal meningitis”
Fungal meningitis
- Fungal meningitis is a rare type of meningitis. It’s caused by a fungus that infects your body & then is transmitted from your bloodstream to your brain or spinal cord.
- Persons with a weakened immune system are more likely to develop fungal meningitis. This includes people with cancer or HIV.
The most common funguses related to fungal meningitis are:
- Cryptococcus is inhaled from dirt or soil that is contaminated with bird droppings, especially pigeons and chickens or destroys vegetation.
- Blastomyces is another type of fungus found in soil, particularly in the Midwestern United States.
- Histoplasma is present in environments that are heavily contaminated with bat & bird droppings, especially in the Midwestern States near the Ohio & Mississippi Rivers.
- Coccidioides, which are present in the soil in specific areas of the U.S. Southwest & South & Central America.
Parasitic meningitis
- This type of meningitis is not much more common than viral or bacterial meningitis, and it’s caused by parasites that are found in dirt, feces, & on some animals & food, like snails, raw fish, chicken, or produce.
One type of parasitic meningitis is more uncommon than others. It’s called eosinophilic meningitis (EM). Three main parasites are responsible for EM. These include:
- Angiostrongylus cantonensis
- Baylisascaris procyonis
- Gnathostoma spinigerum
- Parasitic meningitis is not spread from person to person. , these parasites infect an animal or hide out in food that a human then eats. If the parasite or parasite eggs are infectious when they’re ingested, an infection can occur.
- One very uncommon type of parasitic meningitis, amebic meningitis, is a hazardous type of infection. This type is caused when one of several types of ameba enters the body across the nose while you swim in contaminated lakes, rivers, or ponds. The parasite can destroy brain tissue & may eventually cause hallucinations, seizures, & other serious symptoms. The frequently recognized species is Naegleria fowleri.
Non-infectious meningitis
- Non-infectious meningitis is not an infection. rather than, it is a type of meningitis that’s caused by other medical conditions or management. These include:
- lupus
- a head injury
- brain surgery
- cancer
- certain medications
- Chronic meningitis
- This classification is given to cases of meningitis that are more durable than 4 weeks.
- The etiology of chronic meningitis can be fungi, rheumatological conditions, & cancer, among others. management for chronic meningitis is directed at treating the cause (i.e., managing rheumatoid arthritis).
What are the causes of meningitis?
- Each type of meningitis has a slightly different cause, but each eventually acts in the same way: A bacterium, fungus, virus, or parasite transmitted through the body (via the bloodstream, nerve endings, or even a potential reactivation in the nervous system) until it reaches the brain or spinal cord. There, it sets up in the lining or fluids around these vital body parts & starts developing into a more advanced infection.
- Non-infectious meningitis is the result of a physical injury or another condition; it does not involve an infection.
What are the symptoms of meningitis?
- The symptoms of viral & bacterial meningitis can be similar in the beginning. still, bacterial meningitis symptoms are generally more severe. The symptoms also alter depending on age.
Viral meningitis symptoms
Viral meningitis in infants may cause:
- decreased appetite
- irritability
- vomiting
- diarrhea
- rash
- respiratory symptoms
In adults, viral meningitis may cause:
- headaches
- fever
- stiff neck
- seizures
- sensitivity to bright light
- sleepiness
- lethargy
- nausea & vomiting
- decreased appetite
- altered mental state
Bacterial meningitis symptoms
Bacterial meningitis symptoms develop suddenly. They may include:
- altered mental status
- nausea
- vomiting
- sensitivity to light
- irritability
- headache
- fever
- chills
- stiff neck
- purple areas of skin that resemble bruises
- sleepiness
- lethargy
- pursue immediate medical attention if you are experiencing these symptoms. Bacterial & viral meningitis can be deadly. There is no way to know if you have any bacterial or viral meningitis just by judging your feelings. Your doctor has to perform the tests to determine which type you have.
Fungal meningitis symptoms
Symptoms of fungal meningitis are similar to the other types of this infection. These may include:
- nausea
- vomiting
- sensitivity to light
- neck stiffness
- fever
- headache
- a general sense of being unwell
- confusion or disorientation
- Chronic meningitis symptoms
- You’re diagnosed with chronic meningitis when the symptoms last for longer than 4 weeks.
The symptoms of chronic meningitis are similar to other forms of acute meningitis, but sometimes it can develop slower.
Meningitis rash
- One of the later signs that one bacterial cause of meningitis, Neisseria meningitides, is in your bloodstream is a faint rash on your skin.
- The bacteria from a meningococcal meningitis infection reproduce in your blood & target cells around the capillariesTrusted Source. Damage to these cells leads to capillary damage & light blood leaks. here it shows up as a faint pink, red, or purple rash. The spots may resemble tiny pinpricks & are easily mistaken as a bruise.
- As the infection worsens & spreads, the rash can become more obvious. The spots will grow darker & larger.
- People with dark skin may have a harder time seeing a meningitis rash. Lighter areas of skin, such as the palms of hands & the inside of the mouth, may show signs of a rash more easily.
Is there a vaccine for meningitis?
- Yes, there is a vaccine for some types of bacterial meningitis. Meningococcal meningitis, caused by Neisseria meningitides, is one category for which vaccines are available. While viral meningitis is more common, bacterial meningitis can be more dangerous if it’s not diagnosed and treated rapidly.
For that reason, the two primary vaccines for meningitis are for bacterial sources:
- The meningococcal conjugate or MenACWY vaccine (often called by brand names such as Menactra, Menveo, & MenQuadfi) features a vaccine that targets four of the most common types of bacterial serotypes. It lasts longer & offers greater protection, especially if you maintain booster shots.
- The Serogroup B meningococcal, or MenB, vaccine targets one specific strain, & its protection window is much shorter. Only definite populations are recommended to get this vaccine.
Side effects of a meningitis vaccine can include trusted Source:
- soreness, redness, & burning at the injection site.
- low-grade pyrexia for a day or two following the injection
- chills
- headache
- joint pain
- fatigue
- These side effects should reduce in 3-7 days.
Who should get the MenACWY vaccine?
- The CDC recommends trusted Sources of the MenACWY vaccine for:
- Children ages 11 to 12 years old, with an immunization dose at 16 years old
- All children & adults who may be at an increased risk of meningococcal disease
- Who should get the MenB vaccine?
- The CDC recommends that anyone 10 years old or older who is at more risk for meningococcal disease get the MenB vaccine.
Special conditions
- While most younger children & adults do not need a meningitis vaccine, the CDC recommends trusted Sources for the following conditions:
- certain medical conditions
- particular who work with bacteria for their job
- arrange travel to areas where meningitis is common
- anyone who has more risk of infection due to an outbreak of meningococcal disease
- consult your doctor about the proper time to have your child vaccinated for meningitis, as well as yourself if you fall into any of the categories above.
How contagious is meningitis?
- Some types of meningitis are not contagious. Fungal, parasitic, & non-infectious meningitis is not infectious.
- Viral meningitis is infectious. It’s transmitted through direct contact with body fluids, including mucus, feces, and saliva. Droplets of infected fluid can be spread & shared with sneezing & coughing. You do not have to come into direct contact with an infected person to hoist this infection.
- Bacterial meningitis, the most serious form of meningitis, can also be infectious, especially if it’s meningococcal meningitis. It’s transmitted through prolonged time contact with an infected person. Schools, daycare centers, military barracks, hospitals, & college dorms are prime locations for sharing this infection.
- Some types of meningitis are transmitted through person-to-person contact, but not all.
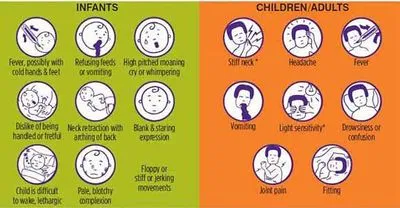
Meningitis in infants:
Babies who develop meningitis may show different signs & symptoms of infection than adults. These symptoms can include:
- pyrexia
- body or neck stiffness
- high-pitched crying
- inconsolable behaviors
- sleepy and difficulty waking
- irritable and grumpy
- does not feel well & has a weak suck during breastfeeding
- Viral meningitis can be common in infants. It can develop as a result of untreated colds, cold sores, flu, & diarrhea. The viruses that lead to these common conditions also cause viral meningitis.
- Bacterial meningitis, which is common but life-threatening, is most likely transmitted from a serious infection in a nearby area of the body. For example, the bacteria from a severe ear infection or sinus infection can enter the bloodstream & find their way to the brain or spinal cord & cause a larger infection.
Meningitis in children
Meningitis becomes more common in children as they grow older & reach high school & college ages. Symptoms of viral & bacterial meningitis in children are similar to symptoms in adults. These include:
- sudden fever
- body & neck aches
- confusion or disorientation
- nausea
- vomiting
- tiredness or fatigue
- Meningitis in adults
- The risk for several forms of meningitis decreases after young adulthood. That’s in large part due to changing circumstances. Schools & college dorms are common sites where some forms of meningitis can be easily shared. Once a young adult ages out of these settings, the likelihood of infection begins to fall.
- However, older individuals who are living with underlying diseases or health conditions that weaken the immune systems can be at greater risk — especially older adults who reside in assisted living facilities, where infections can transmit rapidly.
- Teachers, healthcare professionals, and daycare staffers are also at a higher risk.
How is meningitis diagnosed?
Diagnosing meningitis starts with a health history & physical examination. Age, dorm residence, & daycare center attendance can be important clues. During the physical examination, the doctor will check the :
- fever
- skin issues
- increased heart rate
- neck stiffness
- reduced consciousness
- Your doctor will also order a lumbar puncture. This test is also named a spinal tap. It allows your doctor to analyze the cerebral spinal fluid, which contains a number of indications regarding an infection. Some of the indications in the cerebral spinal fluid can be glucose, white blood cell count, & red blood cell count. This test can also help to decide the best antibiotic for treatment.
Other tests may also be conducted to diagnose meningitis. Common tests include the following:
- Blood cultures identify bacteria in the blood. Bacteria can spread from the blood to the brain. N. meningitides & S. pneumonia, as well as, can cause both sepsis & meningitis.
- A complete blood count with different is a general index of health. It checks the number of red & white blood cells in your blood. White blood cells fight infection. The count is usually increased in meningitis.
- Chest X-rays can give out the presence of pneumonia, tuberculosis, or fungal infections. Meningitis can occur after pneumonia.
- A CT scan of the head may show problems like a brain abscess or intracranial pressure. Bacteria can be transmitted from the sinuses to the meninges.
What is the differential diagnosis of meningitis?
- Stroke
- Subdural hematoma
- Subarachnoid hemorrhage
- Metastatic brain disease
- Brain abscess (might coexist with meningitis).
What are the complications of meningitis?
These complications are typically associated with meningitis:
- seizures
- hearing loss
- vision loss
- memory problems
- migraine headaches
- brain damage
- hydrocephalus
- a subdural empyema, or a buildup of fluid between the brain & the skull
- A meningitis infection may construct bacteria in the bloodstream. These bacteria multiply & some release toxins. That can lead to blood vessel damage & leaking of blood into the skin & organs.
- An extreme form of this blood infection can be life-threatening. Gangrene may damage skin & tissue. In rare cases, amputation may be necessary. Some other severe complications may occur in people with meningitis who are not treated properly.
Meningitis & pneumonia
- Pneumococcal meningitis is a rare but serious & life-threatening form of bacterial meningitis. while the treatment, about 1 in 20 people with this type of infection die.
- About 40 percent of people carry bacteria called Streptococcus pneumonia in their throat & the back of the nose. These bacteria lead to common infections like pneumonia, sinus infections, and ear infections.
- From time to time, however, those bacteria manage to cross the blood-brain barrier & cause inflammation & infection in the brain, spinal cord, or fluids immediately surrounding them.
Symptoms of this serious form of meningitis are:
- chills
- high fever
- vomiting
- light sensitivity
- headache
- stiff neck
- confusion
- weakness
- disorientation
- prosperously, two vaccines are accessible to prevent pneumococcal meningitis. Learn more about them & other ways to obstruct this deadly form of infection.
What are the factors that lead to meningitis?
The following are some of the causes of meningitis:
- Compromised immunity
- People with immunodeficiency are more susceptible to infections. This includes the infections that cause meningitis. Certain disorders & treatments can weaken the immune system. These include:
- HIV/AIDS
- autoimmune disorders
- chemotherapy
- organ or bone marrow transplants
- cancer
- immunosuppressive medication
- Cryptococcal meningitis, which occurs by a fungus, is the most common form of meningitis in people with HIV.
Community living
Meningitis is easily transmitted when people live in close quarters. Being in small areas increases the chance of exposure. Examples include:
- college dormitories
- barracks
- boarding schools
- daycare centers
- assisted living facilities
- Pregnancy
- Pregnant women have a more risk of listeriosis, which is an infection caused by the Listeria bacteria. Infection can spread to the unborn child.
Age: All ages are at risk for meningitis. However, some age groups have a higher risk. Children under the age of 5 are at more risk of viral meningitis. newborns are at higher risk of bacterial meningitis. Older adults can also be at risk for some infections that can lead to meningitis.
Working with animals: Farm workers [farmers]& others who work with animals have more risk of infection with Listeria.
Outlook
- Meningitis is an inflammation of the fluid & three membranes surrounding the brain & spinal cord. Meningitis can cause when fluid surrounding these membranes becomes infected.
- There are some different types of meningitis, including viral, bacterial,& fungal meningitis.
- Meningitis can be quite dangerous if not treated rapidly, & can cause death.
- On a positive note, vaccines, mostly for bacterial meningitis, are available for pre-teens & teens, as well as anyone who may be at a higher risk of developing the condition.
What are the effects of meningitis on the body?
- Meningitis is the inflammation of the protective covering surrounding the brain & spinal cord. There are various types of meningitis, but most are caused by viruses or bacteria. Viral meningitis can make you very sick, but it frequently doesn’t leave lingering effects. Bacterial meningitis is more serious. It increases rapidly & can cause permanent damage or even become life-threatening.
- Quick diagnosis & treatment can help prevent some of the potential long-time side effects. If you have symptoms of meningitis, visit your doctor without delay. Anyone can get meningitis, but it’s more common in babies, children, & youngsters.
Central Nervous System
- The CNS is made up of the brain, spinal cord, & nerves. Meningitis is an infection that causes the conservational membranes of the nervous system to inflame. swelling of the brain & spinal cord can affect every part of the body. Fever & other symptoms can come on suddenly & progress very quickly, causing devastating effects.
- Headache can be a starting warning sign of meningitis. continue headaches may be a problem for some time. Inflammation of the brain can cause a broad range of problems, including cognitive issues & convulsions. The trouble with memory & concentration may last well after the illness has passed. Children may be left with prolonged learning difficulties.
- inflammation in the brain can also interfere with the senses. It can lead to ringing in the ears (tinnitus), partial hearing loss, or deafness. It may cause speech problems. Light sensitivity, eye pain, & loss of vision are possible.
- Inflammation & fever can cause loss of appetite. Sick stomach, nausea, & vomiting are common. Infants & young children may become fussy, irritable, and difficult to comfort. & excessive sleepiness is a symptom of meningitis, so it may be hard to wake a sleeping child. Untreated, meningitis can lead to coma.
- Poor cooperation, dizziness,& clumsiness may remain for some time after a bout with meningitis. Children might have emotional problems following the illness, including clinginess, moodiness, & sleep disturbances.
- Diagnostic testing may include brain imaging & spinal fluid analysis (spinal tap).
Circulatory System
- As bacteria multiply in the bloodstream, they may release toxins (septicemia). Septicemia is a life-threatening condition. Bleeding under the skin starts off looking like a light rash. As the blood pressure decrease & circulation slows, blood vessels become damaged.
- The rash is transmitted & darkens to a deep red or dark purple. The lungs & kidneys may deteriorate, & poor circulation puts the fingers, toes, arms, & legs at risk of amputation.
- Diagnostic procedures may include analyzing the blood for evidence of bacteria. If hospitalized, intravenous fluids, steroids, or antibiotics may be given as part of the treatment.
Skin (Integumentary System)
- At the time of fever, the skin may look blushed. If septicemia sets in & blood vessels become damaged, you’ll see evidence on the skin. At first, the skin may just look a little blotchy. You may mistake symptoms of septicemia for tiny scratches or a small rash. The rash can seem anywhere on the body.
- As the infection aggravates, the rash spreads & gets darker, eventually resembling large bruises. In some cases, the rash can lead to permanent scarring.
- The “glass test” can be used to test the meningitis condition. If you press a drinking glass in opposition to a rash, it should fade. If it’s meningitis, you’ll still be able to see the rash clearly through the glass. Keep in mind that the glass test isn’t 100 percent exact. It’s best to check with your doctor.
Skeletal & Muscular Systems
- Stiff neck & back are common in meningitis. It may become difficult to turn your neck at all. In severe cases, the head, neck, & spine become painfully rigid & arched (opisthotonos). Babies & young children are more likely to experience opisthotonos than older people. A baby with meningitis may produce a high-pitched scream when you try to pick them up. Joint stiffness may continue long after the illness clears up, & arthritis can also be an after-effect.
- For infants, a tight or bulging fontanel (the soft spot on top of a baby’s head) is a sign of inflammation of the brain. If your infant shows this symptom, seek medical attention immediately.
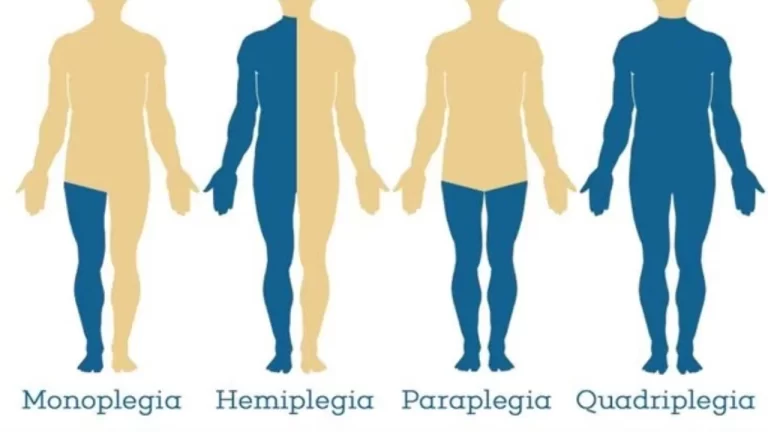
- Muscle weakness is a common symptom of meningitis, both during the illness & in the months that follow. Muscle spasms, body aches, or generalized weakness in some parts of the body may occur.
How meningitis is treated?
The treatment is determined by the cause of meningitis.
Bacterial meningitis requires immediate hospitalization. Early diagnosis & treatment will prevent brain damage & death. Bacterial meningitis is treated with intravenous antibiotics & steroids. There’s no specific antibiotic for bacterial meningitis. It depends on the bacteria involved.
Fungal meningitis is treated with antifungal agents.
Parasitic meningitis may either involve treating just the symptoms & try to treat the infection directly. Depending on the cause, this type may get better without antibiotic medication. If it aggravates, however, your doctor may try to treat the infection itself.
Viral meningitis may solve on its own, but some causes of viral meningitis will be treated with intravenous antiviral medications.
Chronic meningitis is treated by treating the underlying cause first, such as a fungal infection or an immunological issue such as rheumatoid arthritis.
Physiotherapy treatment
- According to the American Physiotherapy Association’s Guide to physioTherapist Practice infectious disorders of the central nervous system fall under the following preferred practice patterns; Impaired Motor Function & Sensory Integrity Associated with the Nonprogressive Disorders of the Central Nervous System- Acquired in Adulthood or Adolescence & Impaired Arousal, Range of Motion, and Motor Control Associated with Coma, Near Coma, or Vegetative State.
- Typically physiotherapy treatment is initiated in the intensive care unit. While initiating a plan of care, it is crucial to keep in mind a patient’s chart information or contraindications to therapy like intracranial pressure, cerebral perfusion pressure, & other lab values that determine rehabilitation guidelines. Meningitis may present with similar symptoms to brain injuries, neurological complications, immunological deficiency, vascular compromise, & additional secondary impairments.
- Further understanding the various stages of consciousness or behavioral changes a patient with secondary complications may go through can guide the approach to treatment. The therapist should create a circumstance that would relieve the patient’s hypersensitivity to sensory input such as light or sound thus creating a structured environment to eliminate behavioral outbursts. Close monitoring of the vital signs will allow the therapist to measure the patient’s receptiveness to therapy. The therapist should be familiar with the Glasgow Coma Scale & monitor the patient’s progression through the levels of consciousness.
- Proper positioning & range of motion exercise should be started as soon as safely possible in the acute phase. Proper positioning with pillows and towels will protect the skin integrity & prevention contractures. Maintaining mobility of the trunk & neck is important to sustain functional movements. The earlier therapy is initiated with a patient, the chances of secondary impairments are decreased allowing for a better outlook.
- A primary key component to treating a patient recovering from bacterial meningitis is proper education not only to the patient but to the family & caregivers as well. Providing the patient and family with education on the disease, stages of the disease, secondary complications, warning signs, & resources can encourage the patient & family to become more involved in the treatment. It is very important to educate on the effects of different systemic involvement & how the timeline of recovery may vary.
How is meningitis prevented?
Maintaining a healthy lifestyle, especially if you are at more risk, is important. This includes:
- getting adequate amounts of rest
- not smoking
- avoiding contact with sick people
- washing the hands often, especially if you work in a daily routine or healthcare setting
- If you’ve been in close contact with one or more people who have a bacterial meningococcal infection, the doctor can give you preventive antibiotics. This will decrease the chances of developing the disease.
Vaccinations can also protect against definite types of meningitis. Vaccines that can restrict meningitis include the following:
- Haemophilus influenza type B (Hib) vaccine
- pneumococcal conjugate vaccine
- meningococcal vaccine
- Practicing good personal cleanliness may also help you prevent meningitis. Some types of meningitis are transmitted through close contact with an infected person’s body fluid, such as saliva & nasal secretions. Avoid sharing drinks, utensils, & personal items that may carry saliva or other fluids.
Pregnancy and listeria
- A listeria infection (L. monocytogenes) can lead to a bacterial meningitis infection if not treated rapidly, & this type of infection can be very dangerous to a developing baby.
- Certain types of food, such as soft cheeses, celery, sprouts, cantaloupe, and ice cream, have recently been connected to listeria outbreaksTrusted Source, but this doesn’t mean eating these foods while pregnant guarantees an infection.
- If you’re pregnant, it’s a good idea to consult your doctor about listeria risks & foods.
FAQ
What are the 5 risk factors associated with meningitis?
Risk factors for meningitis include:
Skipping vaccinations. Risk rises for anyone who hasn’t completed the recommended childhood or adult vaccination schedule.
Age. Most cases of viral meningitis occur in children younger than age 5. …
Living in a community setting. …
Pregnancy. …
Compromised immune system.
What symptom comes first with meningitis?
The primary symptoms are usually fever, vomiting, headache &feeling unwell. Limb pain or pain in the extremities, pale skin, & cold hands & feet often appear earlier than the rash, neck stiffness, dislike of bright lights,& confusion.
How fast does meningitis progress?
Bacterial meningitis – bacterial meningitis has a sudden onset, & can cause serious health problems, or even death, within 24 hours if left untreated. If treated beginning, the symptoms of bacterial meningitis can improve in as little as 2-3 days.
What are the stages of meningitis?
The classic triad of meningitis consists of fever, nuchal rigidity, & altered mental status, but not all patients have all three, & almost all patients have headaches. Altered mental status can range from irritability to somnolence, delirium, & coma
What is the rarest form of meningitis?
Overall, parasitic meningitis is much less common than viral & bacterial meningitis. Primary amebic meningoencephalitis (PAM) is a rare & devastating infection of the brain caused by Naegleria fowleri. Naegleria fowleri is a free-living microscopic ameba that lives in warm water & soil.



5 Comments