Methocarbamol
Introduction of methocarbamol
Methocarbamol is a medication that belongs to a class of drugs known as skeletal muscle relaxants. It is primarily used to relieve muscle spasms and associated pain caused by acute musculoskeletal conditions. Methocarbamol causes muscle relaxation and sedation by depressing the central nervous system. The exact function of methocarbamol is not fully understood. However, it is believed to work by suppressing nerve impulses or signals that are sent to the brain, resulting in muscle relaxation. This drug does not directly act on the muscles themselves but rather on the central nervous system.
Methocarbamol is commonly prescribed for conditions such as muscle strains, sprains, and spasms, often caused by injuries or overexertion. It is frequently used in combination with rest, physical therapy, and other treatments to improve overall musculoskeletal recovery. The medication is typically available in tablet form, and the dosage depends on the severity of the condition being treated. It is usually taken orally, with or without food, and the prescribed frequency and duration of use should be followed as directed by a healthcare professional. Like any medication, methocarbamol may have potential side effects. Common side effects include drowsiness, dizziness, headache, blurred vision, and nausea. It is important to avoid driving or operating heavy machinery until the effects of the medication are known, as it can cause sedation and impair cognitive and motor functions.
As with any medication, it is essential to inform your healthcare provider about any existing medical conditions, allergies, or other medications you are taking before starting methocarbamol. They will be able to determine if this medication is appropriate for you and adjust the dosage if necessary.
In an important point of view, methocarbamol is a skeletal muscle relaxant used to relieve muscle spasms and associated pain caused by acute musculoskeletal conditions. It works by depressing the central nervous system and is commonly prescribed as part of a comprehensive treatment plan that includes rest and physical therapy. If you have any concerns or questions about this medication, it is best to consult with a healthcare professional for personalized advice.
- Pregnancy category: AU: B2
- Metabolism: Liver
- AHFS/Drugs.com: Monograph
- ATC code: M03BA03 (WHO) M03BA53 (WHO) M03BA73 (WHO)
- Elimination half-life: 1.14 to 1.24 hours
- License data: US DailyMed: Methocarbamol
Methocarbamol, which is also sold under the name Robaxin, is a pain reliever for a short duration of time. Rest, physical therapy, and pain medication can all be used with it. In cases of low back pain, it’s not as popular. For rheumatoid arthritis and cerebral palsy, its application is limited.
What do you use methocarbamol for?
Methocarbamol is primarily used for the treatment of muscle spasms and associated pain caused by acute musculoskeletal conditions. Here are some specific situations where methocarbamol may be prescribed:
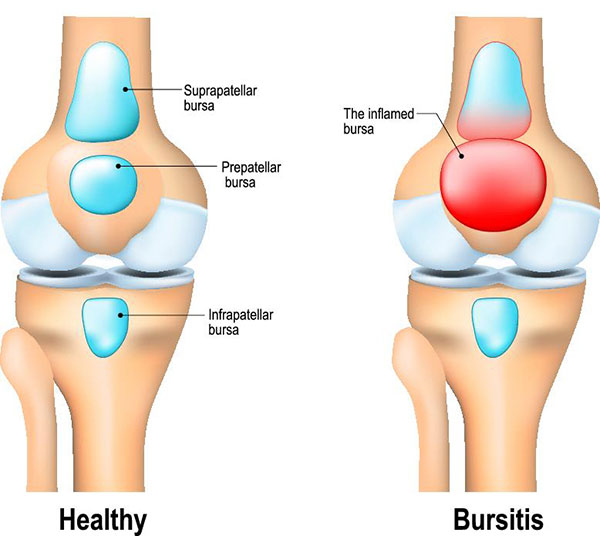
- Muscle Strains: Methocarbamol can be used to alleviate muscle spasms and pain associated with strains, which occur when muscles or tendons are stretched or torn. Strains often result from activities such as lifting heavy objects, overexertion during physical exercise, or sudden movements.
- Sprains: Methocarbamol may also be prescribed for sprains, which involve damage to ligaments connecting bones in a joint. Sprains typically occur due to twisting or wrenching movements and can cause muscle spasms and pain.
- Back Pain: Methocarbamol can help relieve muscle spasms and discomfort associated with acute back pain. This includes conditions such as muscle strains in the lower back, as well as spasms caused by poor posture or muscle imbalances.
- Post-Surgical Muscle Spasms: After certain surgical procedures, muscle spasms may occur as a result of the body’s natural response to trauma. Methocarbamol can be prescribed to manage these post-surgical muscle spasms and provide relief.
- Fibromyalgia: Methocarbamol is sometimes used as part of the treatment for fibromyalgia, a chronic condition characterized by widespread musculoskeletal pain, fatigue, and tenderness in specific areas of the body. While the exact cause of fibromyalgia is unknown, muscle spasms and pain are common symptoms, and methocarbamol may help alleviate these symptoms.
It is important to note that methocarbamol is typically used as a short-term treatment for acute musculoskeletal conditions and is often prescribed in combination with rest, physical therapy, and other supportive measures. Chronic or persistent musculoskeletal pain may require alternative treatment options, and it’s essential to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan.
Who can take the methocarbamol drug?
Methocarbamol can be taken by individuals who require treatment for muscle spasms and associated pain caused by acute musculoskeletal conditions. However, there are certain factors to consider when determining if methocarbamol is suitable for a specific individual. Here are some details regarding who can take methocarbamol:
- Medical Evaluation: Before taking methocarbamol, it is important to consult with a healthcare professional, such as a doctor or pharmacist. They will evaluate your medical history, including any existing medical conditions, allergies, and medications you are currently taking. This evaluation helps ensure that methocarbamol is safe for you and does not interact negatively with any other medications or conditions.
- Adults: Methocarbamol is generally prescribed to adults aged 18 and older. Dosage recommendations may vary depending on the severity of the condition being treated, and healthcare professionals will determine the appropriate dosage and duration of treatment based on individual needs.
- Pregnancy and Breastfeeding: The use of methocarbamol during pregnancy or breastfeeding should be discussed with a healthcare professional. There is limited information available on the safety of methocarbamol in pregnant or breastfeeding individuals, and the potential risks and benefits need to be carefully considered.
- Liver or Kidney Impairment: Individuals with liver or kidney impairment may require dose adjustments or close monitoring while taking methocarbamol. The drug is metabolized in the liver and excreted by the kidneys, so any impairment in these organs can affect the way methocarbamol is processed in the body.
- Sensitivity to the Drug: If you have had an allergic reaction or hypersensitivity to methocarbamol in the past, it is important to avoid using it again and to inform your healthcare provider about this sensitivity. They can suggest alternative treatment options that are better suited for you.
- Driving and Operating Machinery: Methocarbamol can cause drowsiness, and dizziness, and impair cognitive and motor functions. It is essential to assess how the medication affects you individually before engaging in activities that require alertness, such as driving or operating heavy machinery. If you experience significant drowsiness or dizziness, it is important to refrain from such activities until you are certain of how the medication affects you.
Remember, the decision to use methocarbamol should be made in consultation with a healthcare professional who can assess your specific situation and provide personalized advice. They will consider your medical history, the severity of your condition, and other relevant factors to determine if methocarbamol is suitable for you.
Who Cannot take methocarbamol drug?
While methocarbamol is generally safe and well-tolerated, certain individuals may be advised against taking this medication. Here are some situations where methocarbamol may not be recommended:
- Allergy or Hypersensitivity: Individuals who have a known allergy or hypersensitivity to methocarbamol or any of its components should avoid taking the drug. Allergic reactions can range from mild skin rashes to severe allergic responses, such as difficulty breathing or swelling of the face, throat, or tongue. If you have experienced an allergic reaction to methocarbamol in the past, it is important to inform your healthcare provider.
- Renal Impairment: Methocarbamol is primarily excreted by the kidneys. Individuals with severe renal impairment or end-stage renal disease may require dosage adjustments or close monitoring while taking this medication. Reduced kidney function can affect how methocarbamol is processed and eliminated from the body, potentially leading to an increased risk of side effects.
- Liver Impairment: Methocarbamol is metabolized in the liver. Individuals with severe liver impairment or liver disease may require dosage adjustments or close monitoring. Liver dysfunction can affect the metabolism and clearance of methocarbamol from the body, potentially leading to an increased risk of side effects.
- Pregnancy and Breastfeeding: The use of methocarbamol during pregnancy or breastfeeding should be discussed with a healthcare professional. Limited information is available on the safety of methocarbamol in these situations, and the potential risks and benefits need to be carefully considered.
- CNS Depression: Methocarbamol can cause central nervous system (CNS) depression, leading to drowsiness and impairing cognitive and motor functions. Individuals who have conditions that already depress the CNS, such as severe respiratory depression, coma, or concurrent use of other CNS depressant medications (e.g., opioids, sedatives) may be at increased risk of experiencing excessive sedation and respiratory depression. Close monitoring and caution are advised in such cases.
- Children: Methocarbamol is not typically recommended for children under the age of 18. Safety and efficacy data for pediatric use are limited, and alternative treatment options may be considered for muscle spasms in children.
It’s important to note that the decision regarding the use of methocarbamol should be made in consultation with a healthcare professional who can assess your circumstances and medical history. They will consider potential contraindications and determine if methocarbamol is appropriate for you or if alternative treatments should be considered.
Classification of methocarbamol drug
Methocarbamol is classified as a skeletal muscle relaxant. It belongs to a class of medications known as centrally-acting muscle relaxants. These drugs are primarily used to alleviate muscle spasms and associated pain by acting on the central nervous system to induce muscle relaxation. More specifically, methocarbamol is classified as a carbamate derivative. It is chemically related to guaifenesin, which is an expectorant commonly used to thin and loosen mucus in the respiratory tract. Methocarbamol has additional muscle relaxant properties compared to guaifenesin, making it useful for treating musculoskeletal conditions.
Methocarbamol’s precise mechanism of action is still poorly understood. It is believed to work by suppressing nerve impulses or signals sent to the brain, resulting in muscle relaxation. However, its specific effects on the central nervous system are complex and not completely elucidated.
The classification of methocarbamol as a skeletal muscle relaxant helps to differentiate it from other types of medications used for pain management or muscle-related conditions. By targeting muscle spasms directly, it provides relief from symptoms associated with acute musculoskeletal conditions, such as strains, sprains, and back pain. It is worth noting that while methocarbamol is classified as a skeletal muscle relaxant, it is sedative properties and effects on the central nervous system contribute to its therapeutic actions. These properties can also cause side effects, such as drowsiness and dizziness, which need to be taken into consideration when using the medication.
Mechanism of Action of methocarbamol drug
The exact mechanism of action of methocarbamol is not completely comprehended. However, it is believed to exert its effects by depressing the central nervous system (CNS) and producing muscle relaxation. Here is a general overview of the proposed mechanisms:
- CNS Depression: Methocarbamol acts primarily in the CNS, specifically in the brain and spinal cord. It is thought to depress nerve activity and inhibit the transmission of signals from the muscles to the brain. By reducing the excitability of motor neurons, methocarbamol helps to alleviate muscle spasms.
- GABAergic Activity: Methocarbamol has been suggested to enhance the effects of gamma-aminobutyric acid (GABA), which is an inhibitory neurotransmitter in the CNS. GABA works to reduce neuronal activity and promote relaxation. Methocarbamol may facilitate GABAergic transmission, leading to increased inhibitory effects and muscle relaxation.
- Sedative Properties: Methocarbamol has mild sedative properties, which contribute to its muscle relaxant effects. By inducing sedation, the drug can help calm the nervous system and promote relaxation of the muscles.
It’s important to note that while the proposed mechanisms provide a general understanding of how methocarbamol works, the exact details and interactions within the CNS are still not fully elucidated. Furthermore, the drug’s effects on the peripheral musculoskeletal system may also play a role in its muscle relaxant properties. It is always recommended to consult with a healthcare professional for more specific and detailed information about the mechanism of action of methocarbamol, as well as its use in individual cases.
Pharmacodynamics of methocarbamol drug
Certainly! Here is a more detailed explanation of the pharmacodynamics of methocarbamol:
- Central Nervous System (CNS) Depression: Methocarbamol acts centrally on the CNS to depress nerve activity, leading to muscle relaxation. It is believed to inhibit the transmission of signals from the muscles to the brain, thereby reducing muscle spasms. The drug likely exerts its effects through interaction with various neurotransmitter systems in the CNS.
- GABAergic Modulation: Methocarbamol has been shown to enhance the effects of gamma-aminobutyric acid (GABA), the primary inhibitory neurotransmitter in the CNS. GABA functions to reduce neuronal excitability and promote relaxation. Methocarbamol is thought to potentiate GABAergic transmission, leading to increased inhibition and muscle relaxation.
- Calcium Ion Channels: Methocarbamol may interact with calcium ion channels in the CNS. By inhibiting the influx of calcium ions into nerve cells, it may decrease the release of excitatory neurotransmitters, thereby reducing muscle spasms and pain.
- Sedative Properties: Methocarbamol has mild sedative properties, which contribute to its muscle relaxant effects. By depressing the CNS, the drug induces sedation and helps calm the nervous system, promoting muscle relaxation.
- Peripheral Effects: While the exact mechanisms are not fully understood, methocarbamol may also have direct effects on the peripheral musculoskeletal system. It is believed to affect muscle tone, reduce muscle spasms, and improve overall muscle function. However, the specific targets and mechanisms in the periphery remain to be fully elucidated.
- Metabolism: Methocarbamol is metabolized in the liver by various enzymes, including cytochrome P450 enzymes. The metabolism of methocarbamol leads to the formation of metabolites, which are excreted primarily in the urine.
It is important to note that the pharmacodynamics of methocarbamol can vary between individuals, and its precise mechanisms of action are still not completely understood. The drug’s effects on the CNS, GABAergic system, calcium ion channels, and peripheral musculoskeletal system collectively contribute to its muscle relaxant properties. As always, it is recommended to consult with a healthcare professional for a comprehensive understanding of the pharmacodynamics of methocarbamol, especially concerning your specific medical condition and individual factors.
Metabolism of Methocarbamol
Methocarbamol undergoes hepatic metabolism, primarily through enzymatic processes in the liver. Here is an overview of the metabolism of methocarbamol:
- Phase I Metabolism: In phase, I metabolism, methocarbamol is primarily metabolized by the liver’s cytochrome P450 (CYP) enzymes. The main CYP enzymes involved in its metabolism are CYP1A2, CYP2B6, and CYP3A4. These enzymes catalyze reactions, including hydroxylation and demethylation, to convert methocarbamol into metabolites.
- Metabolites: The major metabolites of methocarbamol include 3-(hydroxy-methyl)-methocarbamol and 3-(methoxy-methyl)-methocarbamol. These metabolites are pharmacologically active but have weaker muscle relaxant properties compared to the parent compound.
- Elimination: After undergoing metabolism, methocarbamol, and its metabolites are primarily excreted in the urine. A small portion of the drug may also be eliminated in the feces. The elimination half-life of methocarbamol is approximately 1 to 2 hours, which means it takes this amount of time for half of the drug to be cleared from the body.
- Interactions: Methocarbamol metabolism can be influenced by various factors, including genetic variations in CYP enzymes and drug interactions. For example, medications that inhibit or induce CYP enzymes, such as certain antibiotics or antifungals, may affect the metabolism of methocarbamol. It’s important to consider potential interactions and consult with a healthcare professional or pharmacist when taking methocarbamol alongside other medications.
It is worth noting that individual variations in metabolism can occur, and some individuals may metabolize methocarbamol at different rates or produce different metabolites. Factors such as age, liver function, and genetic factors can influence the metabolism of methocarbamol. As always, it is advisable to consult with a healthcare professional or pharmacist for more specific information on the metabolism of methocarbamol, especially concerning your circumstances and any potential drug interactions.
Absorption of Methocarbamol
Methocarbamol is readily absorbed after oral administration, and here is a detailed explanation of its absorption process:
- Oral Administration: Methocarbamol is typically administered orally in the form of tablets or capsules. It is usually taken with or without food, as directed by the healthcare professional.
- Absorption from the Gastrointestinal Tract: After oral ingestion, methocarbamol is absorbed primarily from the gastrointestinal tract. The drug undergoes dissolution in the stomach and small intestine, where it is then available for absorption.
- Lipophilic Nature: Methocarbamol is a lipophilic compound, meaning it has an affinity for fat and lipid-containing substances. This lipophilic nature allows methocarbamol to pass through the lipid membranes of the gastrointestinal tract for absorption.
- Passive Diffusion: The absorption of methocarbamol occurs primarily through passive diffusion, which is a process that relies on concentration gradients. Methocarbamol molecules move from an area of higher concentration (the gastrointestinal lumen) to an area of lower concentration (the bloodstream).
- Time to Peak Plasma Concentration: Following oral administration, methocarbamol is rapidly absorbed, and the time it takes to reach peak plasma concentration varies. In general, peak plasma levels are achieved within 1 to 2 hours after ingestion.
- Bioavailability: The bioavailability of methocarbamol, which refers to the fraction of the administered dose that reaches the systemic circulation, is reported to be approximately 24% to 50%. This means that a portion of the drug may undergo first-pass metabolism in the liver before reaching systemic circulation.
- Food Effects: While methocarbamol can be taken with or without food, it is worth noting that the presence of food in the stomach can affect its absorption. Taking methocarbamol with a meal may slightly delay the time to reach peak plasma concentration, but it does not significantly alter the extent of absorption.
It is important to follow the specific dosing instructions provided by the healthcare professional and adhere to the prescribed regimen for optimal absorption and therapeutic effect. If you have any concerns or questions regarding the absorption of methocarbamol, it is advisable to consult with a healthcare professional or pharmacist.
The volume of distribution of methocarbamol
The volume of distribution (Vd) of methocarbamol is approximately 1.3 to 2.1 L/kg. The volume of distribution is a pharmacokinetic parameter that describes the apparent space in the body where a drug is distributed. It is used to estimate the extent of drug distribution beyond the bloodstream and provides insights into the drug’s distribution into tissues and organs.
A volume of distribution of 1.3 to 2.1 L/kg indicates that methocarbamol is moderately distributed throughout the body. This means that the drug tends to distribute into tissues and organs beyond the blood compartment.
It is important to note that the volume of distribution can vary among individuals based on factors such as age, weight, body composition, and specific patient characteristics. Additionally, it is influenced by the physicochemical properties of the drug, including its lipophilicity and ability to bind to plasma proteins. The volume of distribution is a crucial parameter for drug dosing calculations and helps in understanding the drug’s pharmacokinetic behavior. However, it is important to consult with a healthcare professional or pharmacist for precise information on the volume of distribution of methocarbamol, as they can provide specific details based on individual circumstances and patient factors.
Protein binding of methocarbamol
Methocarbamol has a low degree of protein binding, with approximately 46% to 50% of the drug bound to plasma proteins. Protein binding refers to the attachment of a drug to proteins in the bloodstream, primarily albumin. When a drug is highly protein-bound, it remains bound to proteins and has limited availability for distribution and action in the body. Conversely, when a drug has low protein binding, it is more readily available for distribution and pharmacological activity.
With methocarbamol’s protein binding ranging from 46% to 50%, it indicates that a significant portion of the drug remains unbound and freely available for distribution to target tissues and exert its therapeutic effects. The extent of protein binding can impact a drug’s pharmacokinetics, including its distribution, metabolism, and elimination. Unbound (free) drug molecules are typically responsible for the pharmacological activity, while protein-bound drug molecules serve as a reservoir or depot. It is worth noting that interactions with other drugs that are highly protein-bound may potentially affect the protein binding and distribution of methocarbamol. Consequently, any concomitant use of medications that are extensively protein-bound should be carefully considered and monitored to ensure appropriate dosing and minimize the risk of adverse effects.
As with any medication, it is important to consult with a healthcare professional or pharmacist for precise information regarding the protein binding of methocarbamol, as they can provide specific details based on individual circumstances and patient factors.
Route of elimination of methocarbamol
Methocarbamol is primarily eliminated through renal excretion, with a small portion of the drug being eliminated in the feces. After undergoing metabolism in the liver, methocarbamol and its metabolites are excreted primarily in the urine. The renal elimination of methocarbamol occurs through a combination of glomerular filtration and active tubular secretion. The drug and its metabolites are filtered out of the bloodstream by the glomeruli in the kidneys and then actively transported into the urine by the renal tubules.
A small fraction of methocarbamol and its metabolites may also undergo biliary excretion and subsequent elimination in the feces. However, the fecal elimination of methocarbamol is considered a minor route compared to renal excretion. It is worth noting that the specific percentages of renal and fecal elimination can vary between individuals and depend on factors such as renal function, hepatic metabolism, and overall health.
In cases of impaired renal function, dosage adjustments may be necessary to avoid drug accumulation. Similarly, in patients with compromised hepatic function, caution should be exercised as impaired metabolism can affect the elimination of methocarbamol. As always, it is important to consult with a healthcare professional or pharmacist for precise information regarding the route of elimination of methocarbamol, especially considering individual circumstances and potential drug interactions.
Half-life of methocarbamol
The half-life of methocarbamol can vary between individuals but is generally reported to be approximately 1 to 2 hours. The half-life of a drug refers to the time it takes for the concentration of the drug in the body to decrease by half. Methocarbamol has a relatively short half-life, indicating that it is eliminated from the body relatively quickly. It is important to note that the half-life of methocarbamol can be influenced by factors such as age, liver function, renal function, and individual metabolism. Additionally, the specific formulation and dosage of methocarbamol may also affect its pharmacokinetics and half-life.
Understanding the half-life of a drug is important for determining the dosing frequency and establishing a steady-state concentration in the body. In the case of methocarbamol, the relatively short half-life suggests that it may be necessary to take the medication multiple times a day to maintain therapeutic levels. It is always recommended to consult with a healthcare professional or pharmacist for precise information regarding the half-life of methocarbamol, as they can provide specific details based on individual circumstances and patient factors.
Clearance of methocarbamol
The clearance of methocarbamol refers to the rate at which the drug is removed from the body, typically measured in milliliters per minute (mL/min) or liters per hour (L/hr). The total clearance of methocarbamol is a combination of hepatic clearance and renal clearance.
- Hepatic Clearance: Methocarbamol undergoes hepatic metabolism, primarily through enzymatic processes in the liver. The metabolism of methocarbamol involves cytochrome P450 (CYP) enzymes, primarily CYP1A2, CYP2B6, and CYP3A4. These enzymes convert methocarbamol into its metabolites, which are less pharmacologically active than the parent compound. The hepatic clearance of methocarbamol refers to the rate at which the drug is metabolized and cleared by the liver.
- Renal Clearance: After undergoing hepatic metabolism, methocarbamol, and its metabolites are primarily excreted in the urine. Renal clearance refers to the rate at which the drug and its metabolites are eliminated from the body via the kidneys. Renal clearance involves filtration of the drug through the glomeruli in the kidneys, followed by active tubular secretion and reabsorption processes.
The total clearance of methocarbamol is influenced by factors such as liver function, renal function, and individual patient characteristics. Impaired liver or kidney function may result in decreased clearance and potentially require dosage adjustments. The precise value for the clearance of methocarbamol can vary among individuals based on various factors, and it is typically not readily available in standard drug references. For specific information regarding the clearance of methocarbamol, it is recommended to consult with a healthcare professional or pharmacist, who can consider individual patient factors and provide more precise details.
Pathways of methocarbamol
Methocarbamol undergoes various metabolic pathways in the body, primarily involving hepatic metabolism. The major pathways of methocarbamol include:
- Hydroxylation: Methocarbamol is metabolized through hydroxylation reactions, primarily catalyzed by cytochrome P450 (CYP) enzymes, such as CYP1A2, CYP2B6, and CYP3A4. Hydroxylation involves the addition of a hydroxyl group (-OH) to the drug molecule, resulting in the formation of hydroxylated metabolites of methocarbamol.
- Demethylation: Methocarbamol can also undergo demethylation, which involves the removal of a methyl group (-CH3) from the drug molecule. This demethylation process results in the formation of demethylated metabolites of methocarbamol.
- Glucuronidation: Methocarbamol can be conjugated with glucuronic acid through glucuronidation, primarily occurring in the liver. Glucuronidation is a phase II metabolic pathway where the drug or its metabolites are conjugated with glucuronic acid to increase their water solubility, facilitating excretion in the urine.
- These metabolic pathways result in the formation of active metabolites of methocarbamol, including 3-(hydroxy-methyl)-methocarbamol and 3-(methoxy-methyl)-methocarbamol. These metabolites contribute to the overall pharmacological activity of the drug, albeit with weaker muscle relaxant properties compared to the parent compound.
It s worth noting that individual variations in metabolism can occur, and some individuals may metabolize methocarbamol differently, resulting in variations in the formation and clearance of specific metabolites. The metabolism of methocarbamol is primarily hepatic, and its metabolites are eliminated primarily in the urine. However, it’s important to consider that the specific metabolic pathways and their relative contributions may be influenced by factors such as genetics, drug interactions, and individual patient characteristics.
For comprehensive information on the metabolic pathways of methocarbamol, it is advisable to consult with a healthcare professional or pharmacist who can provide specific details based on individual circumstances and potential drug interactions.
Toxicity of methocarbamol
Methocarbamol is generally considered to have a relatively low toxicity profile when used at therapeutic doses. However, like any medication, it can potentially cause adverse effects, especially when taken in excessive amounts or by certain individuals with specific medical conditions. Here are some considerations regarding the toxicity of methocarbamol:
- Central Nervous System (CNS) Depression: Methocarbamol has muscle relaxant properties and can have sedative effects on the central nervous system. In high doses or when combined with other substances that also depress the CNS, such as alcohol or opioids, methocarbamol can cause excessive sedation, drowsiness, dizziness, and impaired coordination. These effects can interfere with tasks that require alertness and may increase the risk of accidents.
- Allergic Reactions: Although rare, some individuals may experience allergic reactions to methocarbamol. An allergic reaction can be characterized by a rash, itching, swelling, dizziness, and trouble breathing. It is important to seek immediate medical attention in the event of an allergic reaction.
- Gastrointestinal Effects: Methocarbamol can occasionally cause gastrointestinal side effects, including nausea, vomiting, and stomach upset. These effects are usually benign and transient.
- Hypotension: In rare cases, methocarbamol can cause a drop in blood pressure, resulting in hypotension. This may manifest as lightheadedness, dizziness, or fainting. Individuals with pre-existing low blood pressure or those taking medications that lower blood pressure may be at higher risk.
- Other Side Effects: Additional side effects of methocarbamol may include headache, blurred vision, urinary retention, and skin reactions. It’s important to consult a healthcare professional if any concerning or persistent side effects are experienced.
In the event of an overdose or severe adverse reaction, immediate medical attention should be sought. Overdose of methocarbamol can lead to severe CNS depression, respiratory depression, and even coma. It is crucial to follow the prescribed dosage and instructions provided by the healthcare professional and inform them of any pre-existing medical conditions, allergies, or medications being taken to minimize the risk of adverse effects. This information is not exhaustive, and it’s essential to consult with a healthcare professional or pharmacist for comprehensive and personalized guidance regarding the potential toxicity and side effects of methocarbamol.
The function of methocarbamol
The primary function of methocarbamol is as a muscle relaxant. It is used to provide relief from muscle spasms and associated pain. Methocarbamol acts on the central nervous system (CNS) to alleviate muscle tension and promote muscle relaxation.
The exact mechanism of action of methocarbamol is not fully understood, but it is believed to involve a combination of effects. Methocarbamol is thought to reduce muscle spasms and promote relaxation by inhibiting the transmission of nerve impulses or signals in the spinal cord. It may also exert its effects by depressing the activity of neurons in the brainstem, which further contributes to muscle relaxation.
By reducing muscle spasms and tension, methocarbamol can help alleviate symptoms associated with conditions such as muscle strains, sprains, back pain, and other musculoskeletal disorders. It is often prescribed as part of a comprehensive treatment plan that may also include rest, physical therapy, and other supportive measures. It is important to note that methocarbamol is not a painkiller or analgesic in itself, although it may indirectly help reduce pain by relieving muscle spasms and tension. If pain is a significant component of the condition, additional pain relief measures may be necessary.
The use of methocarbamol should be directed by a healthcare professional, who will determine the appropriate dosage and duration of treatment based on the individual’s specific condition and needs. It is worth noting that methocarbamol may have sedative effects and can cause drowsiness or impair cognitive and motor functions. Therefore, it is important to use caution when engaging in activities that require alertness, such as driving or operating machinery, especially when starting treatment or adjusting the dosage. This information is not exhaustive, and it’s essential to consult with a healthcare professional or pharmacist for comprehensive and personalized guidance regarding the specific function and appropriate use of methocarbamol.
How long should I use an over-the-counter methocarbamol drug?
However, I can offer some general information regarding the use of over-the-counter (OTC) medications containing methocarbamol. It is important to note that the availability of methocarbamol as an OTC medication may vary depending on the country or region. In some areas, methocarbamol may only be available with a prescription. Therefore, it’s crucial to consult with a healthcare professional or pharmacist to determine the appropriate course of action and to ensure compliance with local regulations.
Regarding the duration of use, OTC medications are typically designed for short-term or temporary relief of symptoms. If you are experiencing muscle spasms or related symptoms, it’s recommended to use OTC methocarbamol as directed on the packaging or as advised by a healthcare professional.
If your symptoms persist or worsen despite using the OTC medication, it’s important to seek medical advice. A healthcare professional can evaluate your condition, provide a proper diagnosis, and determine whether further treatment or a different approach is necessary. It is also important to follow the instructions provided with the OTC medication and adhere to the recommended dosage and duration of use. If you have any underlying medical conditions or are taking other medications, it’s advisable to consult with a healthcare professional or pharmacist to ensure there are no contraindications or potential interactions.
Remember that the information provided here is general and not a substitute for professional medical advice. Always consult with a healthcare professional or pharmacist for personalized guidance based on your specific situation.
How long does methocarbamol take to work?
The onset of action of methocarbamol can vary among individuals. In general, methocarbamol starts to take effect within 30 minutes to 1 hour after administration. However, it’s important to note that the time it takes for methocarbamol to work may depend on several factors, including the individual’s metabolism, the severity of muscle spasms, and other personal factors. It is also worth mentioning that while methocarbamol may provide some immediate relief, its full effect may take a few days or weeks of consistent use to achieve optimal results. The medication is typically used as part of a comprehensive treatment plan, which may include rest, physical therapy, and other supportive measures to address the underlying cause of muscle spasms or pain.
If you are using methocarbamol and do not experience a noticeable improvement in your symptoms within a reasonable timeframe, it’s important to consult with a healthcare professional. They can evaluate your condition, reassess your treatment plan, and make any necessary adjustments to ensure the most effective and appropriate management of your symptoms. Remember to follow the recommended dosage and instructions provided by your healthcare professional or as indicated on the medication packaging. If you have any concerns or questions about the timing or effectiveness of methocarbamol, it is always best to consult with a healthcare professional or pharmacist for personalized advice based on your specific situation.
Why this methocarbamol is prescribed?
Methocarbamol is prescribed for the treatment of muscle spasms and associated pain. It is primarily used to provide relief from acute musculoskeletal conditions, such as muscle strains, sprains, and back pain. Muscle spasms can occur due to various reasons, including muscle injuries, overexertion, or underlying musculoskeletal conditions. These spasms can result in pain, stiffness, and limited range of motion. Methocarbamol acts as a muscle relaxant by helping to alleviate muscle spasms and reduce associated discomfort.
The medication is typically prescribed as part of a comprehensive treatment plan, which may also include rest, physical therapy, heat or cold therapy, and other supportive measures. Methocarbamol is intended to be used as a short-term treatment option, generally for a few days to a few weeks, depending on the specific condition and individual response. It is important to note that methocarbamol is not a painkiller or analgesic in itself, although it may indirectly help reduce pain by relieving muscle spasms and tension. If pain is a significant component of the condition, additional pain relief measures may be necessary.
The specific dosage, duration of treatment, and frequency of administration will depend on the individual’s condition and the healthcare professional’s assessment. It’s essential to follow the instructions provided by the prescribing healthcare professional or as indicated on the medication packaging. If you have any questions or concerns about why methocarbamol has been prescribed for you, it’s best to consult with your healthcare professional. They can provide personalized advice and information based on your specific condition and medical history.
How does my doctor choose a methocarbamol drug that’s good for me?
When selecting a methocarbamol drug that is suitable for you, your doctor will consider several factors to ensure the medication is appropriate and effective. Here are some key considerations in the decision-making process:
- Medical History: Your doctor will review your medical history, including any underlying medical conditions or previous drug reactions. They will assess whether there are any contraindications or potential risks associated with methocarbamol use in your specific case.
- Condition Being Treated: Your doctor will evaluate the nature and severity of your muscle spasms and associated pain. They will consider the underlying cause, the affected area, and the duration of symptoms. This information helps determine if methocarbamol is an appropriate treatment choice for your specific condition.
- Medication Interactions: Your doctor will review any medications you are currently taking, including prescription drugs, over-the-counter medications, and supplements. They will assess for potential drug interactions between methocarbamol and other medications to ensure compatibility and prevent adverse effects.
- Individual Factors: Your doctor will take into account individual factors that may influence the selection of a methocarbamol drug. These factors may include your age, weight, renal or hepatic function, pregnancy or breastfeeding status, and any specific considerations related to your unique circumstances.
- Side Effect Profile: Your doctor will consider the side effect profile of methocarbamol and evaluate if the potential benefits outweigh the potential risks. They will take into account any pre-existing conditions or sensitivity to certain side effects that may affect the choice of methocarbamol formulation or dosage.
- Patient Preferences: Your doctor will also consider your preferences, such as medication form (tablet, injection, etc.) and dosing frequency, to ensure the selected methocarbamol drug aligns with your preferences and lifestyle.
Based on these considerations, your doctor will make an informed decision and prescribe a methocarbamol drug that is most suitable for you. They will provide specific instructions regarding dosage, duration of treatment, and any precautions or follow-up monitoring required.
It is essential to communicate openly with your doctor, providing accurate information about your medical history, current medications, and any concerns or preferences you may have. This collaborative approach will help ensure that the chosen methocarbamol drug is tailored to your specific needs and promotes optimal treatment outcomes.
What are the side effects of the methocarbamol drug?
Methocarbamol, like any medication, can potentially cause side effects. Not everyone experiences side effects, and the severity and frequency of side effects can vary among individuals. It’s important to note that not all of the following side effects may occur, but here are some of the potential side effects associated with methocarbamol:
- Drowsiness and Sedation: Methocarbamol can cause drowsiness, dizziness, and a feeling of sedation. These effects can impair cognitive and motor functions, making activities such as driving or operating machinery unsafe. It’s recommended to avoid such activities until you know how methocarbamol affects you.
- Gastrointestinal Effects: Some individuals may experience gastrointestinal side effects, including nausea, vomiting, stomach upset, or diarrhea. These effects are generally mild and temporary.
- Headache: Headaches may occur as a side effect of methocarbamol use. If you experience persistent or severe headaches, it’s important to consult with your healthcare professional.
- Allergic Reactions: Although rare, methocarbamol can potentially cause allergic reactions in some individuals. An allergic reaction can be characterized by a rash, itching, swelling, dizziness, or trouble breathing. Look for guaranteed clinical consideration assuming you experience any indications of an unfavorably susceptible response.
- Hypotension: Methocarbamol may cause a drop in blood pressure (hypotension) in rare cases. This can make you feel dizzy, lightheaded, or faint. Individuals with pre-existing low blood pressure or those taking medications that lower blood pressure may be at higher risk.
- Visual Disturbances: Methocarbamol can occasionally cause blurred vision or other visual disturbances. If you experience any changes in your vision, it’s important to consult with your healthcare professional.
- Urinary Retention: In rare instances, methocarbamol may cause difficulty in passing urine (urinary retention). This may require medical attention if it becomes bothersome.
It is essential to keep in mind that this list does not include all possible side effects. Additionally, the frequency and severity of side effects can vary among individuals. If you experience any concerning or persistent side effects while taking methocarbamol, it’s important to consult with your healthcare professional for further evaluation and guidance. Remember to follow the prescribed dosage and instructions provided by your healthcare professional and inform them of any pre-existing medical conditions or medications you are taking to minimize the risk of side effects and ensure the safe use of methocarbamol.
What should I know regarding the storage and disposal of this drug?
When it comes to the storage and disposal of methocarbamol or any medication, it’s important to follow proper guidelines to ensure safety and effectiveness. Here are a few things to keep in mind:
Storage:
- Read the Label: Start by carefully reading the medication packaging and label instructions. They may provide specific storage recommendations for methocarbamol.
- Room Temperature: In general, methocarbamol should be stored at room temperature, typically between 20 to 25 degrees Celsius (68 to 77 degrees Fahrenheit). Avoid exposing it to extreme temperatures, such as excessive heat or cold, as it may affect the stability and potency of the medication.
- Moisture and Light: Protect methocarbamol from moisture and light. It’s usually recommended to store the medication in its original packaging, which provides some level of protection. Avoid storing it in areas such as bathrooms or kitchen cabinets where moisture levels may be high.
- Keep Out of Reach of Children and Pets: Store methocarbamol in a secure location, out of reach of children and pets. Consider using child-resistant containers for added safety.
- Medication Separation: Store methocarbamol away from other medications to prevent mix-ups. It’s essential to keep medicine in the right place by using labeled and organized.
Disposal:
- Check Expiration Date: Before disposing of methocarbamol, check the expiration date. Expired medications should not be used or kept.
- Follow Local Guidelines: Follow the specific guidelines provided by your local health authorities or waste management facilities regarding medication disposal. Different regions may have different recommendations or programs in place.
- Do Not Flush or Pour Down the Drain: Avoid flushing methocarbamol down the toilet or pouring it down the drain, as it can contribute to environmental contamination.
- Dispose of Household Trash: If no specific disposal instructions are provided, you can generally dispose of methocarbamol in the household trash. To prevent accidental ingestion, it’s recommended to mix the medication with an undesirable substance such as coffee grounds or cat litter, and seal it in a secure bag or container before placing it in the trash.
- Take-Back Programs: Check if there are any medication take-back programs or designated drop-off locations in your community. These programs provide a safe and environmentally friendly way to dispose of medications.
If you have any specific questions or concerns regarding the storage or disposal of methocarbamol, it’s best to consult with your healthcare professional or pharmacist. They can provide guidance based on your location and specific circumstances, ensuring proper handling and disposal of the medication.
In what circumstances should I check with my doctor before taking this drug
It’s important to consult with your doctor before taking methocarbamol in various circumstances to ensure safe and appropriate use. Here are some specific situations where it is advisable to check with your doctor before taking methocarbamol:
- Medical History: If you have a history of liver or kidney disease, it’s important to inform your doctor. Methocarbamol is primarily eliminated by the kidneys, and dosage adjustments may be necessary for individuals with impaired kidney function.
- Allergies and Sensitivities: If you have known allergies or sensitivities to methocarbamol or any other medications, it’s crucial to inform your doctor. They can assess the potential risk and determine if an alternative medication or approach is necessary.
- Pregnancy and Breastfeeding: If you are pregnant, planning to become pregnant, or breastfeeding, it’s essential to discuss the use of methocarbamol with your doctor. They can evaluate the potential risks and benefits and guide whether it is safe to use the medication in your specific situation.
- Other Medications: Inform your doctor about all the medications you are currently taking, including prescription drugs, over-the-counter medications, and supplements. Methocarbamol can interact with certain medications, such as sedatives, tranquilizers, and other muscle relaxants. Your doctor can assess potential interactions and adjust the treatment plan if needed.
- Underlying Medical Conditions: If you have any underlying medical conditions, such as respiratory disorders, epilepsy, or myasthenia gravis, it’s important to inform your doctor. Methocarbamol may affect these conditions, and your doctor can determine if it is safe to use the medication or if an alternative treatment option should be considered.
- Elderly Population: If you are an older adult, your doctor may need to assess the potential risks and benefits of methocarbamol use in light of your age-related changes, such as decreased kidney or liver function, increased sensitivity to sedative effects, and potential interactions with other medications commonly used by older adults.
These are general circumstances where it is advisable to consult with your doctor before taking methocarbamol. However, it’s important to communicate openly with your doctor about your specific medical history, current medications, and any concerns you may have. They can provide personalized advice and recommendations based on your situation to ensure the safe and appropriate use of methocarbamol.
Before taking the methocarbamol drug
Before taking methocarbamol, it’s important to consider the following:
- Consult with Your Healthcare Professional: Speak to your healthcare professional, such as a doctor or pharmacist, before starting methocarbamol. They can assess your medical history, current medications, and any underlying conditions to determine if methocarbamol is suitable for you.
- Allergies: Inform your healthcare professional if you have any known allergies or sensitivities to methocarbamol or any other medications. They can evaluate the potential risks and determine if an alternative medication is necessary.
- Medical Conditions: Disclose any pre-existing medical conditions you have, such as liver or kidney disease, respiratory disorders, epilepsy, or myasthenia gravis. Methocarbamol may interact with these conditions, and your healthcare professional can assess if the medication is appropriate or if an alternative treatment option should be considered.
- Pregnancy and Breastfeeding: If you are pregnant, planning to become pregnant, or breastfeeding, it’s important to discuss the use of methocarbamol with your healthcare professional. They can evaluate the potential risks and benefits and provide recommendations on whether it is safe to use the medication in your specific situation.
- Medication Interactions: Inform your healthcare professional about all the medications you are currently taking, including prescription drugs, over-the-counter medications, and supplements. Methocarbamol may interact with certain medications, such as sedatives, tranquilizers, and other muscle relaxants. Your healthcare professional can assess potential interactions and adjust the treatment plan if needed.
- Dosage and Instructions: Follow the recommended dosage and instructions provided by your healthcare professional or as indicated on the medication packaging. Do not exceed the prescribed dose or use the medication for longer than advised.
- Side Effects: Be aware of the potential side effects associated with methocarbamol. Common side effects include drowsiness, dizziness, gastrointestinal effects (such as nausea or diarrhea), and headache. If you experience any concerning or persistent side effects, consult your healthcare professional.
- Driving and Operating Machinery: Methocarbamol can cause drowsiness and affect cognitive and motor functions. Avoid driving or operating machinery until you know how methocarbamol affects you.
- Storage and Disposal: Follow proper storage guidelines for methocarbamol to ensure its effectiveness. Dispose of unused or expired medication according to local guidelines or medication take-back programs.
Always consult with your healthcare professional for personalized advice and recommendations based on your specific circumstances. They can supply guidance on the safe and appropriate use of methocarbamol and address any concerns or questions you may have.
Can methocarbamol drugs cause allergic reactions?
Yes, methocarbamol can potentially cause allergic reactions in some individuals. Allergic reactions occur when the immune system reacts to a substance as if it were harmful, triggering a range of symptoms. While allergic reactions to methocarbamol are relatively rare, it’s important to be aware of the possibility. If you experience any signs of an allergic reaction after taking methocarbamol, such as rash, itching, swelling (particularly of the face, tongue, or throat), severe dizziness, or difficulty breathing, it is crucial to seek immediate medical attention. Allergic reactions can be serious and may require prompt medical intervention.
If you have a known allergy to methocarbamol or any other medications, it’s important to inform your healthcare professional before starting methocarbamol or any other treatment. They can evaluate the potential risks and benefits and determine if an alternative medication or approach is necessary. If you develop an allergic reaction to methocarbamol or suspect that you may be experiencing one, it’s important to discontinue the medication and seek medical attention promptly. Your healthcare professional will be able to provide appropriate guidance and treatment to manage the allergic reaction effectively.
What should I do if I forget a dose of the methocarbamol drug?
If you forget to take a dose of methocarbamol, here are some general guidelines to follow:
- Read the Instructions: Refer to the medication packaging or the instructions provided by your healthcare professional for specific guidance on missed doses. Different formulations and dosing schedules may have different recommendations.
- Timing: If you remember that you missed a dose close to the time you were supposed to take it, take the missed dose as soon as possible. However, if it is already close to the time for your next scheduled dose, it is generally recommended to skip the missed dose and continue with your regular dosing schedule. Taking two quantities close together can improve the chance of side effects.
- Do Not Double Dose: Do not take a double dose to make up for the missed dose unless specifically instructed to do so by your healthcare professional. Taking more than the prescribed amount can increase the risk of side effects without providing any additional benefit.
- Follow Regular Schedule: Resume taking methocarbamol according to your regular schedule. It’s important to maintain a consistent dosing regimen to ensure the medication’s effectiveness.
- Set Reminders: To help prevent missing doses in the future, consider setting reminders on your phone or using pill organizers to keep track of your medication schedule.
If you are unsure about what to do or have any concerns regarding missed doses of methocarbamol, it’s best to consult with your healthcare professional or pharmacist. They can provide specific guidance based on your individual situation and treatment plan. Remember, this information is general, and it’s always important to follow the instructions provided by your healthcare professional or the medication packaging. They will provide the most accurate and personalized guidance for your specific needs.
Enhancing Healthcare Team Outcomes Methocarbamol drug
To enhance healthcare team outcomes related to the use of methocarbamol, collaboration and effective communication among healthcare professionals is crucial. Here are some ways the healthcare team can work together to optimize outcomes:
- Multidisciplinary Approach: The healthcare team may include physicians, pharmacists, nurses, and other healthcare professionals. Each member brings their expertise to ensure comprehensive patient care. Collaboration allows for a holistic assessment of the patient’s condition, consideration of potential interactions with other medications or underlying conditions, and monitoring for adverse effects.
- Patient Education: Healthcare professionals should educate patients about methocarbamol, including its purpose, dosing instructions, potential side effects, and precautions. Clear communication helps patients understand the importance of adherence to the prescribed treatment plan and allows them to report any concerns or adverse reactions promptly.
- Individualized Treatment Plans: The healthcare team should work together to develop individualized treatment plans based on the patient’s specific needs, medical history, and any underlying conditions. This includes considering factors such as renal or hepatic impairment, drug interactions, and potential contraindications.
- Medication Review: Regular medication reviews by the healthcare team can help identify any potential drug interactions, duplication of therapy, or adverse effects related to methocarbamol. This ensures that the medication remains appropriate for the patient’s condition and minimizes the risk of adverse events.
- Monitoring and Follow-up: The healthcare team should establish a monitoring plan to assess the patient’s response to methocarbamol therapy. This may involve evaluating the effectiveness of the medication in managing the symptoms, monitoring for any side effects or allergic reactions, and conducting periodic laboratory tests if necessary.
- Adverse Event Reporting: If any adverse events or unexpected reactions occur during methocarbamol treatment, healthcare professionals should report these incidents according to established procedures. Reporting adverse events helps to identify potential safety concerns and contributes to the ongoing monitoring of medication safety.
- Continuous Professional Development: Healthcare professionals should stay updated with the latest research, guidelines, and safety information related to methocarbamol. This allows them to provide the most current and evidence-based care to patients and make informed decisions regarding the use of this medication.
By working collaboratively, communicating effectively, and sharing knowledge and expertise, the healthcare team can enhance patient outcomes and ensure the safe and effective use of methocarbamol.
Expert Advice for this Methocarbamol Drug
However, it is important to note that consulting with a healthcare professional, such as a doctor or pharmacist, who has access to your complete medical history, is essential for personalized advice. Here are some general considerations and expert advice related to methocarbamol:
- Follow Prescribed Dosage: Take methocarbamol exactly as prescribed by your healthcare professional. Do not exceed the recommended dose or use it for longer than advised.
- Complete Treatment Course: Ensure that you complete the full course of treatment, even if your symptoms improve. Stopping methocarbamol abruptly may not provide optimal therapeutic benefit.
- Drowsiness and Impaired Alertness: Methocarbamol can cause drowsiness, dizziness, and impaired alertness. Avoid activities such as driving, operating machinery, or performing tasks requiring mental alert until you know how the medication affects you.
- Alcohol and Sedatives: Avoid or minimize the consumption of alcohol and other sedative medications while taking methocarbamol. Combining methocarbamol with these substances can increase the sedative effects and impair cognitive and motor functions.
- Renal or Hepatic Impairment: If you have impaired kidney or liver function, your healthcare professional may need to adjust the dosage or monitor you more closely while taking methocarbamol. Inform your doctor about any existing medical conditions or medications that could affect your kidneys or liver.
- Drug Interactions: Inform your healthcare professional about all the medications, supplements, and herbal products you are taking. Methocarbamol may interact with certain medications, including sedatives, tranquilizers, and other muscle relaxants. Your healthcare professional can assess potential interactions and adjust your treatment plan accordingly.
- Allergic Reactions: If you experience symptoms of an allergic reaction, such as rash, itching, swelling, or difficulty breathing, discontinue methocarbamol and seek immediate medical attention.
- Special Populations: Methocarbamol use in elderly individuals and children should be closely monitored due to the increased risk of adverse effects. Use in pregnant or breastfeeding women should be discussed with a healthcare professional to assess the potential risks and benefits.
- Storage and Disposal: Store methocarbamol according to the instructions on the packaging. Keep it out of reach of children and dispose of any unused or expired medication properly.
Remember, this advice is general, and individual circumstances may vary. It is essential to consult with a healthcare professional who can provide personalized advice based on your specific medical history, current medications, and needs.
Precautions to take when using this methocarbamol drug
When using methocarbamol, it is important to take certain precautions to ensure safe and effective use of the medication. The following are a couple of point-by-point precautionary measures to respect:
- Medical History: Inform your healthcare professional about your complete medical history, including any known allergies, liver or kidney disease, respiratory disorders, epilepsy, or myasthenia gravis. Methocarbamol may interact with these conditions, and your healthcare professional can assess if the medication is appropriate or if an alternative treatment option should be considered.
- Allergic Reactions: If you have a known allergy to methocarbamol or any other medications, inform your healthcare professional. Allergic reactions to methocarbamol are rare but can occur. If you experience symptoms of an allergic reaction, such as rash, itching, swelling, or difficulty breathing, discontinue the medication and seek immediate medical attention.
- Pregnancy and Breastfeeding: If you are pregnant, planning to become pregnant, or breastfeeding, discuss the use of methocarbamol with your healthcare professional. They can assess the potential risks and benefits and provide guidance on whether it is safe to use the medication in your specific situation.
- Medication Interactions: Inform your healthcare professional about all the medications you are currently taking, including prescription drugs, over-the-counter medications, and supplements. Methocarbamol may interact with certain medications, such as sedatives, tranquilizers, and other muscle relaxants. Your healthcare professional can assess potential interactions and adjust the treatment plan if needed.
- Drowsiness and Impaired Alertness: Methocarbamol can cause drowsiness, dizziness, and impaired alertness. Avoid activities such as driving, operating machinery, or performing tasks requiring mental alert until you know how the medication affects you. Alcohol and other sedatives can enhance these effects and should be avoided or minimized.
- Dosage and Instructions: Follow the recommended dosage and instructions provided by your healthcare professional or as indicated on the medication packaging. Do not exceed the prescribed dose or use the medication for longer than advised. Taking higher doses or using it for an extended period can increase the risk of side effects.
- Renal or Hepatic Impairment: If you have impaired kidney or liver function, your healthcare professional may need to adjust the dosage or monitor you more closely while taking methocarbamol. Inform your doctor about any existing medical conditions or medications that could affect your kidneys or liver.
- Elderly and Pediatric Use: Methocarbamol use in elderly individuals and children should be closely monitored due to the increased risk of adverse effects. Elderly individuals may be more sensitive to the sedative effects of the medication. Use in children should be based on the healthcare professional’s recommendation and appropriate dosing for the specific age group.
- Storage and Disposal: Store methocarbamol according to the instructions on the packaging. Keep it out of reach of children and dispose of any unused or expired medication properly, following local guidelines or medication take-back programs.
It’s important to discuss these precautions and any specific concerns with your healthcare professional. They can provide personalized advice based on your circumstances and ensure the safe and effective use of methocarbamol.
Conclusion
In conclusion, methocarbamol is a medication that belongs to the class of muscle relaxants. It is mostly used to stop muscle spasms and the pain that comes with them. Methocarbamol works by acting on the central nervous system to relax muscles and alleviate discomfort. When taking methocarbamol, it is important to follow the prescribed dosage and instructions provided by your healthcare professional. The medication is generally well-tolerated, but like any medication, it may cause side effects. Drowsiness, dizziness, and upset stomach are all common side effects. Although uncommon, serious allergic reactions can occur.
Before starting methocarbamol, it is essential to inform your healthcare professional about your medical history, including any allergies, liver or kidney disease, respiratory disorders, epilepsy, or myasthenia gravis. They can assess if the medication is appropriate for you and if any precautions or dosage adjustments are necessary. Methocarbamol may interact with certain medications, so it is important to disclose all the medications you are taking to your healthcare professional. Alcohol and other sedatives should be avoided or minimized while taking methocarbamol due to the potential for increased sedation.
If you have any concerns or experience any unusual symptoms while taking methocarbamol, it is important to consult your healthcare professional. They can direct you and address any concerns or questions you may have. Remember, this information is intended for general knowledge and is not a substitute for medical advice. Always seek individualized, condition-specific advice and recommendations from a healthcare professional.
FAQ
Is methocarbamol an effective pain reliever?
It is bound to be mishandled at higher dosages, particularly by individuals with a background marked by chronic drug use. Notwithstanding, methocarbamol doesn’t have similar properties as an opiate: It does not alleviate widespread pain. It doesn’t create a feeling of happiness or a “high.”
Who ought to avoid using methocarbamol?
Methocarbamol should not be taken by people who have been prescribed multiple central nervous system (CNS) depressants, opioids, or benzodiazepines, or by people who have a history of substance abuse.
Will methocarbamol put you to bed?
Effects on driving and concentration When you take methocarbamol, you may feel sleepy and have trouble staying focused. If you are over 65 years old or take other drowsy medications, this effect is more likely to occur. Methocarbamol should not be taken with alcohol.
Is diazepam the same as methocarbamol?
Is Robaxin the same thing as Valium? Valium (diazepam) and Robaxin (methocarbamol) are medications used to treat various conditions affecting the skeletal muscle. Valium is used to treat muscle spasms, and Robaxi is used in conjunction with rest and physical therapy to treat skeletal muscle conditions like pain or injury.
Is methocarbamol mitigating?
Are methocarbamol and ibuprofen the same thing? Ibuprofen is a medication that can be used to treat a wide range of inflammatory conditions. It isn’t equivalent to methocarbamol — it is a kind of nonsteroidal calming drug (NSAID). Ibuprofen does not contain methocarbamol, and methocarbamol does not contain ibuprofen.
What is the Indian name for methocarbamol?
Robinaxol – Khandelwal [Methocarbamol]
Is methocarbamol a drug that blocks nerves?
Uses, Dosing, and Side Effects of Methocarbamol – Drugs.com Methocarbamol is a muscle relaxant. It works by stopping nerve impulses, which are also known as pain sensations, from getting to your brain. Methocarbamol is used to treat injuries or pain in the skeletal muscles along with rest and physical therapy.
Is the brain affected by methocarbamol?
Methocarbamol: Seven things you should know: Experts at Drugs.com do not know how methocarbamol works because it does not affect the muscle directly; in any case, its belongings might be because of its calming properties or how it blocks nerve motivations to the mind