Monoarthritis
What is Monoarthritis?
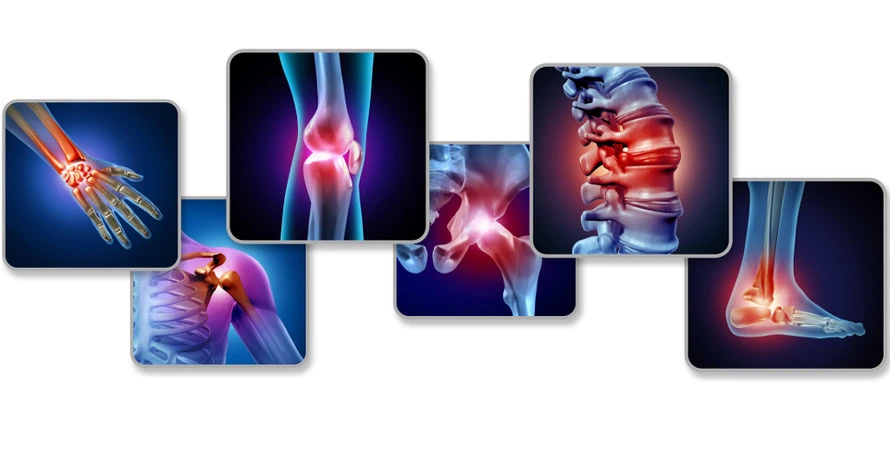
Monoarthritis, also called monoarticular arthritis, refers to joint inflammation that affects one joint ( mono joint ). Frequently, monoarthritis can appear suddenly and cause joint discomfort that ranges from moderate to severe. Later it can involve other joints of the body.
Types of Monoarthritis
Pyogenic arthritis – Pyogenic, or septic, arthritis is a serious and acheful infection of a joint. It is most often caused by bacteria, such as streptococcus or staphylococcus, but can also be caused by a virus or fungus.
Tubercular arthritis – Tuberculous arthritis is an infection of the junction due to tuberculosis (TB).
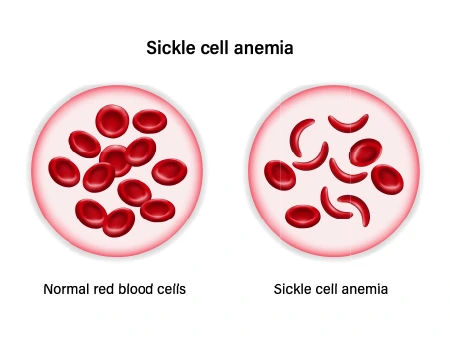
Hemophilic arthritis – Hemophilic Arthropathy is a systemic arthropathy most familiarly caused by hemophilia and characterized by repetitive hemarthroses and progressive joint problems.
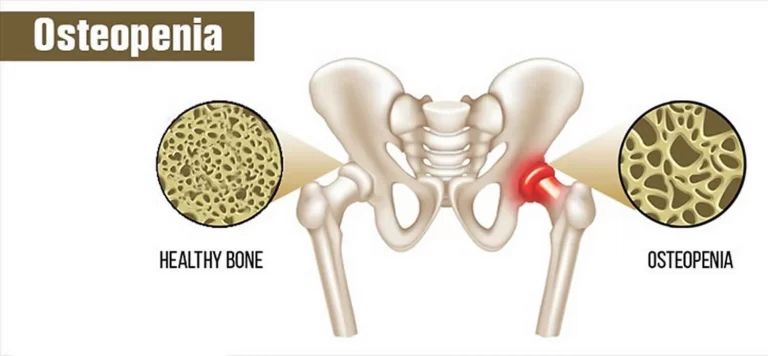
Secondary osteoarthritis – Secondary osteoarthritis happens when your cartilage is harmed by another disease or medical condition. Things that can cause it or make it more likely involve:
Obesity– puts more stress on your junctions, especially your knees. Damage or surgery to the joint.
Gout – sometimes – When your body has extra uric acid, sharp crystals may form in the junctions
Causes of monoarthritis
Monoarthritis can be a symptom of an underlying infection or another medical disease. Because there is a variety of causes, diagnosis can be challenging for doctors, as they seek to rule things out. Let’s go over some of the most general causes of monoarthritis.
Gout
Conditions that cause crystal deposits to build up in the body are the most general culprits behind monoarthritis. This usually means pseudogout and gout.
Gout happens when uric acid crystals build up in your body and start to form a deposit at a joint or junction. Your body produces uric acid when it cut down purines. These are substances found in things like red meat, alcoholic beverages, and beverages sweetened with fructose.
A gout flare can last days to weeks and often start in the big toe or a lower limb. It can cause intense aches and noticeable swelling.
Infection
Infections are also a familiar underlying cause of monoarthritis.
This can be the case in septic (or infectious) arthritis, which occurs due to an underlying infection, typically in the knees joints or hip joints (junction). In addition to aches and joint swelling, septic arthritis is often accompanied by typical signs of infection, including chills, fever, and fatigue.
Gonococcal arthritis (arthritis due to a gonorrhea infection) is the most general cause of monoarthritis in young, sexually active people.
If you have had a joint or junction replacement, infection of the areas around the replacement can also potentially cause monoarthritis. Contact your surgeon right away if you’ve had a junction replacement and are experiencing troubling aches or signs of infection. You may need treatment with drugs (antibiotics).
Other causes
- In addition to gout and septic arthritis, there are several medical conditions that can cause monoarthritis. These involve:
- Osteoarthritis
- Lyme disease, which usually affects the knee junction
- trauma due to injury
- Rheumatoid arthritis (RA), which usually occurs in smaller joints (does not involve the knees or hips)
- Ankylosing spondylitis
- Psoriatic arthritis
- Monoarthritis can occur in five to 20 percent of patients whom a doctor will later diagnose with rheumatoid arthritis.
- But a lot of the time, the above conditions affect more than one junction. Depending on the cause, it’s possible for monoarthritis to progress to inflammation in other junctions over time.
Monoarthritis symptoms
Monoarthritis tends to cause acute aches. This means the ache seems to come on suddenly, usually within hours to days.
Some monoarthritis symptoms may involve:
- Warm feeling in the joint (junction)
- Swelling
- Weakness
- The ache that usually worsens with motion
- A wider range of symptoms depends upon the underlying cause. For example, if Rheumatoid Arthritis (RA) is causing your monoarthritis, you’ll usually experience joint or junction stiffness in the morning that improves in an hour or less.
- Conditions like gout may not cause joint or junction stiffness specifically in the morning. Infections causing monoarthritis may be accompanied by chills, fever, and aches.
Diagnosing monoarthritis
Because monoarthritis can have underlying causes that are serious medical problems, it’s important you consult a medical professional or doctor. Prompt treatment can assist a case of monoarthritis from worsening or causing long-term health problems.
Questions your doctor may ask when evaluating your monoarthritis involve:
- When did the ache or discomfort begin?
- How would you describe the feeling of the joint or junction?
- Have you experienced a recent injury/accident or surgery?
- Do you have any chronic health problems?
- What drugs do you take?
- Your doctor will then likely conduct a physical examination of the affected joint (involve joint ). They’ll observe the joint or junction and move it around slowly. If you have septic arthritis (an infection), you may not be able to move the junction at all.
- Examinations may be uncomfortable, but shouldn’t cause you excessive aches. It’s more important you communicate with your doctor about how you’re feeling.
- Sometimes, your doctor may be able to recognize a cause based on your symptoms and medical history, which can especially be the case with gout.
- Other times a healthcare professional or doctor may order additional exams or tests. This may include taking a sample of synovial fluid and sending you to get blood testing or imaging, like an MRI or X-ray.
Treatment
Medication
- Treatment will depend on the etiology of monoarticular arthritis (monoarthritis ).
- Empiric antibiotics are necessary for septic arthritis based on likely etiology (cause), which will later be tailored based on synovial fluid cultures.
- Give analgesia for gout and pseudogout within 24 hours of symptom onset for better results.
- Corticosteroids, non-steroidal anti-inflammatory drugs (NSAIDs), and colchicine are equally beneficial for treating acute flares of gout and pseudogout with NSAIDs being the first line of treatment.NSAIDs are the first-line treatment with indomethacin, historically being the first-line choice, but no research exists for its superiority to other NSAIDs.
- Colchicine is another treatment solution but does not provide analgesia and is less beneficial if given beyond 72 to 96 hours after symptoms begin. It should be used with care in patients with hepatic or renal impairment, and side effects include vomiting, nausea, and diarrhea.
- Another second-line treatment for patients who cannot tolerate NSAIDs is corticosteroids.
- Caution is important when using corticosteroids with patients with diabetes mellitus (DM) as it can alter their blood glucose levels.
Physiotherapy Treatment
Walking
Walking is a low-impact form of exercise that can assist with aerobic conditioning, joint health, heart, and mood. It is essential to wear proper shoes and stay hydrated, even if the walking is not strenuous or fast. It is often sensible to walk slowly in beginning and then increase the pace when necessary. A person may want to start a walking routine on flat, even surfaces before progressing to downhill, uphill, or uneven surfaces.
Cycling

As Arthritis aggravates the risk of cardiovascular disease, it is important to keep the heart as healthy as possible. Cycling can assist improve cardiovascular function. Riding a static bike can be a safe way to get the joints moving and enhance cardiovascular fitness. A person can be supervised while riding which is a benefit for the patient. A person can also ride their bike outside to get fresh air into the environment. In addition to enhancing aerobic conditioning, cycling can decrease stiffness, build endurance, and increase range of motion and leg strength.
Flowing motions, such as tai chi and yoga
- May decrease arthritis aches
- Assist to improve strength and balance
- May decrease stress and anxiety
- Low impact
- It done by all age groups
Pilates
Pilates is a low-impact activity that can increase flexibility for enhanced junction health. It can be useful to do Pilates poses that activate the core muscles and emphasize motions that assist with stability. Pilates can be suitable for overall motion patterns, similar to tai chi and yoga. People new to Pilates should start slowly and seek guidance from a certified trainer or doctor if possible.
Water exercises

Water assists support body weight by minimizing gravity, which means that water exercises do not impact heavily on the junctions. Swimming, water aerobics, and other gentle water exercises can increase strength, range of motion, flexibility, and aerobic conditioning. They can also decrease joint stress and stiffness.
Acupuncture
Acupuncture is an old Chinese practice that uses small, thin syringes to stimulate acupuncture points on the body to enhance healing. Acupuncture for back aches involves the practitioner inserting syringes into specific trigger points on the body (e.g., lower back, hip, back of the knee). The syringes touching these points are believed to stimulate the central nervous system and may release chemicals that could assist to alleviate symptoms and relieve aches. Acupuncture is associated with significant reductions in ache intensity, improved functional mobility, and better quality of life.
Massage Therapy
Massage therapy is a therapeutic approach to ache management. A licensed massage therapist will use techniques to massage and manipulate tissues and muscles to relieve deep tension. In addition, massage therapy boosts circulation, enhancing repair and decreasing inflammation in the muscles, tissues, and junctions. Massage therapy can increase the range of motion and flexibility, alleviate aches, and improve emotional and mental well-being on a short-term basis. If you cannot see a massage therapist, you can use massage instruments and self-massage at home.
Meditation
Mindfulness-based practices such as meditation can assist the body to relax, decreasing stress. When stress is decreased, inflammation levels and tension in the body also reduce, which can provide relief for those living with back aches. Research shows that meditation can help decrease acute stress and ache response in the body. In addition to the physical advantages of meditation, many people living with chronic aches find it helpful for improving their emotional and mental health. Meditation has been proven beneficial in decreasing anxiety and depression and enhancing deeper sleep. All of these offer help to people with arthritis, enhancing their overall quality of life. There are many varieties of meditation methods. Search available apps and online instructional videos to find the right meditation method for you.
Resistance Training
Adding resistance strength training to your exercise routine allows you to target particular muscle groups while focusing on a strong core and stability. Resistance exercises can be done with body weight, thera bands, or some appropriately weighted dumbbells.
Hot and cold packs
Hot packs stimulate blood flow to the harmed area, soothing the ache, while cold packs decreased inflammation and swelling. In case no heat or ice packs are available, you can use a flannel cloth (which has specific material) and soak it in warm or cold water.
Transcutaneous Electrical Nerve Stimulation (TENS)
It restricts your nerves from sending ache messages to the brain. It uses a small electronic instrument that sends pulses to the nerve endings by creating a tingling sensation to soothe the ache.
Hydrotherapy
It uses water to release the symptoms of arthritis. Patients perform specific exercises in water with temperatures ranging from 33 to 36 degrees Celsius with the guidance of a licensed physiotherapist or doctor.

Use of braces or taping
If you have advanced spine arthritis, we might suggest taping or using special braces to assist your joints.
Complications
Septic arthritis without treatment may rapidly lead to severe complications including:
- Fibrous ankylosis
- Necrosis
- Bony erosions
- Sepsis
- Osteomyelitis
- Death
Gout can lead to :
- Tophi
- Junction damage/deformity
- Renal failure
- Kidney stones
FAQ
What can cause Monoarticular arthritis?
The major causes of acute monoarticular symptoms involve injury, osteoarthritis, crystal-induced arthritis, systemic rheumatic diseases, infection, and mechanical derangement
Is osteoarthritis monoarthritis?
Osteoarthritis is a degenerative disease generally involving the knees and hips. At the last, results from erosion of the cartilage protecting the bones from
rubbing together. Osteoarthritis is, in fact, polyarthritis, but it starts initially in one joint (mono) before the involvement of other junctions, hence, mimicking
monoarthritis.
Can Mono cause joint inflammation?
Mono usually is not serious, but few people with mono feel very tired and have an ache in their junctions that lasts for several weeks
How long is mono recovery?
Most signs and symptoms of mononucleosis ease within a few weeks, but it may be two to 3 months before you feel completely normal. The
more rest you take and the sooner you should recover. Returning to your regular schedule too soon can increase the risk of a relapse.
What is acute monoarthritis?
Acute monoarthritis is arthritis that occurs in a single junction for less than 2 to 4 weeks and is a common presenting symptom for patients in primary care and emergency settings. Diagnosis of acute monoarthritis can be difficult and outcomes range from benign and self-limiting to chronically disabling and deadly.