Rheumatoid Arthritis of Ankle and Physiotherapy Treatment
- Rheumatoid arthritis is a chronic and usually progressive inflammatory disorder of unknown etiology characterized by polyarticular symmetrical joint involvement and systemic manifestations.
- Rheumatoid arthritis (RA) is a chronic, systemic autoimmune disease that involves inflammation in the membrane lining of the joints and often affects internal organs.
- Most patients exhibit a chronic fluctuating course of a disease that can result in progressive joint destruction, deformity, and disability. RA affects between 1 and 2 million Americans. It occurs three times more often in women, and peaks at age 35 to 50 years.
Pathology of Rheumatoid Arthritis of Ankle
- RA is a systemic disease but the most characteristic lesions are seen in the synovium or within rheumatoid nodules. The synovium is engorged with new blood vessels and packed full of inflammatory cells Before RA becomes clinically apparent the immune pathology is already beginning. Raised ESR, C-reactive protein (CRP), and RF may be detectable years before the first diagnosis.
STAGE 1 – pre-clinical
- Early changes are a. Vascular congestion with new blood vessel formation Proliferation of synoviocytes c. Infiltration of the sub synovial layers by polymorphs, lymphocytes, and plasma cells.
- There is a thickening of the capsular structures, villous formation of the synovium, and a cell-rich effusion into the joints and tendon sheath.
STAGE 2 – synovial
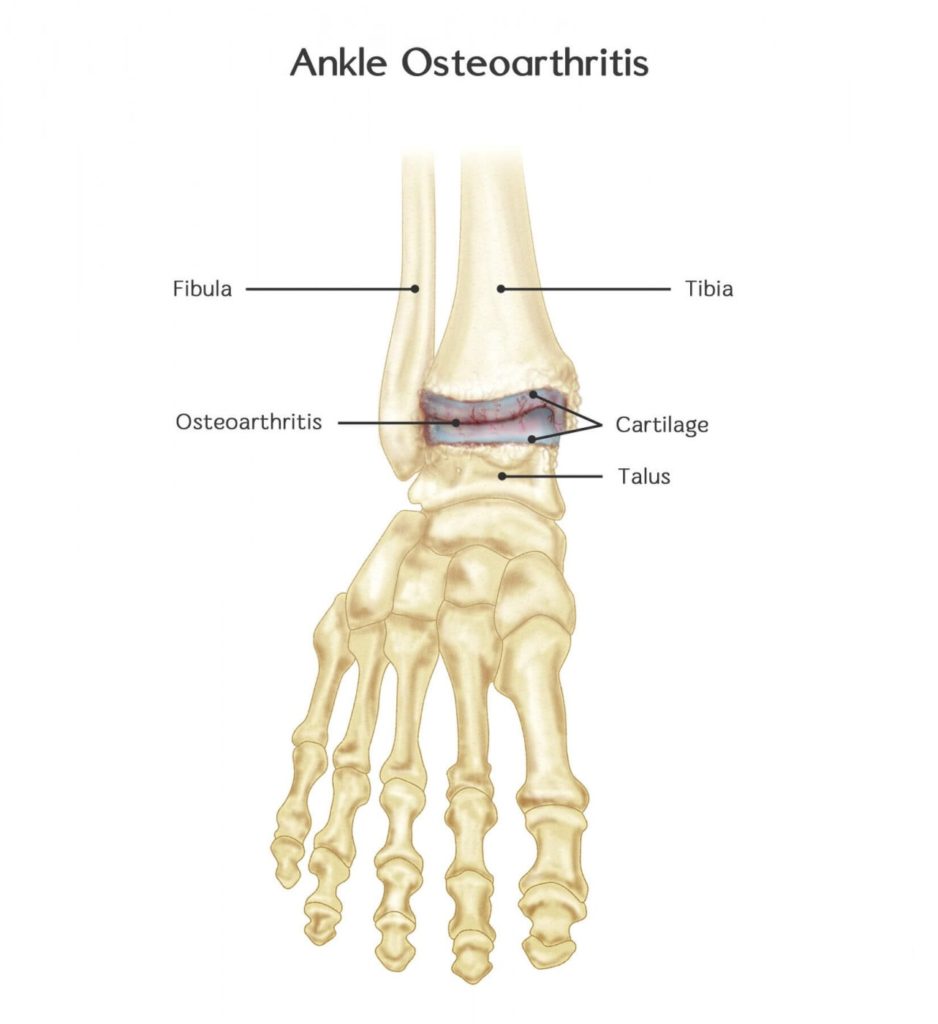
- Persistent inflammation causes joint and tendon destruction. Articular cartilage is eroded. At the margins of the joint, bone is also eroded by granulation tissue invasion and osteoclastic resorption.
- Similar changes occur in tendon sheaths, causing tenosynovitis. Partial or complete rupture of tendons. Swelling of the joints, tendons, and bursae.
STAGE 3 – destruction
- A combination of articular destruction, capsular stretching, and tendon rupture lead to progressive instability and deformity of the joints. The inflammatory process usually continues but the mechanical and functional effects of joint and tendon disruption now become vital.
Anatomy Rheumatoid Arthritis of Ankle
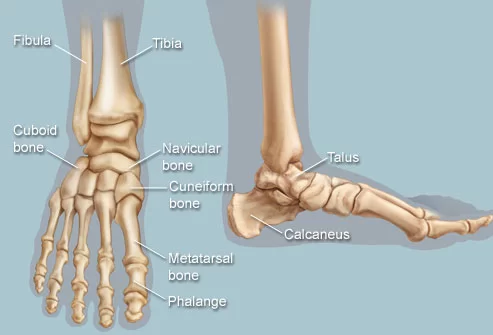
- The ankle joint is formed by three bones; the tibia and fibula of the leg, and the talus of the foot: The tibia and fibula are bound together by strong tibiofibular ligaments.
- Together, they form a bracket shaped socket, covered in hyaline cartilage. This socket is known as a mortise.
- The body of the talus fits snugly into the mortise formed by the bones of the leg. The articulating part of the talus is wedge-shaped – it is broad anteriorly, and narrow posteriorly:
- Dorsiflexion – the anterior part of the talus is held in the mortise, and the joint is more stable.
- Plantarflexion – the posterior part of the talus is held in the mortise, and the joint is less stable.
Ligaments
- There are two main sets of ligaments, which originate from each malleolus.
- Medial Ligament: The medial ligament (or deltoid ligament) is attached to the medial malleolus (a bony prominence projecting from the medial aspect of the distal tibia).It consists of four ligaments, which fan out from the malleolus, attaching to the talus, calcaneus, and navicular bones. The primary action of the medial ligament is to resist over-eversion of the foot.
- Lateral Ligament: The lateral ligament originates from the lateral malleolus (a bony prominence projecting from the lateral aspect of the distal fibula).It resists over-inversion of the foot, and is comprised of three distinct and separate ligaments:
- Anterior talofibular – spans between the lateral malleolus and lateral aspect of the talus.
- Posterior talofibular – spans between the lateral malleolus and the posterior aspect of the talus.
- Calcaneofibular – spans between the lateral malleolus and the calcaneus.
Causes of Rheumatoid Arthritis of Ankle
Important factors in the evolution of RA are:
- Genetic susceptibility
- An immunological reaction; possible involving a foreign antigen, preferentially focused on synovial tissue
- An inflammatory reaction in joints and tendon sheaths
- The appearance of rheumatoid factors in the blood and synovium
- The perpetuation of the inflammatory process
- Articular cartilage destruction
Symptoms of Rheumatoid Arthritis of Ankle
- Swelling: The toes, feet, and ankles may swell due to inflammation and a buildup of synovial fluid in the joints. Swelling is often most noticeable at the big toe joint, the ankle, and the instep. Redness, warmth, and tenderness.
- The skin over the affected joints may appear flushed and feel warm or hot to the touch. The joints may feel tender to the touch or when bearing weight. For example, because of joint changes, the fat pad at the ball of the foot may not longer offer cushion when standing and walking, resulting in tenderness and pain.
- Pain and stiffness: in the heels, balls of feet, toes, or ankles. People with rheumatoid arthritis often complain of stiffness and pain in the feet, especially in the morning or after prolonged periods of inactivity.
- Walking, climbing stairs, and even wearing shoes may become difficult. Pain and stiffness can be especially pronounced where the base of the arch meets the heel, on the inside of the ankle, and in the toes.
- Achilles tendon pain. Located at the back of the ankle, above the heel, the Achilles tendon can become inflamed and cause pain, particularly when walking uphill or squatting down.
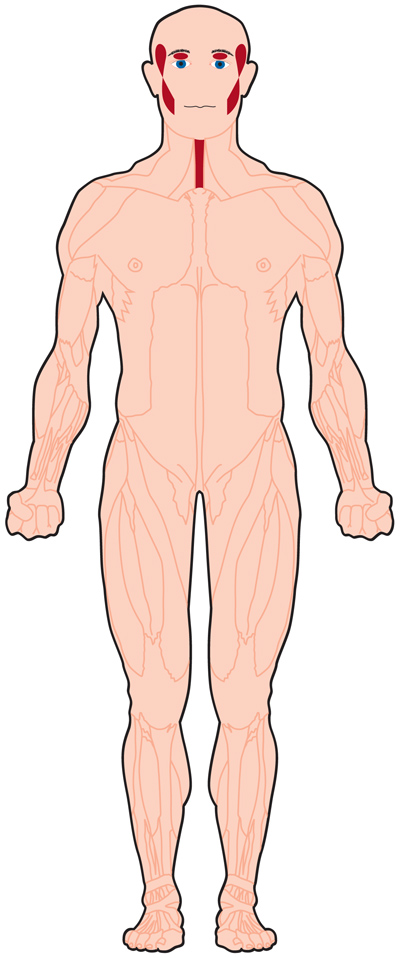
- Symmetrical inflammation. Unlike osteoarthritis, which may only affect one foot or ankle at a time, rheumatoid arthritis usually occurs to the same degree on both sides of the body.
- Malaise, fever, and fatigue: As an autoimmune disorder that affects the whole body, rheumatoid arthritis impacts more than just the bones and joints. Patients may feel tired, feverish, and general unwell during flare-ups.
- Rheumatoid nodules: These round, hard bumps often from underneath the skin in people with rheumatoid arthritis. They frequently appear on the balls of the feet, and also may appear on the sides of the feet, on the toes, or on the instep.
- Rheumatoid nodules can rub up against shoes and cause pain when walking. Some people have persistent symptoms, while others may go for long periods with no symptoms before flare-ups return. The disease progresses at different rates for different people, with some people experiencing rapid joint damage that can result in permanent foot deformity.
Diagnosis of Rheumatoid Arthritis of Ankle
Mostly clinical:
- Bilateral, symmetrical polyarthritis
- Involving proximal joints of hand or feet
- Present for at least 6 weeks
- Confirmed with subcutaneous nodules or periarticular erosions on x-ray
Investigation
1. FBC- normocytic hypochromic anemia (due to abnormal erythropoiesis from chronic inflammation), WBC
2. Inflammatory markers- ESR, CRP elevated (its use as an indication of disease progression monitoring, treatment response)
3. Rheumatoid factor(RF)- anti-IgG auto Ab 80% will have it
4. Anti- cyclic citrullinated peptide(CCP) Ab
Management of Rheumatoid Arthritis of Ankle
- There is no cure for rheumatoid arthritis, Aim to delay the progression of the disease, alleviate symptoms, reduce functional limitation. Supportive and palliative
Medication
- Disease-Modifying Antirheumatic Drugs (DMARD): There are used with NSAIDs and/or prednisolone to slow joint destruction caused by RA over time. Examples are methotrexate, injectable gold, penicillamine, azathioprine, chloroquine, hydroxychloroquine, sulfasalazine, and oral gold.
- Biologic Response Modifiers: These drugs directly modify the immune system by inhibiting proteins called cytokines, which contribute to inflammation. Examples of these are abatacept, etanercept, infliximab, adalimumab, and anakinra.
- Protein: A Immunoadsorption Therapy This is not a drug, but a therapy that filters the blood to remove antibodies and immune complexes that promote inflammation
Surgery
- Osteotomy:Literally meaning, “to cut bone,” this procedure is used to increase stability by redistributing the weight on the joint. Osteotomy isn’t often used with RA because there are other options available besides cutting the bones.
- Joint Replacement Surgery or Arthroplasty:This is the surgical reconstruction or replacement of a joint. Successfully used to help people who otherwise might be in a wheelchair, joint replacement surgery involves the removal of the joint, resurfacing and relining of the ends of bones, and replacing the joint with a man-made component.
- This procedure is usually recommended for people over 50 or who have severe disease progression. Typically a new joint will last between 20 and 30 years
- Arthrodesis or fusion: This procedure fuses two bones together. While it limits movement, it does decrease pain and increase the stability of the joints in the ankles.
Physiotherapeutic management
Principles of physiotherapy
- Relief of pain and inflammation
- Prevention of deformity
- Correction of deformity
- Restoration and maintenance of joint motion
- Improvement of muscle strength and endurance
- Guidance and training to achieve optimum function
- Education on the management of recurrence
- As the course of the disease is unpredictable, accurate assessment of the condition is a must at the time of reporting as well as at regular intervals.
Objective evaluation of the patient is carried out as follows:
- Pain: Body image pain chart and VAS
- Swelling: Volumetric measures
- Skin: Erythema, temperature, skin lesion, presence of nodules, the texture of nails and hair
- Deformity: Exact degree of deformity
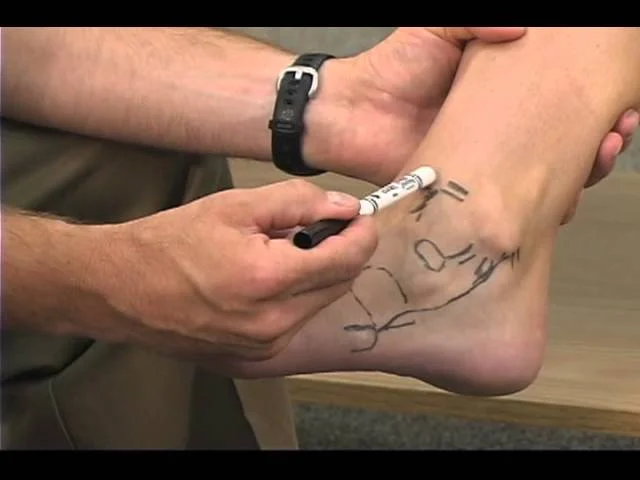
- Joint range: By goniometry
- Muscle strength and endurance of the muscles of the joints involved and the related joints
- Gait analysis
- The efficiency of performing activities of daily living (ADLs)
- Physical requirements of the vocation
- General psychological status
The type of measures adopted depends on the clinical status of the disease.
The clinical course of RA is divided into two phases:
1. Acute phase or active phase
2. Chronic phase
- The treatment differs radically in both these phases of the disease. There may be remissions and exacerbations during the course of the disease. Any form of active exercise is contraindicated during the acute phase or the acute-on-chronic phase (exacerbations).
- However, the tendency for developing tightness or contractures should be avoided. During the chronic phase, various forms of vigorous exercises are given as the pain is less. Functional training should also be intensified.
Acute phase (3–4 weeks)

- During the acute or active phase of the disease, the acute symptoms – pain, erythema, tenderness, and swelling – are present. Properly supported positioning of the involved joints and correct bed posture are important.
- The use of a firm mattress or occasional back support minimizes the effects of malpositioning and thereby preserves the integrity of the affected joints.
- The limb is placed in a position of minimal discomfort; however, contracture should be avoided. Splints and sandbags may provide additional support to the limb. Special attention is needed for the knee and elbow joints as they are prone to develop flexion contractures.
- The use of casts should be kept to the minimum. Splints or casts should be checked regularly to avoid complications due to them. Joints and muscles free from immobilization and the active disease need to be put through the full ROM and PRE.
- Functional mobility should be encouraged and maintained within the pain-free limits. Postural guidance and methods of performing activities without putting extra strain on the affected joints are taught. In cases where weight-bearing joints are involved, the upper extremities should be prepared for future crutch walking.
- Isometrics: Isometric exercises do not involve movements of the joints and are therefore relatively painless. They should be started early. Muscles like the quadriceps and deltoid are susceptible to disuse atrophy and hence need repeated sessions of isometrics.
- Other functional muscles concerned with weight-bearing and body balance need strengthening and improved endurance and thus require repetitive isometrics.
- Speedy isometrics to the affected limb in elevation reduce swelling and effusion. No heat therapy should be given to the joints that are already warm.
- TENS, pulsed ultrasound, ice massage, or ice packs for longer periods offer a reduction in muscle spasm and pain.
- The interferential current of 90–100 Hz reduces the accommodation of nerves, whereas a frequency of 50–100 Hz improves healing, blood supply, and membrane permeability by improving absorption.
- Properly guided pool therapy for the whole body provides an ideal medium for exercises.
Chronic phase

- It is a phase of vigorous activity to train the patient to use the involved joints to the greatest extent for physical independence. By 4–5 weeks of the onset, independent sitting by the use of hands can be started.
- If pain permits, active and functional therapeutic programs should be initiated. This will include standing and walking. However, weight-bearing should be deferred until pain and discomfort subside.
- Before allowing weight-bearing, it is absolutely essential to providing the necessary orthotic support or walking aid to relieve compressive forces on the affected joints. This should be done between the parallel bars to judge the effects of weight-bearing on the diseased joints.
- Sustained or intermittent stretching procedures may be necessary for the joints that have developed tightness or contractures during the acute phase. Deep heat (if acceptable), ultrasonics, TENS, and other adjuncts may be used to relieve pain.
- Efforts should be made to improve the strength and endurance of the muscles related to the affected joints.
- Education and assistance are provided in adopting functional positions, speed, and proper gait.
- Job-oriented performance should be imparted in the exercise regime.
Relapse
- Relapse is common in RA. It should be treated on the same lines as detailed for the acute phase.
Caution
- Since it is a systemic disease, it is usually accompanied by early fatigue. Therefore, exercise sessions should be brief. Ankle and foot: Maintenance of neutral position and full ROM exercises to the intrinsic muscles are important to reduce the expected deformities of the valgus foot and metatarsus valgus.
- The tendency for the deformity should be detected early and checked by varus pad in the shoe or a splint.





6 Comments