Myalgia
What is Myalgia?
Myalgia, the medical term for muscle pain, can occur as a result of various factors. Acute causes of myalgia include muscle strains, overuse, infections, and deficiencies in essential vitamins. On the other hand, chronic conditions such as fibromyalgia, rheumatoid arthritis, and depression can also lead to persistent muscle pain and soreness.
Treatment for myalgia depends on the underlying cause and may involve a combination of medications, self-care techniques, and physical therapy.
This article aims to provide a comprehensive understanding of myalgia, its potential causes, and how it can be effectively managed. Additionally, it highlights the importance of seeking medical attention when necessary and describes common approaches to treating myalgia symptoms.
What are the Symptoms of Myalgia?
Muscle pain can range from mild to severe and, in some cases, can be debilitating depending on its underlying cause. Pain is a prominent symptom often associated with chronic conditions, and the specific symptoms experienced can vary.
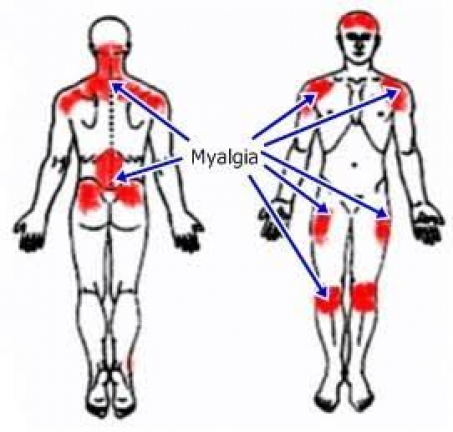
Myalgia can present as localized or widespread muscle pain. The pain itself can manifest as dull or sharp, and its intensity may range from mild to severe. Duration of pain can vary as well, with episodes lasting only a few minutes or persisting constantly. Unfortunately, the factors influencing the nature of the pain are multifaceted and depend on various factors unique to each individual.
If myalgia is caused by an infection, it may be accompanied by symptoms such as fevers or chills. Joint pain and fatigue, leading to a sense of weakness, can also be associated with myalgia. The presence of pain can contribute to feelings of depression and excessive tiredness, which are common symptoms experienced by individuals with chronic pain conditions. Additionally, myalgia may be accompanied by tenderness, swelling, or redness in the affected muscles.
Managing daily activities can become challenging for individuals who suffer from myalgia and experience these symptoms. Seeking appropriate medical attention and exploring effective treatment options can significantly improve one’s ability to engage in daily tasks and enhance the overall quality of life.
Myalgia, characterized by muscle pain, presents various symptoms that individuals may experience. These include:
- Deep muscle pain localized in a specific area or a more widespread pain sensation.
- Dull or sharp aching pain that can vary in intensity.
- Mild to severe pain that may persist for minutes or remain constant.
- Pain that is aggravated by both rest and movement.
- Muscle tenderness and swelling, akin to the sensation of a pulled muscle.
In addition to muscle pain, myalgia can be accompanied by other symptoms, which may include:
- The presence of fever and chills in cases where an infection is an underlying cause.
- Joint pain that accompanies muscle pain.
- Fatigue that hampers normal daily activities.
- Experiencing depression can occur from continued pain.
It is essential to recognize these symptoms and seek appropriate medical attention to determine the cause of myalgia and devise an effective treatment plan.
What are the Causes of Myalgia?
Myalgia often manifests as localized pain in a specific area or group of muscles. There are various common factors that can contribute to muscle pain, including stress, overuse, injuries, and tension. Additionally, systemic muscle pain, which affects multiple areas of the body, can be attributed to illnesses, infections, or certain medication side effects.
Several conditions are known to cause myalgia, including:
- Chronic fatigue syndrome
- Fibromyalgia
- Lyme disease
- Lupus
- Myofascial pain syndrome
- Rheumatoid arthritis
Moreover, there are numerous other diseases and conditions that can lead to muscle pain, such as hyperthyroidism, influenza, and dystonia.
Understanding the underlying causes of myalgia is crucial in order to properly diagnose and manage the condition. If you experience persistent muscle pain, it is recommended to consult with a healthcare professional for an accurate evaluation and appropriate treatment options.
What are the types of Myalgia?
Acute Myalgia
Acute myalgia is typically of short duration and can be effectively managed. One of the most common causes is exercise or muscle exertion.
Moreover, acute myalgia can serve as a primary symptom of various conditions, including:
- Injury/overuse: This kind of muscle pain is localized, impacting specific muscles or a small region of the body.
- Influenza: Muscle soreness often accompanies many infections, particularly during bouts of the flu.
- Lyme disease: During the early stages of this tick-borne illness, flu-like symptoms, including muscle pain, can be observed.
- Deficiencies in essential vitamins and minerals: Certain deficiencies, such as inadequate levels of vitamin D or potassium, can contribute to muscle pain.
Furthermore, myalgia can arise as a side effect of certain medications. Early recognition of such cases enables swift management through a switch to alternative medications. For instance, statins (cholesterol-lowering medications) are known to be associated with muscle pain.
Glucocorticoids, immunologic drugs, and antimicrobials can induce myopathies, which are diseases that affect muscle tissue. Abruptly discontinuing high doses of these medications can potentially trigger such myopathies.
Recognizing the underlying causes of acute myalgia is essential for appropriate management and treatment. It is advisable to consult with a healthcare professional if you experience persistent or concerning muscle pain.
Chronic Myalgia
Chronic myalgia often serves as the primary symptom in various conditions affecting the muscles and bones, as well as autoimmune diseases where the body’s immune system mistakenly attacks healthy cells.
Some examples of these conditions include:
- Fibromyalgia: This illness is described by general muscle pain, frequently accompanied by throbbing, shooting, and penetrating senses.
- Rheumatoid arthritis (RA): The inflammatory processes that affect the joints in RA can also lead to inflammation and pain in the muscles.
- Multiple sclerosis (MS): Muscle pain, stiffness, and involuntary muscle spasms are common symptoms experienced by individuals with MS.
- Depression: Physical symptoms, such as unexplained muscle aches and pains, can manifest as a result of depression.
Chronic myalgia can also be caused by various diseases or triggered by traumatic events.
Individuals with chronic myalgia conditions typically experience persistent or recurring muscle pain that affects multiple areas of the body.
It is crucial to seek medical evaluation and appropriate management strategies for chronic myalgia to improve quality of life and minimize discomfort. Consulting with a healthcare professional can help identify the underlying causes and develop an effective treatment plan.
How to Diagnose Myalgia?
Myalgia itself is not a diagnosis but rather a symptom indicating the presence of muscle pain. The process of reaching a diagnosis involves identifying an underlying condition that may have triggered the onset of muscle pain.
The diagnostic journey typically includes several steps:
- Medical history: The healthcare provider reviews your complete medical history, including past injuries, illnesses, and current medications.
- Physical examination: This involves assessing the affected area of pain, muscle tone, strength, and stiffness, as well as observing gait and posture.
- Blood tests: Blood work may reveal changes indicative of muscle damage, inflammation, or underlying conditions related to myalgia.
- Imaging: X-rays and magnetic resonance imaging (MRI) scans can be utilized to diagnose or rule out certain causes of myalgia.
In addition to these general diagnostic procedures, condition-specific testing may be conducted based on the suspected underlying condition. For instance, autoimmune diseases may require specific blood tests to identify relevant antibodies and genes. Nerve conduction studies can be employed to evaluate the functionality of nerves supplying the muscles, aiding in the diagnosis of conditions like myositis, which involves muscle tissue inflammation and degeneration.
Some muscle conditions, such as fibromyalgia, may not be easily confirmed or ruled out through blood work or imaging alone. In such cases, the healthcare provider relies on a thorough evaluation of symptoms and the exclusion of other conditions to reach a diagnosis.
A comprehensive diagnostic approach assists in identifying the underlying cause of myalgia, facilitating appropriate treatment planning and management of the condition.
What are the Treatments of Myalgia?
Muscle pain resulting from overuse or injury can be alleviated by giving the body ample rest and taking over-the-counter pain relievers or nonsteroidal anti-inflammatory drugs (NSAIDs). Applying ice and heat alternately within the first 24-72 hours can help reduce pain, inflammation, and muscle tension.
For myalgia provoked by overuse and illnesses such as fibromyalgia, methods like massage therapy and soft stretching exercises can deliver comfort. However, if the pain persists for more than three days, it is advisable to consult a doctor for further evaluation and guidance.
When muscle pain is akin to a strain or pulled muscle due to an activity, the recommended at-home treatment approach is R.I.C.E. therapy:
- Rest: Take a rest from everyday actions.
- Ice: Apply ice to the affected area at 10-minute intervals throughout the day.
- Compression: Utilize a compression bandage to decrease swelling.
- Elevation: Elevate the affected area to help reduce swelling.
Home remedies are often effective for managing acute myalgia. Some strategies to relieve acute muscle pain include resting the affected area, taking over-the-counter pain relievers like ibuprofen or acetaminophen, applying ice and heat alternately, gently stretching muscles, avoiding high-impact activities until the pain subsides, and practicing stress relief exercises such as yoga or meditation to alleviate muscle tension.
For chronic myalgia, physical therapy is a common treatment approach. It can improve flexibility in sore muscles and strengthen surrounding tissues. Additionally, a physical therapist can provide guidance on stress management techniques and ergonomic adjustments to minimize the risk of injury in the workplace and at home.
In some cases, healthcare providers may prescribe medications to manage chronic myalgia. Over-the-counter pain relievers are often effective for myalgia resulting from overuse. Prescription medications, such as certain anti-seizure drugs (e.g., pregabalin) or antidepressants (e.g., duloxetine), may be beneficial for fibromyalgia. Injections of pain medications or anti-inflammatory drugs directly into the affected area can also be used to reduce pain.
Treatment for myalgia related to autoimmune diseases focuses on managing systemic inflammation. Medications like corticosteroids may be prescribed based on the specific condition to help alleviate symptoms.
It is important to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan for myalgia, taking into account the underlying cause and individual circumstances.
Physical Therapy Management for Myalgia
An explanation of the disorder should be provided, helping patients understand the underlying causes and mechanisms of myalgia. This knowledge empowers them to recognize that their pain is real, while also reassuring them that it does not necessarily indicate further harm or damage. By addressing their concerns and providing accurate information, healthcare professionals can alleviate anxiety and prevent excessive catastrophizing.

Activity management is crucial in managing myalgia. Patients should be encouraged to practice pacing, self-monitoring, and taking regular rest breaks. By avoiding activities that could exacerbate their symptoms and setting realistic activity goals, individuals can prevent flare-ups and maintain a functional level of activity.
Relaxation techniques play a vital role in reducing pain symptoms and improving overall well-being. Patients should be advised to minimize environmental stressors, engage in deep breathing exercises, adopt healthy and active lifestyle habits, prioritize adequate sleep, and consider a therapeutic massage or other relaxation strategies. These practices can have a positive impact on their pain perception and help manage their condition more effectively.
Aerobic and Resistance Exercise

According to the evidence-based clinical practice guidelines from the Ottawa Panel (2008), managed light aerobic training and strength exercise are highly suggested for controlling chronic pain, involving myalgia. These exercises have been shown to enhance patients’ functional capacity while reducing the symptoms associated with myalgia. In particular, aerobic activity has been found to improve psychological symptoms such as depression, cognitive decline, and sleep disturbances. Exercise also promotes better cellular metabolism and respiratory capacity, increases lean muscle mass and tone, and enhances oxygen uptake within the body’s systems. Consequently, these benefits contribute to alleviating chronic pain and reducing fatigue reported by patients.
Manual/Passive Therapy
Several studies have provided support for the use of transcutaneous electrical nerve stimulation (TENS) and joint mobilizations as short-term pain relief methods in patients with myalgia. Specifically, individuals with chronic back pain attributed to myalgia may benefit from spinal manipulations, although the evidence supporting this approach is limited. There is moderate evidence indicating that passive soft tissue mobilization (STM) can be helpful in regulating pain. However, it is important to note that diffuse chronic pain presentations may be less responsive to medical management with TENS compared to localized pain. Passive therapies shouldn’t be the direct focus of myalgia medical management because of the possibility of supporting maladaptive condition opinions and managing procedures connected to pain.
Also, manual lymphatic drainage therapy & connective body tissue massage have been examined in women with myalgia. Researchers utilized the Myalgia Impact Questionnaire and the Nottingham Health Profile to assess the impact of these treatments. The findings suggest that both manual lymph drainage therapy and connective tissue massage demonstrate improvements in both the FIQ (Fibromyalgia Impact Questionnaire) and the Nottingham Health Profile scores. However, the group receiving manual lymph drainage therapy showed significantly greater improvements, suggesting that this modality may be preferable over connective tissue massage in managing myalgia symptoms.
Aquatic Therapy & Balneotherapy

Recent research has provided evidence that aquatic therapy is a well-tolerated exercise option for individuals experiencing myalgia pain. The buoyancy of the water enables patients to engage in active movement without exerting excessive energy or putting additional pressure on their joints. Moreover, studies have shown that aquatic therapy and hydrotherapy contribute to long-term improvements in the quality of life of individuals with myalgia.
Aquatic therapy can help alleviate the central hypersensitivity and pain associated with myalgia. The hydrostatic pressure exerted by the water and the soothing temperature has a positive effect on nerve endings, promoting muscle relaxation and reducing pain perception.
When considering pool temperatures for aquatic therapy sessions, it is recommended to maintain a range between 84°F and 90°F. For the general population, temperatures between 82°F and 84°F are suitable. However, for individuals with arthritic conditions, a slightly higher temperature range of 90°F to 94°F is preferred.
Likewise, an training education schedule has established a fair but important gain in the health situation of patients with myalgia and chronic overall pain, particularly in those with calmer symptoms. Compared to education alone, combining exercise and education leads to better outcomes in managing myalgia symptoms.
In addition, thermal mud baths and other balneotherapy methods have been shown to increase plasma levels of beta-endorphins, explaining their analgesic and anti-spastic effects. This finding is particularly relevant for individuals with myalgia, as it helps alleviate pain symptoms associated with the condition.
It is important to note that while these findings are based on current research, individual responses to these therapies may vary. Consulting with healthcare professionals and incorporating a comprehensive treatment plan tailored to each person’s specific needs is recommended.
Other Types of Physiotherapy Management
Occupational Therapy:

Occupational therapy interventions for myalgia focus on modifying activities to promote better management of symptoms. This may include strategies such as working at a moderate pace, incorporating frequent positional or postural changes, and taking rest breaks before fatigue sets in. Occupational therapists evaluate and adjust proper body mechanics and posture related to various activities in the patient’s daily life, including self-care, work, and leisure.
Cognitive Behavioral Therapy (CBT):
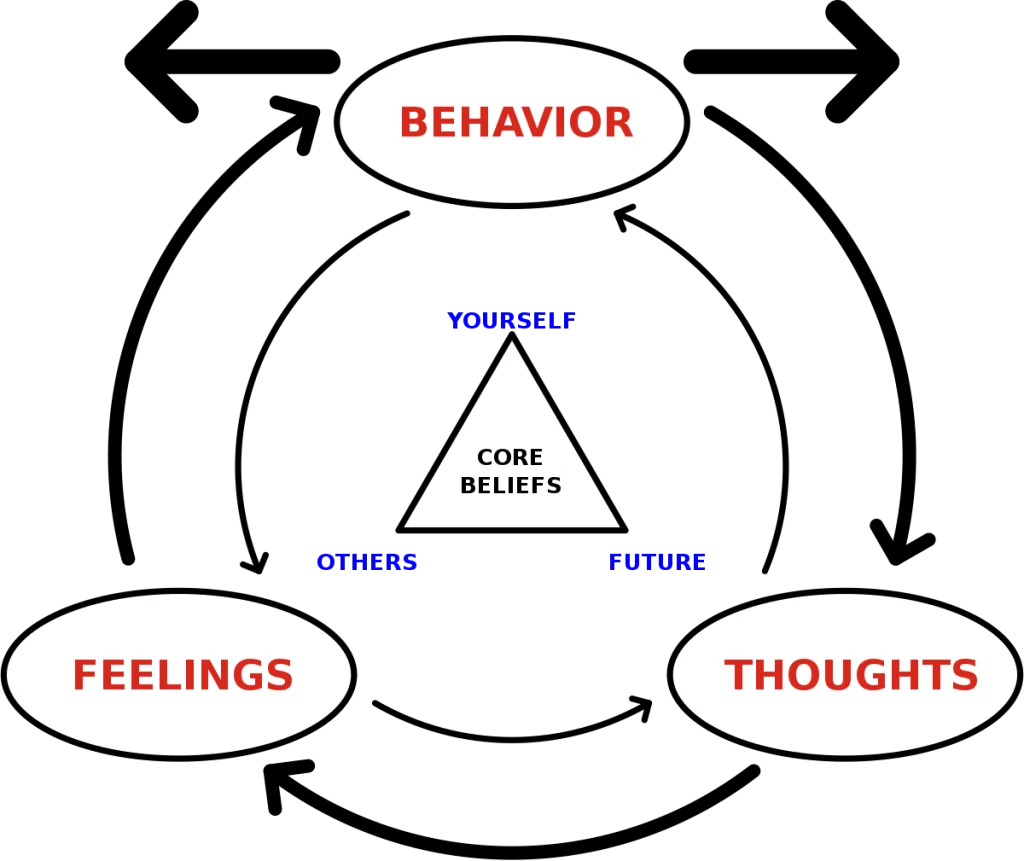
Research by Moseley has shown a relationship between pain association, beliefs, and physical performance. The evidence supports the use of cognitive behavioral therapy (CBT) as part of the assessment and treatment plan for patients with chronic pain, including myalgia. CBT has been found to improve reports of pain, reduce hyperalgesia, and modulate chronic pain-related brain responses in individuals with myalgia. Additionally, a study on behavioral insomnia therapy in myalgia patients revealed promising results, showing improvements in sleep duration and overall condition compared to other groups.
Emotional Awareness and Expression Therapy:
A group intervention focusing on emotional awareness and expression of emotions has demonstrated effectiveness in reducing pain for up to six months, surpassing the efficacy of cognitive behavioral therapy.
Chiropractic Care and Massage:
Currently, there is insufficient evidence to support the effectiveness of chiropractic care or therapeutic massage in pain management for myalgia.
Acupuncture:
Although acupuncture is commonly explored by patients for pain and fatigue relief, the existing literature provides weak evidence to support its effectiveness in managing myalgia symptoms.
It’s important to note that individual responses to these therapies may vary, and it’s advisable to consult with healthcare professionals to determine the most appropriate treatment plan based on individual needs and circumstances.
Conclusion
Myalgia is a medical word utilized to define muscle pain. It can occur as an acute, or short-term, condition, often experienced as sore muscles after intense exercise. Alternatively, myalgia can be chronic, or long-term, which may be associated with conditions like fibromyalgia.
In many cases, muscle pain can be effectively managed using at-home remedies such as rest, gentle stretching, and over-the-counter pain medication. However, when myalgia becomes chronic or significantly impacts daily life, it is advisable to seek medical attention. Healthcare providers can conduct a thorough examination, review medical history, and order diagnostic tests to determine the underlying cause of the muscle pain. This helps in developing an appropriate and personalized treatment plan for the patient. Treatment options may include medications, physical therapy, lifestyle modifications, and other interventions tailored to the specific needs of the individual.
FAQ
What autoimmune diseases cause muscle pain?
Autoimmune diseases happen when the immune system inaccurately attacks itself. A healthful immune system battles germs & conditions. Autoimmune conditions that induce muscle pain contain:
Inflammatory myopathies, for example, include body myositis and polymyositis.
Lupus.
Multiple sclerosis (MS)
What types of infections cause muscle pain?
Bacterial & viral infections can make a person sense achy all around the body. Relying on the reason, individuals may also have bulged lymph nodes, fever, and nausea. Kinds of infections that generate muscle pains contain:
Colds and flu.
Lyme illness & Rocky Mountain spotted fever (infections circulated via tick bites).
Malaria.
Trichinosis (a foodborne illness).
What types of injuries cause muscle pain?
When a person frequently utilizes the same muscles at work or while exercising, a person may originate sore muscles from overuse. Other kinds of damage that generate sore muscles contain:
Abdominal strains.
Back strains and sprains.
Broken bones and traumatic injuries.
Myofascial pain syndrome from repetitive movements (overuse).
Tendinitis.
Tendinosis.
What medications cause muscle pain?
Specific medications and cures can induce temporary/chronic pain. Medicines generate swelling over muscle cells (myositis) and activate muscle pain receptors. These medications include:
Cancer therapies, involving chemotherapy & radiation therapy.
Hypertension drugs, like angiotensin-converting enzyme (ACE) inhibitors.
Statins to lower cholesterol levels.
What other conditions cause muscle pain?
Other circumstances that even induce muscle pain contain:
Cancers, like sarcomas (soft tissue cancers) & leukemia (blood cancer).
Chronic fatigue syndrome.
Compartment syndrome (a buildup of stress in muscles).
Fibromyalgia.
Imbalance of electrolytes (minerals in the blood, for example, calcium, magnesium, sodium, and potassium).
Hypothyroidism (underactive thyroid).
Peripheral artery disease (PAD).
Stress and tension.






5 Comments