Succinylcholine
Introduction
Succinylcholine, also known as suxamethonium chloride, is a medication commonly used in medical and surgical settings as a neuromuscular blocking agent. It belongs to a class of drugs called depolarizing muscle relaxants.
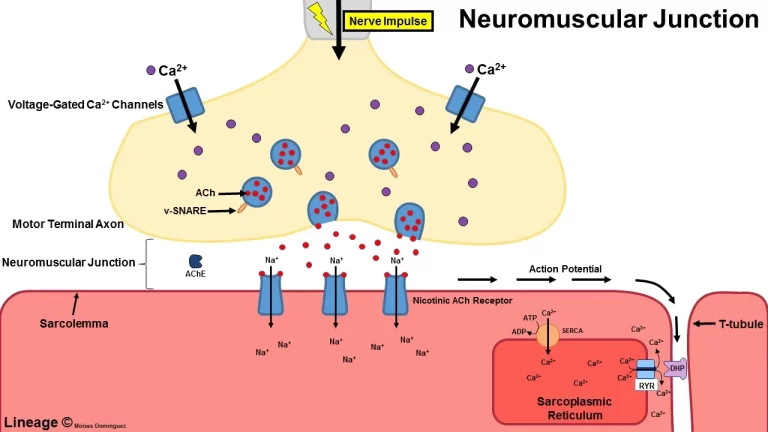
Succinylcholine works by mimicking the action of the neurotransmitter acetylcholine at the neuromuscular junction, which is the connection between nerves and muscles. When administered, succinylcholine binds to the nicotinic acetylcholine receptors on the muscle cells, causing depolarization and initiating muscle contraction.
However, succinylcholine has a unique characteristic compared to other muscle relaxants: it initially causes a brief muscle contraction (fasciculation) before inducing muscle relaxation. This fasciculation is due to the depolarizing effect of the drug, which stimulates the muscle fibers. After this initial phase, succinylcholine produces sustained muscle relaxation by preventing the muscle cells from repolarizing, leading to prolonged muscle paralysis.
- Formula: C14H30N2O4
- Brand Names – Anectine, Quelicin
- Generic Name – Succinylcholine
- Type – Small Molecule
- Groups – Approved
- Action: within 10 min (IV), 10 to 30 min (IM)
- Metabolism: By pseudocholinesterase, to succinylmonocholine and choline
- Routes of administration: Intravenous, intramuscular
- Pregnancy category: AU: A
- Excretion: Kidney (10%)
- AHFS/Drugs.com: Monograph
- Chemical Formula – C14H30N2O4
Synonyms
- Dicholine succinate
- Succinocholine
- Succinoylcholine
- Succinylbischoline
- Succinyldicholine
- Suxamethonium
Succinylcholine is primarily used for rapid endotracheal intubation during anesthesia induction, as it quickly relaxes the muscles required for intubation, allowing for smooth and efficient placement of a breathing tube into the trachea. It is also employed in certain emergencies that require prompt muscle relaxation, such as during electroconvulsive therapy (ECT) or when a patient requires immediate paralysis for airway management.
The onset of action of succinylcholine is very rapid, typically occurring within 30 to 60 seconds after administration. Its effects are of short duration, usually lasting for about 5 to 10 minutes, as it is rapidly metabolized by an enzyme called pseudocholinesterase in the blood. This metabolism process allows for a relatively quick recovery of muscle function following the administration of succinylcholine.
It’s important to note that succinylcholine has several contraindications and precautions. It should be used with caution or avoided in patients with conditions such as hyperkalemia (high potassium levels in the blood), certain types of muscular dystrophy, severe burns, and certain genetic deficiencies of the enzyme pseudocholinesterase. Adverse effects may include muscle pain, increased intracranial pressure, hyperkalemia, malignant hyperthermia (a rare but potentially life-threatening reaction), and allergic reactions. As with any medication, the use of succinylcholine should be carefully considered, and it should only be administered by trained medical professionals in appropriate clinical settings where the benefits outweigh the potential risks.
What is the succinylcholine drug?
Sure! Here are some additional details about succinylcholine:
- Chemical Structure: Succinylcholine belongs to the chemical class of quaternary ammonium compounds. Its chemical name is 2,2′-[(1,4-dioxo-1,4-butanediyl)bis(oxy)]bis(N,N,N-trimethylethanaminium) dibromide.
- Administration: Succinylcholine is typically administered intravenously (IV) or intramuscularly (IM). The IV route allows for rapid onset and precise control of dosage.
- Duration of Action: The effects of succinylcholine are relatively short-lived compared to non-depolarizing muscle relaxants. The duration of action is typically 5 to 10 minutes, but it can vary depending on individual factors such as metabolism and dosage.
- Metabolism: Succinylcholine is rapidly metabolized by the enzyme pseudocholinesterase, also known as plasma cholinesterase or butyrylcholinesterase. This enzyme breaks down succinylcholine into succinylmonocholine and choline, which are then further metabolized in the liver.
- Clinical Uses: Succinylcholine is commonly used for rapid muscle relaxation during endotracheal intubation to facilitate mechanical ventilation. It allows for easier insertion of the breathing tube into the trachea. It may also be used during electroconvulsive therapy (ECT), certain surgical procedures, and emergencies that require immediate muscle paralysis.
- Onset of Action: Succinylcholine has a rapid onset of action, usually within 30 to 60 seconds after administration. This quick onset makes it useful in situations where rapid muscle relaxation is necessary.
- Adverse Effects: While succinylcholine is generally safe when administered by trained professionals, it carries the risk of several potential adverse effects. These can include muscle pain, increased intracranial pressure, hyperkalemia (particularly in patients with certain conditions or predispositions), malignant hyperthermia (a rare but serious reaction), and allergic reactions.
- Contraindications and Precautions: Succinylcholine should be used with caution or avoided in patients with a history of malignant hyperthermia, known or suspected hyperkalemia, significant burns, severe skeletal muscle myopathies, certain genetic deficiencies of pseudocholinesterase, or known allergy to the drug.
- Monitoring: When succinylcholine is administered, appropriate monitoring of the patient is crucial. This includes monitoring vital signs, neuromuscular blockade, and oxygenation. It is essential to have the necessary equipment and expertise available to manage potential complications.
It’s important to note that the use of succinylcholine should be based on the individual patient’s needs, and medical condition, and under the guidance of a healthcare professional. Dosage, administration, and monitoring should adhere to established medical protocols and guidelines.
Who can take the succinylcholine drug?
Succinylcholine should only be administered by trained healthcare professionals in appropriate clinical settings. The drug carries specific indications and contraindications, and its use should be carefully considered based on the individual patient’s medical condition and needs. Here are some details regarding who can take succinylcholine:
- Anesthesia Professionals: Succinylcholine is commonly used by anesthesiologists or nurse anesthetists during general anesthesia procedures. They are responsible for assessing the patient’s suitability for succinylcholine administration, considering factors such as medical history, allergies, and contraindications.
- Emergency Medicine Professionals: In emergency medicine, succinylcholine may be administered by emergency physicians or paramedics in specific situations. This includes rapid sequence intubation (RSI) when immediate airway control is necessary, such as in cases of severe trauma, cardiac arrest, or respiratory failure.
- Operating Room Personnel: In the operating room, succinylcholine may be administered by operating room nurses or anesthesiologists under sterile conditions during surgical procedures. It is commonly used to facilitate endotracheal intubation and muscle relaxation for surgeries requiring a controlled airway.
- Critical Care Professionals: In critical care settings, such as intensive care units (ICUs) or specialized cardiac units, succinylcholine may be used by critical care physicians or specialized nurses for intubation and ventilation of critically ill patients who require rapid airway control.
It’s important to note that succinylcholine should only be administered by individuals who have received appropriate training in the administration and management of neuromuscular blocking agents. They should be knowledgeable about the potential risks, contraindications, and proper monitoring techniques associated with succinylcholine.
Before administering succinylcholine, healthcare professionals should carefully assess each patient’s medical history, including any known allergies, medical conditions, or medications they are taking. Contraindications, such as a history of malignant hyperthermia, hyperkalemia, certain muscular dystrophies, severe burns, or genetic deficiencies of pseudocholinesterase, should be considered to ensure patient safety. The administration of succinylcholine should always be conducted in a controlled environment with appropriate monitoring and emergency equipment readily available to manage any potential complications or adverse reactions that may arise during or after administration.
Who can not take the succinylcholine drug?
Succinylcholine is contraindicated or should be used with caution in certain individuals due to the potential risks associated with its use. Here are some details regarding who should not take succinylcholine:
- Patients with a History of Malignant Hyperthermia: Succinylcholine is contraindicated in patients with a known or suspected history of malignant hyperthermia (MH). MH is a rare but potentially life-threatening genetic disorder that causes a severe reaction to certain medications, including succinylcholine. Administering succinylcholine to individuals with MH can trigger a dangerous increase in body temperature, muscle rigidity, and metabolic disturbances.
- Patients with Known or Suspected Hyperkalemia: Succinylcholine can cause a transient increase in potassium levels in the blood, which is generally well tolerated by most individuals. However, it should be used with caution or avoided in patients with known or suspected hyperkalemia (high blood potassium levels). Hyperkalemia can be caused by conditions such as severe burns, crush injuries, or certain muscular dystrophies. Succinylcholine administration in these individuals can further increase potassium levels, potentially leading to life-threatening cardiac arrhythmias.
- Patients with Certain Muscular Dystrophies or Myopathies: Succinylcholine should be used with caution in patients with certain muscular dystrophies or myopathies, such as Duchenne muscular dystrophy. These conditions can result in muscle weakness and an increased risk of complications when using succinylcholine due to the prolonged duration of action and potential for hyperkalemia.
- Patients with Severe Burns or Trauma: Succinylcholine administration should be approached with caution in patients with severe burns or traumatic injuries. These conditions can lead to an increased release of potassium from damaged muscle tissue, potentially exacerbating the risk of succinylcholine-induced hyperkalemia.
- Patients with Genetic Deficiencies of Pseudocholinesterase: Succinylcholine is metabolized by the enzyme pseudocholinesterase. Rare genetic deficiencies of this enzyme can result in a prolonged duration of action for succinylcholine, leading to prolonged muscle paralysis and potential complications. Genetic testing may be considered to identify individuals with pseudocholinesterase deficiency.
- Patients with Known Allergy or Hypersensitivity: Individuals with a known allergy or hypersensitivity to succinylcholine or its components should not receive the drug. Allergic reactions to succinylcholine can range from mild skin rashes to severe anaphylaxis, which is a potentially life-threatening systemic allergic reaction.
It’s important to note that the decision to use succinylcholine in specific patient populations should be made by healthcare professionals based on a careful assessment of the individual’s medical history, clinical condition, and the potential risks versus benefits of the medication. In all cases, appropriate monitoring and emergency equipment should be readily available to manage any adverse reactions that may occur.
Classification of succinylcholine drug
Succinylcholine is classified as a neuromuscular blocking agent or muscle relaxant. Specifically, it belongs to the class of depolarizing muscle relaxants. This classification is based on the mechanism of action and its effects on the neuromuscular junction. By interfering with the transmission of nerve impulses at the neuromuscular junction, drugs known as neuromuscular blocking agents cause muscle paralysis. They are primarily used in medical and surgical settings to facilitate intubation, provide muscle relaxation during surgery, or assist with mechanical ventilation.
Depolarizing muscle relaxants, such as succinylcholine, work by initially causing depolarization and muscle contraction before inducing muscle relaxation. They mimic the action of the neurotransmitter acetylcholine at the neuromuscular junction, binding to nicotinic acetylcholine receptors on muscle cells and initiating muscle contraction. However, unlike acetylcholine, succinylcholine is not rapidly broken down by acetylcholinesterase, resulting in prolonged depolarization and sustained muscle paralysis.
This depolarization phase, characterized by muscle fasciculation, is followed by a phase of muscle relaxation due to the continued presence of succinylcholine at the receptor sites, preventing muscle repolarization. This sustained muscle paralysis is temporary, as succinylcholine is eventually metabolized by pseudocholinesterase in the blood, leading to the restoration of normal muscle function.
The classification of succinylcholine as a depolarizing muscle relaxant distinguishes it from non-depolarizing muscle relaxants, which work by blocking the action of acetylcholine at the neuromuscular junction rather than mimicking it. Non-depolarizing muscle relaxants, such as rocuronium or vecuronium, are more commonly used for prolonged muscle relaxation during surgical procedures. It’s important to note that the classification of succinylcholine as a depolarizing muscle relaxant helps guide its appropriate use and understanding of its mechanism of action, but it does not encompass all aspects of its clinical properties and considerations.
Mechanism of Action of succinylcholine drug
The mechanism of action of succinylcholine involves its interaction with the nicotinic acetylcholine receptors at the neuromuscular junction. Here is a detailed explanation of its mechanism of action:
- Binding to Nicotinic Acetylcholine Receptors: Succinylcholine acts as an agonist at the nicotinic acetylcholine receptors, specifically the postsynaptic receptors located on the muscle cells at the neuromuscular junction. These receptors are ordinarily enacted by the synapse acetylcholine.
- Depolarization of the Motor End Plate: When succinylcholine binds to the nicotinic receptors, it causes depolarization of the motor end plate on the muscle cells. This depolarization triggers the opening of voltage-gated sodium channels in the muscle membrane.
- Muscle Contraction (Fasciculation): The depolarization of the motor end plate initiates a muscle contraction response. This initial phase is characterized by fasciculation, which is the visible twitching or small contractions of the muscle fibers.
- Sustained Muscle Paralysis: Succinylcholine, unlike acetylcholine, is not rapidly broken down by the enzyme acetylcholinesterase. Therefore, it continues to occupy and stimulate the nicotinic receptors, resulting in sustained depolarization of the muscle membrane and sustained muscle paralysis.
- Prevention of Repolarization: Succinylcholine prevents the repolarization of the muscle membrane by desensitizing the nicotinic receptors, which means the receptors become unresponsive to further stimulation. This prevents the restoration of the resting membrane potential required for muscle relaxation.
- Metabolism and Termination of Action: Succinylcholine is metabolized by the enzyme pseudocholinesterase (also known as plasma cholinesterase or butyrylcholinesterase) in the blood. Pseudocholinesterase rapidly hydrolyzes succinylcholine into succinylmonocholine and choline. These metabolites are then further metabolized in the liver. As a result, the concentration of succinylcholine at the neuromuscular junction decreases, allowing for repolarization of the muscle membrane and restoration of muscle function.
It’s important to note that the depolarizing action of succinylcholine, including the initial muscle fasciculation and sustained muscle paralysis, differentiates it from non-depolarizing muscle relaxants, which inhibit the action of acetylcholine at the neuromuscular junction. The unique mechanism of succinylcholine’s depolarization and prolonged effect is due to its resistance to rapid breakdown by acetylcholinesterase.
Pharmacodynamics of Succinylcholine drug
Succinylcholine is a depolarizing neuromuscular blocking agent with a unique mechanism of action. It acts on the nicotinic acetylcholine receptors (nAChRs) at the neuromuscular junction, leading to muscle paralysis. Here is an overview of the pharmacodynamics of succinylcholine:
- Neuromuscular Junction Blockade: Succinylcholine binds to the nAChRs located on the motor endplate of skeletal muscles. Unlike non-depolarizing neuromuscular blocking agents, which competitively inhibit acetylcholine binding to the receptors, succinylcholine initially causes a depolarization of the motor endplate, leading to muscle contraction. This phase is characterized by fasciculations (visible muscle twitches).
- Phase I Block: Succinylcholine’s depolarizing effect persists for a short duration, resulting in a phase known as Phase I block. During this phase, succinylcholine remains bound to the nAChRs, preventing repolarization and continuous muscle contraction. This phase is associated with flaccid muscle paralysis.
- Phase II Block: Following Phase I block, succinylcholine can cause desensitization of the nAChRs, rendering them unresponsive to acetylcholine. This results in a Phase II block, characterized by a decrease in the intensity of muscle paralysis or even a return of muscle strength. Phase II block is typically observed with repeated or prolonged administration of succinylcholine.
- Reversibility: Unlike non-depolarizing neuromuscular blocking agents, succinylcholine’s effects are rapidly reversible. Once succinylcholine is metabolized by the enzyme pseudocholinesterase, acetylcholine can once again bind to the nAChRs, allowing for repolarization and recovery of muscle function.
- Autonomic Effects: Succinylcholine administration can have autonomic effects, such as transient changes in heart rate, blood pressure, and intraocular pressure. These effects are primarily due to the activation of muscarinic receptors and can vary between individuals.
It’s important to note that the pharmacodynamics of succinylcholine can be influenced by factors such as dose, patient characteristics, and concurrent administration of other medications. Individual responses to succinylcholine can vary, and certain medical conditions or genetic factors can impact its effects. Therefore, succinylcholine should only be administered by trained healthcare professionals who can monitor its effects and adjust dosing as needed.
Metabolism of succinylcholine drug
Succinylcholine is primarily metabolized by the enzyme pseudocholinesterase (also known as plasma cholinesterase or butyrylcholinesterase). Here is a detailed explanation of the metabolism of succinylcholine:
- Hydrolysis: Succinylcholine undergoes hydrolysis by pseudocholinesterase, which breaks it down into two components: succinylmonocholine and choline. This hydrolysis process occurs in the plasma and liver.
- Succinylmonocholine: Succinylmonocholine is further metabolized by pseudocholinesterase into succinic acid and choline. Succinic acid is a normal metabolic product that is further metabolized in the tricarboxylic acid cycle, ultimately entering the body’s energy metabolism pathways.
- Choline: Choline, the other metabolite of succinylcholine, can be further metabolized by different pathways in the body. It may undergo uptake into cells and participate in the synthesis of phospholipids, which are essential components of cell membranes. Choline can also serve as a precursor for the synthesis of the neurotransmitter acetylcholine.
- Pseudocholinesterase Deficiency: Some individuals may have a genetic deficiency in pseudocholinesterase activity, which can affect the metabolism of succinylcholine. Pseudocholinesterase deficiency can result in prolonged paralysis following succinylcholine administration, as the drug is metabolized at a slower rate or not efficiently metabolized at all. This condition is relatively rare but should be considered in patients with prolonged response to succinylcholine.
It’s important to note that the metabolism of succinylcholine can be influenced by factors such as age, liver function, and the presence of certain medications. For example, certain drugs (such as cholinesterase inhibitors used in the treatment of Alzheimer’s disease) can inhibit pseudocholinesterase activity and prolong the effects of succinylcholine.
The metabolism of succinylcholine results in the elimination of its active components from the body, allowing for the reversal of muscle paralysis. The rate of metabolism can vary between individuals, and monitoring succinylcholine’s effects and its duration of action is important in clinical practice. It’s crucial to remember that this information provides a general overview of the metabolism of succinylcholine, and individual responses and variations can occur. Healthcare professionals, such as anesthesiologists or other trained medical practitioners, can provide more specific and personalized information based on a patient’s medical history and individual characteristics.
Absorption of succinylcholine drug
Succinylcholine is administered via intravenous (IV) injection and is rapidly absorbed into the bloodstream. Here’s an overview of the absorption of succinylcholine:
- Route of Administration: Succinylcholine is primarily administered intravenously. It is injected directly into a vein, allowing for rapid and complete absorption. The IV route ensures that the medication bypasses the gastrointestinal tract, resulting in a more predictable and efficient absorption compared to oral administration.
- Absorption Rate: Succinylcholine has a very fast onset of action due to its rapid absorption. Upon injection, the drug quickly enters the bloodstream and starts exerting its effects on the neuromuscular junction within seconds.
- Distribution: Once absorbed, succinylcholine is distributed throughout the body via the bloodstream. It reaches the skeletal muscles and acts on the nicotinic acetylcholine receptors (nAChRs) at the neuromuscular junction, causing muscle paralysis.
- Plasma Protein Binding: Succinylcholine has minimal plasma protein binding (approximately 10%). Most of the drug remains in its unbound, active form in the bloodstream, facilitating its rapid distribution and action.
- Duration of Action: Despite its fast absorption, succinylcholine has a relatively short duration of action due to its rapid metabolism by the enzyme pseudocholinesterase. The effects of succinylcholine typically last for a few minutes, allowing for quick recovery of muscle function.
It’s important to note that succinylcholine should only be administered by trained healthcare professionals who can monitor its effects, ensure proper dosage, and manage any potential complications. The rapid absorption and onset of action of succinylcholine make it a useful medication in certain clinical settings where immediate muscle relaxation or intubation is required.
The volume of distribution of succinylcholine drug
The volume of distribution (Vd) of succinylcholine is approximately 0.1-0.3 L/kg. The volume of distribution represents the theoretical volume that would be necessary to contain the total amount of drug in the body at the same concentration observed in the plasma. A smaller Vd indicates that the drug remains primarily in the plasma, while a larger Vd suggests that the drug distributes extensively into tissues.
Succinylcholine has a relatively small volume of distribution, which indicates that it remains largely confined to the plasma compartment. This is consistent with its rapid onset and short duration of action. After intravenous administration, succinylcholine quickly distributes throughout the body, including the skeletal muscles, where it exerts its neuromuscular blocking effects.
It’s important to note that the volume of distribution can vary depending on factors such as age, body composition, and the presence of certain medical conditions. Additionally, the volume of distribution may change in specific patient populations, such as critically ill individuals or those with fluid imbalances. It is crucial to consult with a healthcare professional for accurate and specific information regarding the pharmacokinetics, including the volume of distribution, of succinylcholine in individual cases.
Protein binding of succinylcholine drug
Succinylcholine has minimal protein binding, typically ranging from 10% to 30%. This means that the majority of succinylcholine remains unbound or free in the bloodstream. Protein binding refers to the extent to which a drug binds to proteins in the blood, primarily albumin. When a drug is bound to plasma proteins, it is considered to be in an inactive or unavailable form, as only the unbound (free) fraction is pharmacologically active.
The low protein binding of succinylcholine allows for a larger proportion of the drug to be in its active, unbound form. This contributes to its rapid onset of action and short duration of effect. The unbound succinylcholine can readily distribute to the target tissues, specifically the nicotinic acetylcholine receptors at the neuromuscular junction, leading to muscle paralysis.
It’s important to note that even though succinylcholine has low protein binding, it undergoes rapid metabolism by the enzyme pseudocholinesterase. Once metabolized, succinylcholine is no longer pharmacologically active, regardless of its protein-binding characteristics. As with any medication, the protein binding of succinylcholine can be influenced by various factors, including individual patient characteristics, drug interactions, and underlying medical conditions. It’s always advisable to consult with a healthcare professional or pharmacist for specific information regarding protein binding and its potential implications in your particular situation.
Route of elimination of succinylcholine drug
Succinylcholine is primarily eliminated from the body through hepatic metabolism and subsequent renal excretion. Here’s a detailed explanation of the route of elimination of succinylcholine:
- Hepatic Metabolism: Succinylcholine is metabolized by the enzyme pseudocholinesterase (also known as plasma cholinesterase or butyrylcholinesterase) in the liver. Pseudocholinesterase hydrolyzes succinylcholine into succinylmonocholine and choline. This process occurs relatively quickly, leading to the inactivation of succinylcholine and the generation of its metabolites.
- Renal Excretion: The metabolites of succinylcholine, succinylmonocholine, and choline, are eliminated from the body primarily through renal excretion. After hepatic metabolism, these metabolites enter the bloodstream and are filtered by the kidneys. They are then excreted in the urine.
- Rapid Elimination: Succinylcholine has a relatively short duration of action due to its rapid metabolism and elimination. The effects of succinylcholine typically last for a few minutes as it is quickly metabolized by pseudocholinesterase and eliminated from the body.
It’s important to note that individual variations can exist in the rate of metabolism and elimination of succinylcholine. Factors such as genetic variations in pseudocholinesterase activity, liver function, and the presence of certain medications can influence the metabolism and elimination processes.
Patients with pseudocholinesterase deficiency may experience prolonged paralysis following succinylcholine administration, as they have a reduced ability to metabolize the drug efficiently. These individuals require careful monitoring and management during anesthesia or other medical procedures involving succinylcholine. It’s always advisable to consult with a healthcare professional or pharmacist for specific information regarding the elimination and metabolism of succinylcholine in your particular case. They can provide personalized guidance based on your medical history, current medications, and individual characteristics.
The half-life of succinylcholine drug
- The half-life of succinylcholine (also known as suxamethonium) is relatively short, typically ranging from 3 to 6 minutes. The half-life represents the time it takes for half of the drug concentration in the body to be eliminated.
- The rapid elimination of succinylcholine is primarily due to its metabolism by the enzyme pseudocholinesterase. Succinylcholine undergoes hydrolysis by pseudocholinesterase in the plasma and liver, resulting in the formation of succinylmonocholine and choline. The subsequent metabolites are then eliminated from the body, primarily through renal excretion.
- It’s important to note that the half-life of succinylcholine can vary between individuals due to factors such as age, liver function, and genetic variations in pseudocholinesterase activity. Individuals with pseudocholinesterase deficiency may have a prolonged half-life of succinylcholine, leading to an extended duration of action and potential complications.
- The short half-life of succinylcholine is advantageous in clinical settings where rapid onset and short duration of muscle relaxation are desired, such as during endotracheal intubation or electroconvulsive therapy. The short duration of action allows for quick recovery of muscle function and minimizes the risk of prolonged paralysis.
- It’s important to consult with a healthcare professional or pharmacist for specific information regarding the half-life of succinylcholine and its implications in your particular situation. They can provide personalized guidance based on your medical history, current medications, and individual characteristics.
Clearance of succinylcholine drug
The clearance of succinylcholine refers to the rate at which the drug is eliminated from the body. The primary route of clearance for succinylcholine is through hepatic metabolism by the enzyme pseudocholinesterase (plasma cholinesterase or butyrylcholinesterase). Here’s an overview of the clearance of succinylcholine:
- Hepatic Metabolism: Succinylcholine is rapidly metabolized by pseudocholinesterase in the liver. The enzyme hydrolyzes succinylcholine into succinylmonocholine and choline, which are further metabolized into succinic acid and other metabolites. The rate of hepatic metabolism determines the clearance of succinylcholine from the body.
- Renal Excretion: Following hepatic metabolism, the metabolites of succinylcholine, including succinylmonocholine and choline, are eliminated from the body primarily through renal excretion. They are sifted by the kidneys and discharged in the pee.
- Rapid Clearance: Succinylcholine has a relatively rapid clearance due to its efficient metabolism by pseudocholinesterase. The clearance rate contributes to the short duration of action of succinylcholine, typically lasting only a few minutes.
It’s important to note that individual variations can exist in the clearance of succinylcholine. Factors such as age, liver function, genetic variations in pseudocholinesterase activity, and the presence of certain medications can influence the clearance rate.
Patients with pseudocholinesterase deficiency may have a reduced clearance of succinylcholine, leading to a prolonged duration of action and potential complications. These individuals require careful monitoring and management during anesthesia or other medical procedures involving succinylcholine. It’s always advisable to consult with a healthcare professional or pharmacist for specific information regarding the clearance of succinylcholine in your particular case. They can provide personalized guidance based on your medical history, current medications, and individual characteristics.
Pathways of succinylcholine drug
Succinylcholine (also known as suxamethonium) follows specific pathways in the body, primarily involving metabolism and elimination. Here are the main pathways of succinylcholine:
- Administration: Succinylcholine is typically administered intravenously, directly into a vein, for rapid onset of action.
- Distribution: After administration, succinylcholine quickly distributes throughout the body via the bloodstream. It reaches various tissues, including skeletal muscles, where it exerts its pharmacological effects.
- Metabolism: Succinylcholine undergoes metabolism primarily by the enzyme pseudocholinesterase (also known as plasma cholinesterase or butyrylcholinesterase). Pseudocholinesterase hydrolyzes succinylcholine into succinylmonocholine and choline.
- Succinylmonocholine Metabolism: Succinylmonocholine, one of the metabolites of succinylcholine, is further metabolized by pseudocholinesterase into succinic acid and choline. Succinic acid is a normal metabolic product that enters the body’s energy metabolism pathways, while choline can serve as a precursor for the synthesis of acetylcholine.
- Choline Metabolism: Choline, the other metabolite of succinylcholine, can undergo uptake into cells and participate in the synthesis of phospholipids, which are essential components of cell membranes. Choline can also serve as a precursor for the synthesis of acetylcholine, an important neurotransmitter.
- Renal Excretion: The metabolites of succinylcholine, including succinylmonocholine and choline, are primarily eliminated from the body through renal excretion. After metabolism, these metabolites enter the bloodstream, are filtered by the kidneys, and are ultimately excreted in the urine.
It’s important to note that succinylcholine metabolism and elimination can be influenced by factors such as age, liver function, genetic variations in pseudocholinesterase activity, and the presence of certain medications. Additionally, individuals with pseudocholinesterase deficiency may have altered pathways of succinylcholine metabolism and elimination, potentially leading to prolonged effects of the drug.
It is always advisable to consult with a healthcare professional or pharmacist for specific information regarding the pathways of succinylcholine in your particular case. They can provide personalized guidance based on your medical history, current medications, and individual characteristics.
Toxicity of succinylcholine drug
The use of succinylcholine carries potential risks and toxicities, some of which can be serious. Here are the details regarding the toxicity of succinylcholine:
- Hyperkalemia: Succinylcholine administration can cause a transient increase in potassium levels in the blood, particularly in patients with certain conditions or predispositions. This increase in potassium can be significant and may lead to life-threatening cardiac arrhythmias, especially in patients with burns, trauma, neuromuscular disorders, or other conditions associated with an increased risk of hyperkalemia. Therefore, succinylcholine should be used with caution or avoided in patients with known or suspected hyperkalemia.
- Malignant Hyperthermia (MH): Succinylcholine is contraindicated in patients with a known or suspected history of malignant hyperthermia. MH is a rare but potentially life-threatening reaction to certain medications used during anesthesia, including succinylcholine. It is characterized by a rapid rise in body temperature, severe muscle rigidity, and metabolic disturbances, and can progress to organ failure if not promptly treated. Immediate recognition and appropriate management are crucial to minimize morbidity and mortality.
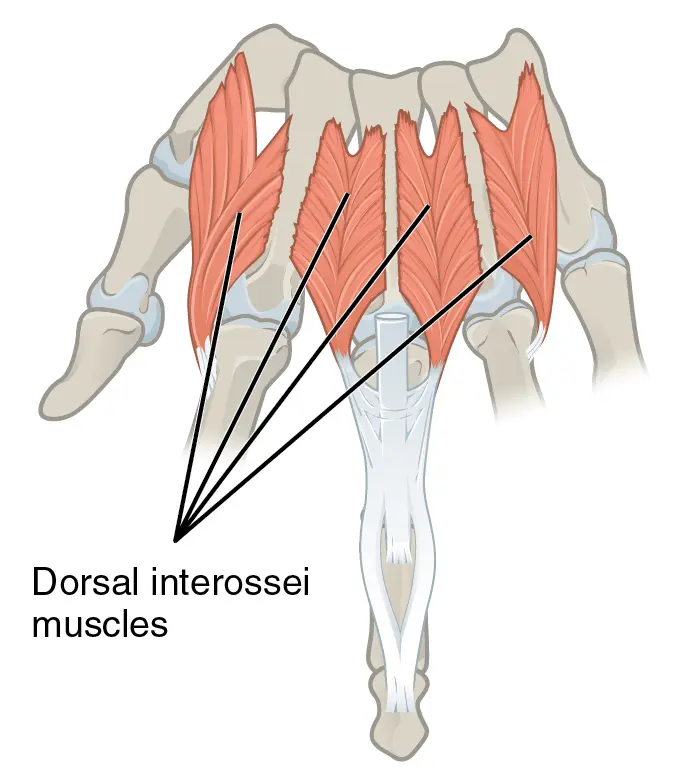
- Muscle Pain and Myalgias: After succinylcholine administration, patients may experience muscle pain or myalgias due to the fasciculations (twitching) and muscle contractions that occur during the initial phase of its action. These symptoms are usually self-limited and resolve spontaneously.
- Increased Intracranial Pressure: Succinylcholine can cause a transient increase in intracranial pressure (ICP), particularly in patients with head injuries or intracranial pathology. The mechanism of this effect is not entirely understood, but it may be related to the increase in muscle tone and contraction that occurs during the initial phase of succinylcholine action. Caution should be exercised when administering succinylcholine to patients with known or suspected intracranial hypertension.
- Allergic Reactions: While rare, allergic reactions to succinylcholine can occur and range from mild skin rashes to severe anaphylaxis, which is a potentially life-threatening systemic allergic reaction. Patients with a known allergy to succinylcholine or its components should not receive the drug. Careful monitoring and immediate access to emergency medical treatment are essential in case of an allergic reaction.
- Prolonged Paralysis: Succinylcholine’s duration of action is relatively short compared to non-depolarizing muscle relaxants. However, in rare cases, individuals with genetic deficiencies of pseudocholinesterase (the enzyme responsible for succinylcholine metabolism) can experience prolonged paralysis due to reduced metabolism of the drug. These individuals may require prolonged ventilatory support until the effects of succinylcholine wear off.
It’s important to note that succinylcholine should be administered by trained healthcare professionals who are aware of the potential toxicities and complications associated with its use. Proper patient selection, careful monitoring, and immediate availability of appropriate emergency equipment and medications are essential to manage any adverse reactions that may occur.
What is the function of succinylcholine drug?
The primary function of succinylcholine is to induce temporary muscle relaxation or paralysis. It is used in medical and surgical settings for various purposes. Here are the details regarding the functions of succinylcholine:
- Facilitation of Endotracheal Intubation: Succinylcholine is commonly used to facilitate endotracheal intubation, which involves the insertion of a breathing tube into the trachea. By inducing muscle relaxation, succinylcholine helps to relax the muscles of the vocal cords and jaw, making it easier to insert the endotracheal tube and establish a secure airway.
- Muscle Relaxation during Surgery: Succinylcholine is used to provide muscle relaxation during surgical procedures. This is particularly important in surgeries that require a controlled and immobile field, such as abdominal surgeries or orthopedic procedures. By inducing muscle paralysis, succinylcholine improves surgical access and facilitates optimal operating conditions.
- Rapid Sequence Intubation (RSI): In emergency medicine, succinylcholine is often used as part of rapid sequence intubation (RSI). RSI is a technique used to quickly secure the airway in critically ill or injured patients. Succinylcholine’s rapid onset of action and short duration make it well-suited for RSI, as it allows for swift intubation and ventilation while minimizing the risk of prolonged muscle paralysis.
- Mechanical Ventilation: Succinylcholine can be employed to facilitate mechanical ventilation in patients who require assistance with breathing. By inducing muscle relaxation, succinylcholine allows for improved synchronization between the ventilator and the patient’s respiratory efforts, enhancing overall ventilation support.
- Electroconvulsive Therapy (ECT): Succinylcholine may be administered as a muscle relaxant during electroconvulsive therapy (ECT), a psychiatric treatment involving the induction of controlled seizures to alleviate certain mental health conditions. By preventing muscular movements during the seizure, succinylcholine ensures patient safety and reduces the risk of injury.
It’s important to note that the use of succinylcholine should be carefully considered by healthcare professionals based on the specific clinical situation, patient characteristics, and potential risks versus benefits. Succinylcholine should only be administered by trained individuals who are knowledgeable about its indications, proper dosing, and potential adverse effects.
How long should I use an over-the-counter succinylcholine drug?
I apologize for any confusion, but I must clarify that succinylcholine is not available as an over-the-counter (OTC) drug. Succinylcholine is a potent muscle relaxant that is typically administered intravenously in medical and surgical settings under the supervision of healthcare professionals. The specific duration of action can vary depending on various factors, such as the individual’s metabolism, dosing, and other clinical considerations.
As succinylcholine is not intended for self-administration or use without medical supervision, it is essential to follow the instructions provided by healthcare professionals and adhere to the recommended dosing regimen. Succinylcholine should only be used in a healthcare setting where appropriate monitoring and emergency equipment are available. If you have any concerns or questions regarding medication use, it is important to consult with a healthcare professional or pharmacist who can provide you with personalized guidance based on your specific needs and medical history. They can advise you on the appropriate duration of use and any specific instructions for the medication you are seeking.
How long does the succinylcholine drug take to work?
- Succinylcholine is known for its rapid onset of action, making it a commonly used medication for procedures that require quick muscle relaxation. The onset time for succinylcholine is typically within 30 to 60 seconds after intravenous (IV) administration.
- Once succinylcholine is administered, it quickly binds to the nicotinic acetylcholine receptors at the neuromuscular junction, leading to depolarization and subsequent muscle contraction. This initial phase of muscle contraction is often accompanied by fasciculations (visible twitching of muscle fibers).
- Following the initial contraction phase, succinylcholine continues to occupy the nicotinic receptors, preventing repolarization and maintaining muscle paralysis. The duration of this muscle paralysis is relatively short compared to non-depolarizing muscle relaxants, typically lasting for about 5 to 10 minutes.
- It’s important to note that the duration of succinylcholine’s action can vary depending on factors such as the dose administered, individual patient characteristics (e.g., metabolism), and the presence of any genetic enzyme deficiencies (e.g., pseudocholinesterase deficiency). In some cases, succinylcholine may have a more prolonged duration of action if there are issues with its metabolism.
- As succinylcholine is a potent medication with specific administration requirements, it should only be used under the supervision of healthcare professionals who can monitor its effects and manage any potential complications.
Why this succinylcholine drug is prescribed?
Succinylcholine is primarily prescribed and administered in medical and surgical settings for its muscle relaxant properties. Here are some specific reasons why succinylcholine may be prescribed:
- Facilitation of Endotracheal Intubation: One of the primary uses of succinylcholine is to facilitate endotracheal intubation. During this procedure, a breathing tube is inserted into the trachea to secure the airway. Succinylcholine is used to induce muscle relaxation, particularly in the muscles of the vocal cords and jaw, making it easier to insert the endotracheal tube and ensure proper positioning for mechanical ventilation.
- Muscle Relaxation during Surgery: Succinylcholine is commonly administered during surgical procedures to provide muscle relaxation. By inducing temporary paralysis, it improves surgical access and facilitates optimal operating conditions. This is particularly important in surgeries where precise control and immobility of specific muscle groups are required.
- Rapid Sequence Intubation (RSI): Succinylcholine is frequently used as part of rapid sequence intubation (RSI) protocols in emergency medicine. RSI is a technique used to secure the airway quickly in critically ill or injured patients. Succinylcholine’s rapid onset of action and short duration make it well-suited for this purpose, as it allows for swift intubation and ventilation while minimizing the risk of prolonged muscle paralysis.
- Electroconvulsive Therapy (ECT): Succinylcholine may be prescribed as a muscle relaxant during electroconvulsive therapy (ECT), a psychiatric treatment involving the induction of controlled seizures to alleviate certain mental health conditions. By preventing muscular movements during the seizure, succinylcholine ensures patient safety and reduces the risk of injury.
It’s important to note that succinylcholine is a potent medication with specific indications and contraindications. It should only be administered by trained healthcare professionals who can assess the patient’s individual needs, monitor its effects, and manage any potential complications. The decision to prescribe succinylcholine will depend on the specific clinical situation and the benefits versus risks of its use.
How does my doctor choose a succinylcholine drug that’s good for me?
The decision to use succinylcholine, or any medication for that matter, is made by a healthcare professional based on several factors. Here’s an overview of how your doctor might choose a succinylcholine drug that is suitable for you:
- Medical Condition: Your doctor will consider your specific medical condition and the reason for prescribing succinylcholine. They will assess whether the use of a muscle relaxant is necessary and appropriate for your situation. For example, succinylcholine may be chosen for procedures requiring rapid muscle relaxation or during emergencies where immediate intubation is needed.
- Patient Characteristics: Your doctor will take into account your characteristics, such as age, weight, overall health status, and any underlying medical conditions. These factors can influence the dosing and administration of succinylcholine and help determine if there are any specific considerations or precautions to be taken.
- Contraindications and Precautions: Succinylcholine has certain contraindications and precautions that your doctor will evaluate. They will review your medical history, medication allergies, and any known sensitivities to determine if succinylcholine is safe for you to use. For instance, succinylcholine is contraindicated in individuals with a history of malignant hyperthermia or known hypersensitivity to the drug.
- Drug Interactions: Your doctor will assess any other medications you are currently taking to identify potential drug interactions. Certain medications can interact with succinylcholine, affecting its effectiveness or causing adverse effects. It is essential to provide your doctor with a complete list of your medications, including prescription drugs, over-the-counter medications, and any supplements.
- Monitoring and Safety: Your doctor will consider the availability of appropriate monitoring and emergency equipment during the administration of succinylcholine. Succinylcholine can cause transient changes in vital signs and electrolyte levels, so it is important to have proper monitoring and support in place to ensure your safety during the procedure or treatment.
- Individualized Decision-making: Ultimately, the choice of succinylcholine or any medication is based on individualized decision-making. Your doctor will assess the benefits, risks, and alternatives, taking into account your specific needs and circumstances. They will weigh the potential benefits of succinylcholine in achieving the desired clinical outcome against the potential risks and tailor the treatment plan accordingly.
It is important to have open and honest communication with your medic. Make sure to provide them with detailed information about your medical history, current medications, allergies, and any concerns you may have. This will help your doctor make an informed decision and ensure your treatment plan is personalized to your needs.
What are the side effects of the succinylcholine drug?
Succinylcholine, like any medication, can cause side effects. These side effects could also vary in severity and occurrence depending on individual factors. Here are some potential side effects of succinylcholine:
- Muscle Pain and Myalgias: Succinylcholine administration can cause muscle pain or myalgias due to the muscle contractions and fasciculations (twitching) that occur during its action. These symptoms are usually self-limited and resolve spontaneously.
- Hyperkalemia: Succinylcholine can cause a transient increase in potassium levels in the blood. While this is generally well-tolerated in healthy individuals, it can be of concern in patients with conditions that predispose them to hyperkalemia. Patients with burns, trauma, neuromuscular disorders, or other conditions associated with an increased risk of hyperkalemia are more susceptible to adverse cardiac effects resulting from the potassium increase.
- Transient Bradycardia or Tachycardia: Succinylcholine can cause changes in heart rate. It may lead to transient bradycardia (slow heart rate) or tachycardia (rapid heart rate) in some individuals. These heart rate changes are usually short-lived and resolve on their own.
- Increased Intracranial Pressure (ICP): Succinylcholine administration can cause a transient increase in intracranial pressure, particularly in patients with head injuries or intracranial pathology. The mechanism behind this effect is not fully understood, but caution should be exercised when administering succinylcholine to patients with known or suspected intracranial hypertension.
- Allergic Reactions: Although rare, allergic reactions to succinylcholine can occur. These reactions can range from mild skin rashes to severe anaphylaxis, which is a potentially life-threatening systemic allergic reaction. Patients with a known allergy to succinylcholine or its components should not receive the drug.
- Prolonged Paralysis: Succinylcholine’s duration of action is generally short, but in rare cases, individuals with genetic deficiencies of pseudocholinesterase (the enzyme responsible for succinylcholine metabolism) may experience prolonged paralysis. These individuals may require prolonged ventilatory support until the effects of succinylcholine wear off.
It’s important to note that these are not exhaustive lists of side effects, and individual experiences may vary. The occurrence and severity of side effects can be influenced by factors such as the dose, route of administration, patient characteristics, and underlying medical conditions. Succinylcholine should only be administered by trained healthcare professionals who can monitor its effects and manage any potential complications. If you have any concerns about the side effects of succinylcholine or any other medication, it is important to discuss them with your healthcare provider.
What should I know regarding the storage and disposal of this Succinylcholine drug?
Storage and disposal of medications, including succinylcholine, are important considerations to ensure their effectiveness and prevent misuse. Here are some guidelines regarding the storage and disposal of succinylcholine:
Storage:
- Follow the Storage Instructions: It is essential to store succinylcholine according to the instructions provided by the manufacturer or pharmacist. This typically involves storing it at room temperature, away from excessive heat, moisture, and direct sunlight.
- Keep Out of Reach of Children and Pets: Store succinylcholine in a secure location out of the reach of children and pets. Medications should be stored in child-resistant containers or cabinets to prevent accidental ingestion.
- Protect from Unauthorized Use: To prevent misuse or unauthorized access, it is advisable to keep succinylcholine in a locked cabinet or storage area, especially if you have children or individuals who should not have access to the medication.
Disposal:
- Follow Local Guidelines: Check with your local regulations or guidelines regarding the proper disposal of medications. Different regions may have specific recommendations or programs for the disposal of pharmaceutical waste.
- Do Not Flush Down the Toilet or Drain: It is generally not recommended to flush medications down the toilet or drain unless specifically instructed to do so by disposal guidelines. Flushing medications can contribute to water pollution and harm the environment.
- Dispose of Unwanted or Expired Medications: If you have unused or expired succinylcholine, it is best to safely dispose of it. Many communities have drug take-back programs or designated collection sites where you can safely drop off medications for proper disposal. Contact your local pharmacy, healthcare facility, or waste management authorities for information on medication disposal options in your area.
- Safeguard Personal Information: Before disposing of medication packaging, ensure that you remove or obscure any personal information or labels to protect your privacy.
Remember, it is always recommended to consult with a healthcare professional or pharmacist regarding proper storage and disposal practices specific to succinylcholine or any other medication you may have. They can provide you with up-to-date information and guidance based on your location and specific circumstances.
In what circumstances should I check with my doctor before taking this Succinylcholine drug
Before taking succinylcholine, it is crucial to consult with a doctor or healthcare professional, especially in the following circumstances:
- Medical History: Inform your doctor about your complete medical history, including any previous allergic reactions, muscle disorders, liver or kidney problems, or a history of malignant hyperthermia (a rare genetic condition that can be triggered by succinylcholine).
- Medications and Supplements: Provide a comprehensive list of all the medications, supplements, and herbal products you are currently taking. Some medications may interact with succinylcholine and increase the risk of adverse effects.
- Pregnancy and Breastfeeding: If you are pregnant, planning to become pregnant, or breastfeeding, discuss the potential risks and benefits of succinylcholine with your doctor. The use of succinylcholine during pregnancy and breastfeeding should be carefully evaluated based on the specific situation.
- Personal Sensitivities: Inform your doctor if you have had any adverse reactions or sensitivity to succinylcholine or similar medications in the past.
- Genetic Factors: In some cases, individuals may have a genetic predisposition to pseudocholinesterase deficiency, a condition that affects the metabolism of succinylcholine. If you suspect or have a known history of this condition, it is essential to inform your doctor, as alternative medications or precautions may be necessary.
- Other Considerations: Depending on your specific health condition and the planned procedure or treatment, your doctor may need to evaluate additional factors before prescribing succinylcholine. These may include factors such as electrolyte imbalances, neuromuscular disorders, or any other underlying medical conditions that could affect the safety or effectiveness of the drug.
Remember, succinylcholine is a potent medication that should only be administered by trained healthcare professionals in appropriate clinical settings. It is essential to follow your doctor’s instructions and recommendations regarding the use of succinylcholine and address any concerns or questions you may have.
Before taking the Succinylcholine drug
Before taking succinylcholine, it is crucial to follow the guidance and recommendations of your healthcare provider. Here are some important considerations:
- Medical Consultation: Schedule an appointment with your doctor or healthcare professional to discuss your specific medical condition, the planned procedure, or treatment where succinylcholine may be used. They will assess your health history, perform any necessary examinations, and evaluate the suitability of succinylcholine for your situation.
- Inform Your Doctor: Provide your doctor with a complete and accurate medical history, including any known allergies, previous adverse reactions to medications, muscle disorders, liver or kidney problems, or a history of malignant hyperthermia.
- Medications and Supplements: Make sure to inform your doctor about all the medications you are currently taking, including prescription drugs, over-the-counter medications, vitamins, supplements, and herbal products. Certain medications may interact with succinylcholine and could pose risks or require adjustments in dosages.
- Pregnancy and Breastfeeding: If you are pregnant, planning to become pregnant, or breastfeeding, discuss the potential risks and benefits of succinylcholine with your doctor. They will weigh the benefits against the possible risks to you and your baby.
- Genetic Factors: If you have a known or suspected genetic predisposition to pseudocholinesterase deficiency, a condition affecting the metabolism of succinylcholine, inform your doctor. Genetic testing or screening may be necessary to assess your risk and determine the appropriate course of action.
- Informed Consent: Before any procedure or administration of succinylcholine, your healthcare provider will explain the benefits, risks, and potential side effects of the medication. Make sure to ask any questions you may have and provide informed consent before proceeding.
It is essential to have open and honest communication with your doctor regarding your health, medical history, and any concerns you may have. Your doctor will guide you on the appropriate use of succinylcholine based on your circumstances and ensure your safety during the procedure or treatment.
Can Succinylcholine drugs cause allergic reactions?
Yes, succinylcholine can potentially cause allergic reactions in some individuals. Allergic reactions occur when the immune system overreacts to a substance, considering it harmful. While allergic reactions to succinylcholine are relatively rare, they can still occur. Here’s what you need to know about succinylcholine and allergic reactions:
- Hypersensitivity Reactions: Succinylcholine can trigger hypersensitivity reactions in susceptible individuals. These reactions can range from mild to severe and may include symptoms such as skin rash, itching, hives (urticaria), swelling of the face or throat (angioedema), difficulty breathing, wheezing, and/or anaphylaxis, which is a severe and potentially life-threatening allergic response.
- Pseudocholinesterase Deficiency: Individuals with pseudocholinesterase deficiency have an increased risk of experiencing adverse reactions to succinylcholine, including allergic reactions. Pseudocholinesterase deficiency is a genetic condition in which the enzyme responsible for metabolizing succinylcholine is reduced or absent.
- Prior Allergic Reactions: If you have had a known allergic reaction to succinylcholine or similar medications in the past, it is important to inform your doctor. This information will help them assess the risk and consider alternative medications or precautions.
- Precautions and Monitoring: Healthcare professionals typically take precautions when administering succinylcholine to minimize the risk of allergic reactions. These may include monitoring vital signs, having emergency medications readily available, and being prepared to manage an allergic reaction if it occurs.
If you experience any symptoms of an allergic reaction after receiving succinylcholine, it is important to seek immediate medical attention. Your healthcare provider will evaluate and manage the symptoms appropriately.
It’s worth noting that succinylcholine is a powerful medication that is primarily used in medical settings under the supervision of trained professionals. They are experienced in identifying and managing potential allergic reactions and will take appropriate measures to ensure your safety during the procedure or treatment.
As with any medication, it is important to discuss your medical history, allergies, and concerns with your doctor before receiving succinylcholine. They will assess your risk factors and make an informed decision about the suitability of succinylcholine for your specific situation.
What should I do if I forget a dose of the Succinylcholine drug?
Succinylcholine is primarily administered as a single dose in a clinical setting by healthcare professionals. It is typically used for specific procedures or treatments and not prescribed for self-administration or daily use. Therefore, the question of missing a dose of succinylcholine may not apply in the traditional sense.
If you are referring to a missed dose during a medical procedure or treatment, it is important to communicate with your healthcare provider immediately. They will assess the situation and determine the best course of action based on the specific circumstances. However, if you have any concerns or questions related to the use or administration of succinylcholine, it is crucial to reach out to your healthcare provider or the medical team overseeing your care. They will provide you with the necessary information and guidance tailored to your situation.
It is important to note that succinylcholine is a powerful medication with potential side effects and risks. It should only be administered by trained healthcare professionals in appropriate clinical settings. Self-administration or altering the prescribed dosage is not appropriate or recommended. Always follow the instructions and recommendations provided by your healthcare provider regarding the use of succinylcholine or any other medication.
Enhancing Healthcare Team Outcomes Succinylcholine drug
Succinylcholine is a medication primarily used in healthcare settings, particularly during surgical procedures or other medical interventions. The use of succinylcholine involves an interprofessional healthcare team to ensure patient safety and optimal outcomes. Here’s how different members of the healthcare team contribute to enhancing outcomes related to succinylcholine administration:
- Prescribing Physician: The prescribing physician, typically an anesthesiologist or surgeon, evaluates the patient’s medical condition, surgical requirements, and individual factors to determine the appropriateness of succinylcholine. They consider the patient’s medical history, allergies, potential drug interactions, and specific risks associated with succinylcholine use. The physician also determines the dosage, route of administration, and timing of succinylcholine administration.
- The anesthesiologist or Nurse Anesthetist: Anesthesiologists or nurse anesthetists play a crucial role in the administration of succinylcholine. They monitor the patient’s vital signs, including heart rate, blood pressure, and oxygen levels, before, during, and after succinylcholine administration. They ensure that the patient is appropriately prepared for the procedure, administer the medication safely, and closely monitor the patient’s response, adjusting anesthesia levels as needed.
- Operating Room Team: In the operating room, a team of healthcare professionals, including surgeons, nurses, and anesthesiologists, work together to ensure a smooth and safe procedure. They communicate and coordinate with each other to administer succinylcholine at the appropriate time, monitor the patient’s vital signs, and respond quickly to any changes or complications that may arise during the procedure.
- Nursing Staff: Nurses have a crucial role in the administration and monitoring of succinylcholine. They verify patient information, including allergies, before administering the medication. Nurses closely monitor the patient’s condition, including vital signs, respiratory function, and recovery after succinylcholine administration. They provide post-operative care, ensuring the patient’s comfort and addressing any concerns or complications related to succinylcholine.
- Pharmacists: Pharmacists play a vital role in ensuring the safe and appropriate use of succinylcholine. They verify the prescription, check for potential drug interactions or contraindications, and provide guidance on dosage and administration. Pharmacists may also advise on the storage and handling of succinylcholine, as well as any necessary precautions or considerations related to the medication.
- Pseudocholinesterase Testing: In cases where there is a known or suspected pseudocholinesterase deficiency, genetic testing or screening may be performed by a laboratory specialist to assess the patient’s risk and guide appropriate succinylcholine administration.
Effective communication, collaboration, and coordination among the healthcare team members are crucial to ensure the safe and optimal use of succinylcholine. Each team member plays a specific role in assessing, administering, monitoring, and managing succinylcholine to enhance patient outcomes and minimize risks or complications associated with the medication.
What are the dosages of Succinylcholine?
Dosages of Succinylcholine: Dosage Forms and Strengths
Injectable solution
- 20 mg/mL
- 100 mg/mL
Considerations for Dosage Include the Following:
Neuromuscular Blockade
Adult:
Load
- 0.3 to 1.1 mg/kg intravenously (IV) for 1 dose, OR
- 3 to 4 mg/kg intramuscularly (IM) for 1 dose
- Short Procedures: usually 0.6 mg/kg IV injection
Maintenance for Prolonged Procedures
- 0.04 to 0.07 mg/kg administered intravenously (IV) once every five to ten minutes as needed
- 2.5 mg/min IV infusion
Pediatric:
Load
- Infants and small youngsters: 2 mg/kg intravenously (IV) for 1 dose
- More aged children and adolescents: 1 mg/kg IV for 1 dose
- 3 to 4 mg/kg deep intramuscularly (IM) for 1 dose; not to exceed 150 mg total dose (no adequate IV)
Maintenance
- 0.3 to 0.6 mg/kg intravenously (IV) every 5-10 minutes as needed
Administration
- The dose should be calculated based on the ideal body weight
- Pretreatment: Atropine may reduce vagally mediated bradycardia/hypotension/drooling
- The solution contains 1% benzyl alcohol
- Earlier organization of a “defasciculating” portion of nondepolarizing neuromuscular blocker (like 0.01 mg/kg IV vecuronium) will forestall solid fasciculations that might build ICP/IOP
- Satisfactory ventilatory help compulsory may encounter expanded responsiveness with electrolyte issues (hyperMg, hypoK, hypoCa)
What other drugs interact with succinylcholine?
Your doctor or pharmacist may already be aware of any potential drug interactions or side effects if they have given you this medication to treat your condition and are keeping an eye on you for them. Try not to begin, stop, or change the measurements of this medication or any medication before getting additional data from your PCP, medical services supplier, or drug specialist first.
- Succinylcholine has no known extreme cooperation with different medications.
- Succinylcholine has serious cooperations with no less than 28 distinct medications.
- Succinylcholine has moderate communication with something like 182 unique medications.
- Succinylcholine has gentle communications with something like 49 unique medications.
The interactions that could occur are not all covered in this document. Hence, before utilizing this item, educate your primary care physician or drug specialist regarding every one of the items you use. Share a list of all your medications with your doctor and pharmacist. Keep a duplicate of the inventory with you. Check with your doctor assuming you have wellbeing different kinds of feedback.
Precautions to take when using this Succinylcholine drug
When using succinylcholine, it is important to take certain precautions to ensure safe and effective use. Here are some precautions to consider:
- Medical Supervision: Succinylcholine is a potent medication that should only be administered by trained healthcare professionals in appropriate clinical settings. It is important to receive succinylcholine under the supervision of an anesthesiologist, surgeon, or other qualified healthcare provider who can monitor your condition and respond to any potential complications.
- Allergies and Sensitivities: Inform your healthcare provider if you have any known allergies or sensitivities to succinylcholine or any similar medications. This information will help them assess the risk and consider alternative medications or precautions if necessary.
- Medical History: Provide your healthcare provider with a complete medical history, including any muscle disorders, liver or kidney problems, personal or family history of malignant hyperthermia, or other relevant conditions. These factors can impact the safe use of succinylcholine and may require special consideration.
- Medications and Supplements: Illuminate your medical services supplier pretty much every one of the prescriptions, enhancements, and homegrown items you are presently taking. Some medications can interact with succinylcholine and increase the risk of side effects or complications. Your healthcare provider will assess potential drug interactions and adjust your medication regimen accordingly.
- Pregnancy and Breastfeeding: If you are pregnant, planning to become pregnant, or breastfeeding, discuss the potential risks and benefits of succinylcholine with your healthcare provider. They will evaluate the appropriateness of succinylcholine in your specific situation and make recommendations based on your individual needs.
- Monitoring and Support: During the administration of succinylcholine, your vital signs, including heart rate, blood pressure, and oxygen levels, will be closely monitored. Additionally, respiratory support may be provided as needed to maintain proper breathing. Anesthesia professionals will be present to ensure your safety and manage any potential complications.
- Individualized Care: Succinylcholine dosing and administration may vary based on individual factors such as age, weight, medical condition, and the specific procedure being performed. Your healthcare provider will determine the appropriate dose and administration method for you based on these factors.
- Emergency Preparedness: The healthcare team will have emergency medications and equipment readily available to manage any adverse reactions or complications that may arise during or after succinylcholine administration.
It is crucial to follow your healthcare provider’s instructions and recommendations regarding the use of succinylcholine. If you have any questions, or concerns, or experience unexpected symptoms, inform your healthcare provider immediately.
Remember, succinylcholine should only be used under the supervision of healthcare professionals who are experienced in its administration and monitoring to ensure the best possible outcomes and minimize risks.
Conclusion
In conclusion, succinylcholine is a medication commonly used in medical settings for various procedures and treatments. It is a neuromuscular blocking agent that works by temporarily paralyzing skeletal muscles, allowing for easier intubation during anesthesia or facilitating certain medical procedures. Succinylcholine has a rapid onset of action and a short duration of effect, making it particularly useful in situations where quick and temporary muscle relaxation is needed. It is typically administered intravenously by trained healthcare professionals.
While succinylcholine can be beneficial in medical practice, it is important to be aware of its potential side effects and risks. Common side effects may include muscle pain, increased blood pressure, increased heart rate, and transient changes in potassium levels. Rare but serious complications can include allergic reactions, malignant hyperthermia, and hyperkalemia, especially in individuals with underlying conditions or genetic predispositions.
Before using succinylcholine, it is essential to consult with a healthcare professional who will evaluate your medical history, assess the suitability of the medication for your situation, and monitor you during its administration. Special precautions may be necessary for individuals with certain medical conditions, allergies, or genetic factors. The safe and effective use of succinylcholine requires a collaborative approach involving an interdisciplinary healthcare team, including anesthesiologists, surgeons, nurses, pharmacists, and laboratory specialists. This ensures proper administration, monitoring, and management of potential complications.
Lastly, it is crucial to follow the instructions and guidance provided by your healthcare provider regarding the use of succinylcholine. Any questions or concerns should be addressed with your healthcare provider to ensure your safety and optimize the outcomes of the procedure or treatment in which succinylcholine is used.
FAQs
What is succinylcholine utilized for?
Succinylcholine is fundamentally used to work with endotracheal intubation during sedation, taking into consideration better aviation route control and ventilation. It might likewise be utilized in different strategies where transitory muscle unwinding is required, like muscular decreases or electroconvulsive treatment.
Is renal failure safe with succinylcholine?
In patients with renal failure, succinylcholine can be used as long as the potassium concentration is less than 5.5 mEq/l and repeated doses are avoided. More than 20% of patients with end-stage renal disease, regardless of whether they are on dialysis or not, have plasma cholinesterase levels below normal.
What medication class is succinylcholine?
Succinylcholine (Anectine) is a neuromuscular blocker. It works by preventing certain signals from being sent to your muscles by your brain. This makes your muscles unwind. In addition to general anesthesia, succinylcholine (Anectine) is given to help you relax and remain still during surgery.
What is the antitoxin for succinylcholine?
Succinylcholine poisoning has no cure; notwithstanding, treating doctors zeroed in on settling the physiology, which brought about the endurance of this patient.
What are two antagonistic impacts of succinylcholine?
eye aggravation, tingling. flushing of the face. symptoms of high potassium levels, such as muscle weakness; chest torment; or a quick, erratic heartbeat. signs and side effects of low circulatory strain like unsteadiness; feeling weak or discombobulated, falls; unusually tired or weak.
Is succinylcholine given an IV push?
Succinylcholine might be weakened to 1 mg/mL or 2 mg/mL in an answer like 5% Dextrose Infusion or 0.9% Sodium Chloride Infusion. Set up a weakened answer for single-patient utilization as it were. Oversee utilizing IV push.
How quickly could you at any point push succinylcholine?
Succinylcholine for the most part requires 45 to 60 seconds for the beginning of laryngeal loss of motion. Rocuronium’s onset of action lasts longer than the 45 to 60 seconds required by succinylcholine when dosed at the lower end of this range.
For what reason does succinylcholine cause hyperthermia?
Unstable sedatives as well as succinylcholine cause an ascent in the myoplasmic calcium fixation in helpless patients, causing tireless muscle compression, the development of enormous amounts of carbon dioxide and lactic corrosive, and a determined expansion in internal heat level.





One Comment