Myofascial pain syndrome: Cause, Symptoms, Diagnosis, Treatment
What is Myofascial pain syndrome?
“Myo” means muscle and “fascial” means fascia. myofascial pain syndrome is a chronic pain condition that causes pain in the musculoskeletal system. This condition affects the muscles and fascia. Fascia is the thin, white connective tissue that is wrapped around all muscles. Myofascial pain is associated with trigger points in muscles.
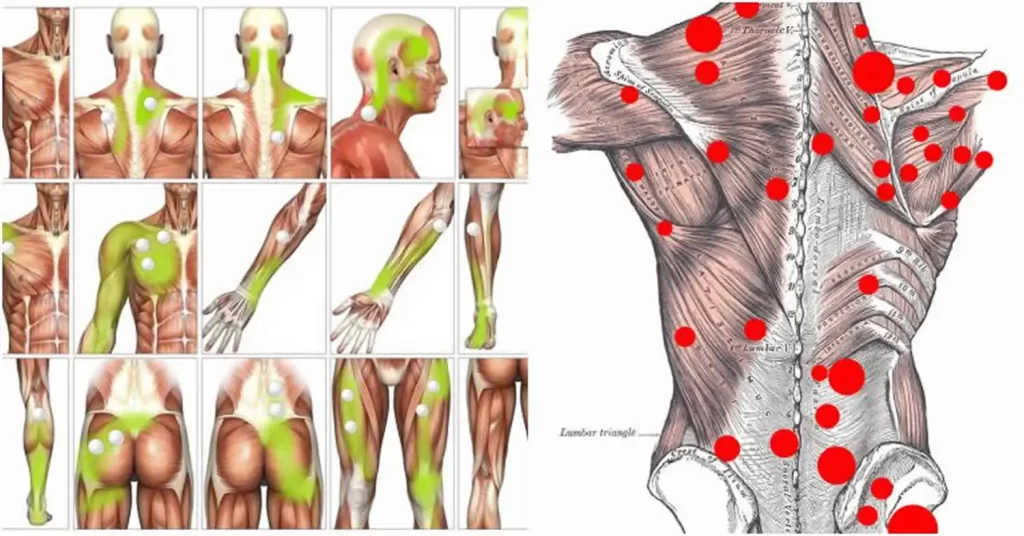
Trigger points radiate pain to the affected area when pressure on sensitive points in the muscles is applied to them and sometimes spontaneously with no pressure. and sometimes in seemingly not related body parts. This is called referred pain. The syndrome happens after repeated injury or muscle overuse. This syndrome typically occurs after a muscle has contracted repetitively. This can be caused by repetitive movements used in jobs or hobbies or by stress-related muscle tension.
Meaning of trigger points: Trigger points are discrete, focal, hyperirritable spots situated in a taut band of skeletal muscle. They produce local pain in a referred pattern and often accompany chronic musculoskeletal disorders. Acute trauma or repetitive microtrauma may cause the development of stress on muscle fibers and the formation of trigger points. Patients may have regional, persistent pain resulting in a reduced range of motion or movement in the affected muscles. These include muscles used to maintain body posture, like those in the neck, shoulders, and pelvic girdle.
Trigger points may also manifest as tension headache, tinnitus, temporomandibular joint pain, reduce or decrease range of motion in the legs, and low back pain. Palpation of a hypersensitive bundle or nodule of fiber of muscle harder than normal consistency is the physical finding normally associated with a trigger point. Palpation of the trigger point will elicit pain directly over the affected area and/or lead to radiation of pain toward a zone of reference and a local twitch response. many modalities, such as the Spray and Stretch technique, ultrasonography, Transcutaneous electrical nerve stimulation, manipulative therapy, and injection, are used to inactivate trigger points. The trigger-point injection treatment is one of the most effective treatment modalities to inactivate trigger points and provide prompt relief of symptoms.
Where does myofascial pain syndrome most commonly occur?
Myofascial pain and trigger points can be developed in any muscle of your body. the most commonly affected muscles are those in the neck, upper back, and shoulder. These muscles include the:
- Sternocleidomastoid: This largest muscle helps rotate your head to the opposite side and flexes your neck. It is Situated on the bilateral of your neck, running from your skull behind your ear area to your collarbone and breast bone.
- Trapezius: This large paired, broad, trapezoid-shaped, flat triangular back muscle tilts and turns your head and neck, shrugs and steadies your shoulders, and twists your arms. The muscle extends from the base of your skull to the middle of the back.
- Levator scapulae: This muscle is long and slender. This muscle pair of strap-like. help elevate and rotate each of your shoulder blades. They run from the first four cervical vertebrae to the top end of your shoulder.
- Infraspinatus: This triangular muscle, situated on the back side of each of your shoulder blades, helps rotate and stabilize your shoulder joints. This muscle is one of four muscles of the rotator cuff.
- Rhomboids: This muscle is paired with the upper back. these muscles draw your shoulder blades together when they contract and attach the upper limbs to your shoulder blade. rhomboid muscles run diagonally from the neck and chest vertebrae of the spine down to the back of the shoulder blades.
Myofascial pain syndrome trigger point chart
Causes of myofascial pain syndrome
- Myofascial pain syndrome’s exact cause is unknown. It may begin due to the mechanical stress on a muscle resulting in the formation of trigger points
- Myofascial pain syndrome may arise from the overuse of a muscle or trauma.
- Many factors are that could result in the formation of trigger points
- Due to injury to muscles
- The presence of inflammatory conditions
- Excessive exercise or lack of exercise
- Abnormal posture
- Muscle strain
- Repetitive muscle use (e.g. hammering) or Repetitive motions
- Muscle weakness
- Lack of muscle activity (e.g. a leg in a cast will not get enough movement, such as having a broken arm in a sling).
- Nutritional deficiencies including vitamin deficiencies
- Sleep disturbances, stress, anxiety, generalized fatigue
- Hormonal changes
- Presence of chronic infections.
- Obesity
- Frequent exposure to cold weather
- Ergonomic factors: One example is poor posture, which might be due to working at a desk all day. Another is mechanics, which may involve repeated overhead activity, such as painting a ceiling.
- Traumatic events: An event such as a car accident or sports injury may lead to this condition.
- Systemic factors and diseases: Deficiency in certain minerals or vitamins, such as iron or vitamin D, may increase a person’s risk of this syndrome. Some health conditions, like hypothyroidism, may also be risk factors.
- Structural factors: This Condition that affects the structure of the musculoskeletal system may lead to myofascial pain syndrome. Examples include:
- scoliosis
- osteoarthritis
- Working in a cold environment or living in a cold environment.
- Emotional stress (can cause muscle tension).
- Pinched nerve.
- Metabolic or hormonal problems like thyroid disease or diabetes-related neuropathy.
- Myofascial pain may develop from a muscle injury or excessive strain on a particular muscle or muscle group, ligament, or tendon.
- Injury to muscle fibers
- Excessive strain or muscle injury on a muscle or muscle group can cause this syndrome. Such injuries can lead to sensitive areas of tight muscle fiber that are called trigger points, where the myofascial pain syndrome develops.
- spondylitis
Pathophysiology of myofascial pain syndrome
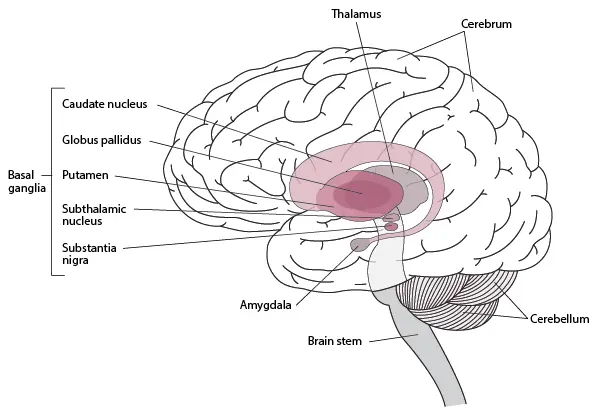
Nowadays, the exact pathophysiology of myofascial pain syndrome is still not known. Many researchers are trying to find scientific evidence and formulate hypotheses. One of the most accepted theories is the energy crisis of muscle fibers. Repetitive or prolonged activity can lead to overloading of the muscle fibers which causes muscle ischemia and hypoxia. as well as, intracellular calcium pumps are dysfunctional due to energy depletion. Intracellular calcium increase induces sustained contraction of the muscle which results in the development of taut bands. Moreover, inflammatory mediators lead to injury of the muscle and contribute to pain and tenderness of the affected muscles. Other than this hypothesis, there are many theories like neurogenic inflammation, sensitization, and limbic dysfunction that are proposed to relate to myofascial pain syndrome.
Risk factors of myofascial pain syndrome
Myofascial pain syndrome is caused by a stimulus, like muscle tightness, that sets off trigger points in your muscles. some risk factors that may increase your risk of muscle trigger points include:
- Muscle injury.:An acute muscle injury or continual muscle stress may cause the development of trigger points. For eg, a spot within or near a strained muscle may become a trigger point. Repetitive motions and not proper posture also may increase your risk.
- Stress and anxiety: People that frequently experience stress and anxiety may be more likely to develop trigger points in their muscles. One theory holds that these people could also be more likely to clench their muscles, a form of repeated strain that leaves muscles susceptible to trigger points.
- Sleep problems: Signs and symptoms of this pain syndrome may make it difficult to sleep at night. You will have trouble finding a comfortable sleep position. And if you move during the night, you might hit a trigger point and awaken.
- Fibromyalgia: Some research suggests that this pain syndrome may develop into fibromyalgia in a few people. it is a chronic condition that features widespread pain. It is believed that the brains of people with fibromyalgia become more sensitive to signals of pain over time. A few doctors believe myofascial pain syndrome may play a role in starting this process.
Symptoms of myofascial pain syndrome
- Pain that’s described as deep aching in the localized area of muscles, throbbing, tight, stiff, or vice-like.
- Pain that persists or worsens
- A tender knot in a muscle.Trigger points (a small bump, nodule, or knot in the muscle that causes pain when touched and sometimes when it’s not touched).
- Muscle pain that’s gets worsens when the affected or injured muscle is stretched or strained
- Sleep disturbances due to pain and behavioural disturbances
- Reduced or decreased range of motion in the affected areas (e.g., you may be unable to completely rotate your shoulder).
- Muscle stiffness
- Fatigue
- Headaches
- Dizziness
- Mood swings
- Muscles that are tender or sore.
- Weakness in the affected muscle(s).
- Pain that gets worse in the affected muscle or does not improve with time
- Presence of painful knots in muscles that when pressed produce intense localized or referred pain.Trigger points that activate the pain
- Postural abnormalities or affected postures such as hunching, shoulder rounding, or forward head posture (not aligned with spine)
Diagnosis of myofascial pain syndrome
Diagnosis is commonly based on the symptoms. This syndrome is often an underdiagnosed and overlooked condition. It might be mistaken for a problem with your ligaments, bones, nerves, and tendons but it is not. It is a problem with the muscles. Physicians diagnose this syndrome based on the areas of complaints of muscle pain and associated tenderness during a physical examination. Extensive laboratory testing is usually unnecessary. In addition, there are no apparent changes such as redness, unusual muscle warmth, swelling, etc. In areas of involvement. The look is the same as similar areas on the other side of the body.
During the physical examination, Your doctor will perform a physical exam to look for myofascial trigger points. your doctor may apply gentle finger pressure to the painful area of a person’s body, feeling for tense areas. Certain ways of pressing on the trigger point can elicit particular responses. Your doctor will look for tender nodules in the taut bands of your muscles and gently press them to find a pain response. Trigger points can be identified by pain. Muscle pain has many possible causes. When pressing a trigger point, your doctor will feel for a muscle twitch(also called a “jump sign”). Your doctor may recommend other tests and procedures to rule out other leads to muscle pain.
Essential criteria:
- Exquisite place of tenderness in a taut band
- The taut band is palpable, where the muscle is accessible
- Patient recognition of current pain complaint by the pressure of the examiner
- Painful limit to full stretch ROM
Confirmatory observations:
- The visual or tactile local twitch response
- Referred pain sensations are on compression of the taut band
- SEA confirmed by electromyography
There are no tests. no imaging tests or lab tests/ blood work, electromyography, or muscle biopsy that can diagnose myofascial pain syndrome.
There are four types of trigger points:
- An active trigger point: These trigger points typically lie within a muscle and pressure on it results in local or regional pain. An active trigger point is an area of severe tenderness that usually lies within the skeletal muscle and is associated with local or regional pain. Active trigger points are nodules within a taut band of muscle. They are typically the source of muscle pain. They are very tender, cause referred pain, and produce a twitch in the muscle when touched.
- A latent trigger point: It has the potential to be active, but is dormant. this trigger point is a dormant (inactive) area that has the potential to act like a trigger point. It may cause weakness of the muscle or restricted movement. These nodules do not lead to pain when touched. They can remain inactive for years and become active when there is stress or trauma.
- A secondary trigger point: This is situated in a muscle other than the one that holds the active trigger point. It could be disturbed at the same time as the active trigger point. This is a painful point in the muscle that becomes active when you stress other muscles.
- A satellite trigger point: This trigger point becomes inactive because it overlaps with the region of another trigger point. This is a painful spot that becomes active because it’s situated near another trigger point.
A visual exam to look for abnormalities in posture.
Your Physicians may ask some questions to diagnose myofascial pain syndrome.
Your Physicians may order some tests to rule out other conditions and ask you questions about your pain, including:
- Where do you feel the pain?
- How would you describe your pain?
- How often do you experience pain?
- What makes your pain better?
- What makes your pain worse?
- Have you had any recent injuries?
- Do your symptoms get well at certain times during the day?
- What does your work day look like (to look for activities in which there is muscle strain/repetitive activities or recent injuries)?
Your Physicians may check how you walk (your gait) and your posture to see if there is a balance of muscle use and look for signs of weakness of the muscles. You may also be asked about more health problems that can contribute to this syndrome including how much and how well you sleep and if you feel stressed, anxious, or depressed.
Differential diagnosis
The differential diagnosis depends on patterns and location of pain
One source of confusion related to myofascial pain is fibromyalgia. Both entities A indeed likely lead to severe muscle pain and tenderness but they do not share the same etiology or pathogenesis and their clinical presentation is not the same. Therefore two different conditions should be distinguished. Myofascial Pain and Fibromyalgia pain feel similar. Both have trigger points that give out pain.
Main differences between myofascial pain and fibromyalgia:
Myofascial Pain
- Local Pain or one specific area(or, if more than one area, those areas are typically on the same side of the body)
- Regional Condition
- Palpable of Taut Band
- Pain pattern follows a called distribution of muscular referred pain
- Restricted range of motion or slight weakness of the muscle.
Fibromyalgia
- Widespread Pain
- This pain is felt throughout the entire body.
- Fibromyalgia has more trigger points, general pain, worse fatigue and sleep issues, headaches, irritable bowel, a sensation of swelling, and sometimes burning, Prickling, or tingling feeling.
- Pain is on both sides of the body. Axial skeletal pain is present in the neck, chest, thoracic or low back.
- Absence of taut bands
- Presence of at least 11 tender points
A differential diagnosis should be made with another condition such as:
- muscle spasm
- neuropathic or radicular pain
- delayed onset muscle pain
- articular dysfunction
- infectious myositis.
Treatment of myofascial pain syndrome
Treatment for myofascial pain syndrome typically includes medications, trigger point injections, or physiotherapy. Myofascial pain syndrome requires a treatment plan. No conclusive evidence supports using one therapy over another therapy, but exercise is considered an important component of any treatment program. Discuss your options and treatment preferences with the doctor. You will need to try more than one approach to find pain relief or reduction of pain. Many people combine medications with another therapy that relieve pain and muscle stiffness.
Medications
Medications such as non-steroidal anti-inflammatory drugs, acetaminophen, or opioids may be used to treat myofascial pain. Medications for depression, sleep, or muscle spasm are sometimes used, as well. Several medications can be used for the symptoms of myofascial pain syndrome, including:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These drugs are pain relievers. Over-the-counter pain relievers like ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve) may help some people. and your doctor may prescribe stronger pain relievers. Some are available in patches that you simply place on your skin. Over-the-counter drugs like acetaminophen (Tylenol) and ibuprofen (Advil) can relieve pain and swelling. analgesics(Pain-killing medications) are Pain relievers such as lidocaine or diclofenac patch, tramadol, COX-2 inhibitors, and tropisetron (not available in the United States) may be considered.
- muscle relaxants: Benzodiazepines and tizanidine (Zanaflex) can reduction of muscle spasms.
- Sedatives. Clonazepam (Klonopin) helps treat the anxiety and sleep disturbance that sometimes occurs with myofascial pain syndrome. It must be used carefully because it can cause sleepiness and may be habit-forming. Sedatives enhance the quality of your sleep.
- Botox injections: Botulinum A is a potent neurotoxin that avoids and may have pain-relieving effects and muscle contractions.
Physiotherapy treatment of myofascial pain syndrome
Physiotherapy treatments may include:
Physical therapy involving gentle stretching and exercise may be useful for recovering the full range of motion and motor coordination. Once the trigger points are gone, muscle-strengthening exercises can start, supporting the long-term health of the local muscle system.
A physiotherapist can devise a plan to help relieve your pain based on your signs and symptoms. If you have myofascial pain syndrome, treatment is going to be more successful if you see your healthcare provider early after symptoms develop before trigger points are established. In some chronic cases of myofascial pain, combinations of physiotherapy, myofascial release therapy, trigger point injections, or massage are needed.
Many treatments are available and your medical professional will likely use a mixture of the following to manage your pain and restore affected muscles. Physical therapy to relax, stretch and strengthen muscles. Physiotherapy helps to relieve myofascial pain syndrome and may involve:
There are two different approaches to the treatment of myofascial trigger points. There are non-invasive techniques like Therapeutic Ultrasound, Low-level laser therapy, and TENS (Transcutaneous Electrical Nerve Stimulation).
Low-level light therapy / cold laser
- lasers using to stimulate the release of pain-relieving chemicals. low-level light therapy is also known as cold laser, in which the trigger point is exposed to near-infrared light
- Ultrasound therapy uses sound waves to increase blood circulation and warmth, which may promote healing in soft tissues affected by myofascial pain syndrome. These machines transmit sound waves into the soft tissue through a sound-conducting gel applied to the skin. The sound waves can heat up and relax muscles, increasing blood flow, and removing scar tissue. The pain-relieving effects may be minimal. But, this treatment may reduce or diminish stiffness and increase mobility if done before stretching. This therapy uses sound waves to penetrate soft tissues.
- This therapy has been successfully used for pain associated with rheumatoid arthritis, so it may be worth discussing with your doctor.
TENS (Transcutaneous electrical nerve stimulation)
- Transcutaneous electrical nerve stimulation involves sending low-voltage electric signals from a small device to the painful area through electrodes attached to your skin
Electrical stimulation involves placing an electrode across the muscle affected by a trigger point to cause rapid contractions.
Massage therapy:
There are some types of massage treatments that can relax myofascial trigger points. These include:
- passive rhythmic release
- active rhythmic release
- shiatsu (acupressure)
- trigger point pressure release
Massage techniques increase blood flow and warm up muscles. This can help reduce stiffness and relieve pain. your therapist applied pressure on your trigger points, which will aggravate the pain and then release the muscle tension. A physiotherapist may massage your affected muscle to help relieve your pain. A physical therapist may use long hand strokes along your muscle or place pressure on specific areas of your muscle to release tension. Massage therapy using trigger-point release techniques could also be effective in short-term pain relief. massage may improve the condition.
Myofascial release therapy involves gentle fascia manipulation.
- The dry needling technique is one of the fastest ways to inactivate myofascial trigger points. Dry needling, in which the doctor will insert a thin needle directly into and around your trigger point, move it around, and poke it in and out. dry needling technique involves inserting a needle into several places in and around the trigger point. It can be quite painful and helps break up muscle tension, but it’s one of the most effective ways to inactivate a trigger point and reduce the pain. Acupuncture also appears to be helpful for a few people who have this pain syndrome. some therapists use acupuncture needles, which are smaller and less painful than hypodermic needles. There are some key differences between dry needling and acupuncture. pushing thin needles into the trigger point to reduce tightness, increase blood flow and relieve pain. A systematic review concluded that dry needling for the treatment of this pain syndrome in the lower back appeared to be a useful adjunct to standard therapies, but that clear recommendation could not be made because the published studies were small and of low quality.
Wet needling/trigger point injections
- Trigger point injections are such as dry needling. Typically, doctors use a needle to inject saline or a local anaesthetic like lidocaine into the trigger point to relieve pain. The effects are compared to dry needling, but the procedure may cause less discomfort and Trigger point injections with steroids are also an option. Wet needling is also known as trigger point injections, is the same as dry needling except for the doctor simultaneously injecting a numbing agent or steroid.
Stretching techniques (e.g. spray and stretch)
- A physiotherapist may lead you through gentle stretching exercises to help ease the pain in your affected muscle. If you feel trigger point pain when stretching, the physiotherapist may spray a numbing solution on the skin. Stretching helps many people with myofascial pain syndrome. Some physiotherapists apply a cold, numbing spray to the muscle area before leading someone through stretches. There are also some gentle stretches and exercises you can try at home to decrease pain.
- “Stretch and spray” technique: This technique involves spraying the muscle and trigger point with a coolant and then slowly, manually stretching the muscle.
Heat: Applying heat, via a hot pack or a hot shower, can help relieve muscle tension and reduce or decreased pain.
Acupuncture and relaxation therapies, including cognitive behavioural therapy and biofeedback also good for improving sleep and reducing anxiety.
Posture training
Which, Improving your posture can help relieve myofascial pain, particularly in your neck muscle. Exercises that strengthen the muscles surrounding your trigger point will help you prevent overworking of any one muscle.
Many physical and manual therapy techniques such as:
- Post-isometric relaxation
- Active Release Techniques
- Trigger point pressure release
- Muscle energy techniques
Other treatment options include:
- Dietary changes to reduce inflammation and prevent ingredients that seem to trigger pain
- Heat
- Behaviour modification such as exercise, posture, workstation setup, yoga, meditation, sleep habits, etc.
- Physiotherapy, including steps to realign posture, as needed
- Acupuncture
Home advice
Treatments you can do at home include:
- Heat as in a heating pad. Some people benefit from cold/ice packs.
- Exercise. Specifically weight-bearing exercises to help strengthen muscles, stretching exercises to stretch muscles, and aerobic exercises to get more oxygen into the muscles.
- Over-the-counter pain killers such as acetaminophen or NSAIDs like ibuprofen or naproxen. Don’t take these drugs if you are taking analgesics or NSAIDs prescribed by your doctor.
- Relaxation techniques include yoga to stretch, decrease stress, and relax the muscle, breathing exercises, and meditation.
- changes in your diet avoid foods known to cause inflammation.
- Soaking in warm water.
- Massages.
- The duration of this pain syndrome varies from person to person. With treatment, it may go away after a day or some weeks, but it can take longer for some.
How fast this pain syndrome resolves depends on some factors, including:
- Your general health.
- Diet.
- Amount and quality of sleep.
- Take care of yourself if you have this pain syndrome. Self-care measures to maintain your body healthily may make it easier for you to concentrate on coping with your pain. Try to:
- Exercise: Gentle exercise can help you cope and improve with pain. When your pain allows, get moving. Ask your doctor or physiotherapist about proper exercises.
- Relax: If you’re stressed and tense, you may experience increased pain. Find ways to relax. Meditating, talking with friends, or writing in a journal can all be helpful.
- Take care of your body: Eat a healthy diet of vegetables and fruits. Get enough sleep so that your wake rests. Take care of the body so that you can put your energy toward coping with your pain.
Prevention of myofascial pain syndrome
Certain factors can put you more at risk for developing myofascial pain syndrome and Managing these risk factors may not prevent you from developing the syndrome but could help reduce or diminish the severity of this condition.
Many of the preventable suggestions to follow are also pain management strategies:
- Maintain proper sleep hygiene.
- Reduce your stress.
- Get exercise.
- Prevent muscle injury. (this is an example of preventing muscle injury, is the shoulder bag or purse you carry too heavy).
- Practice relaxation methods.
- Eat a diet healthy, like the Mediterranean diet.
Some foods lead to inflammation and inflammation increases myofascial pain. Some foods to avoid include:
- Fried foods (French fries, for example).
- Dairy (milk, cheese, yogurt).
- Refined carbohydrates and foods with refined flour such as pizza, pasta, pastries, white bread, and breakfast cereals.
- Margarine (butter), vegetable oil.
- Sugary foods and beverages like soft drinks.
- Red meat (burgers, steaks).
- Artificial sweeteners and general additives (“no sugar added” products, zero-calorie “diet” soft drinks, and processed foods that include candy, ice cream, and fruit).
- Processed meat like hot dogs, and sausage.
DISCLAIMER:
This article is intended or purposeful for your general informational purposes only and does not address particular circumstances. it is not a substitute for professional advice(or guidance) or help( or assistance) and should not be relied on to make decisions of any kind. A few or any actions you take upon the information presented in this article are strictly at your own risk and responsibility.





Myofascial pain syndrome gradually become common in people due to continuous stress and workload, Physiotherapy treatment offers permanent solution and natural way to recover, i personally recommend everyone go for Physical therapy!