Achilles Tendon Tear
Introduction
An Achilles tendon tear usually occurs when there is a complete gap between the upper and lower portions of this tendon. The tear takes place 2-3 inches above the heel bone but it can also be higher in the leg or directly at the attachment.
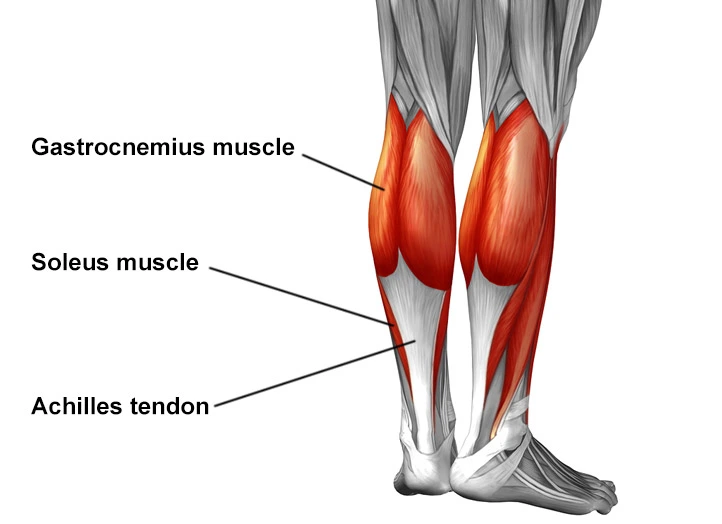
The connection between the heel and calf muscles is made through the Achilles tendon which is the largest tendon in the body. It provides the strength to push off with forces up to 10 times our body weight.
Your body’s biggest tendon is the Achilles tendon which runs from the bones of your heel to your calf muscles. It is a springy band of tissue located at the back of your ankle and above your heel. It enables you to point your toes downward and raise your tiptoes. The dense fibers of the Achilles tendon make it extremely strong and it can withstand forces up to 1,100 pounds.
However, due to the poor blood flow in this area of the leg, the Achilles tendon can be easily injured. When the lower part of your leg feels stiff or burns, your doctor may refer to it as tendinitis or tendonitis.
If the pain is severe, it could indicate that your Achilles tendon is partially or completely torn.
Which symptoms point to a torn Achilles tendon?
Presumably due to the causes primarily related to sports, there is a noteworthy over-representation of males.
Individuals who fall within the age group of 30-50 years and have no prior history of calf or heel pain are usually the ones who seek medical attention for this condition. However, there exist several acknowledged factors that can contribute to the development of this condition.
- intra-tendinous steroid injection
- diabetes mellitus
- systemic inflammatory illnesses
- rheumatoid arthritis
- systemic lupus erythematosus
- repeated microtrauma
- gout
- fluoroquinolone antibiotics
- ochronosis 4
- hyperparathyroidism
During physical activities such as running and jumping, or in the event of a slip or fall, a tear can occur. Patients often describe their initial sensation as a “pop” or feeling as though they’ve been struck at the back of the ankle, which is followed by some pain. Typically, there is no pain in this area before the tear. After the tear, patients may experience weakness when attempting to push off their feet while walking or standing on their tiptoes. In the first few days, there may be a small bruise on the inside of the heel.
The main indications are sudden pain and swelling at the back of the ankle. At the time of injury, most individuals will hear a distinctive popping sound or feel like they were struck in the back of the leg with a hard object. It may be challenging or impossible to bend the forefoot downward or effectively push off from the foot with the injury.
What causes an Achilles tendon tear?
Achilles tendon ruptures are typically the result of sudden and intense athletic activity that was not preceded by adequate stretching. These ruptures tend to happen during high-stress activities such as running, jumping, or cutting, but in some cases, the tendon may become weakened over time and rupture during less intense activities like walking. Approximately 10% of Achilles tendon ruptures occur in individuals who have pre-existing Achilles tendinopathy.
The ability to point your foot downward, rise on your toes, and push off your foot when walking heavily relies on your Achilles tendon. It is used almost every time you move your foot.
If ruptured, the Achilles tendon is usually damaged in the section situated within 2 1/2 inches (about 6 centimeters) from the point where it connects to the heel bone. This part may be more prone to ruptures due to the poor blood flow, which also makes it harder to heal.
The sudden increase in stress on your Achilles tendon is often the cause of ruptures. Some common examples include:
- increasing the intensity of sports activities
- particularly those involving jumping
- falling from a height
- stepping into a hole.
- Certain medications and medical conditions are known to increase the risk of Achilles tendon rupture.
If an individual experiences a ruptured Achilles tendon, they may feel a sudden, sharp pain in the back of their ankle or calf, which can then turn into a dull ache. They may also feel a popping or snapping sensation, notice swelling between their heel and calf, or have difficulty walking or rising on their toes.
It is vital to seek prompt medical attention when experiencing these symptoms to prevent further damage. In the meantime, the patient should follow the RICE method, which involves resting the injured foot and ankle, applying a bag of ice covered with a thin towel to reduce swelling and pain, and wrapping the foot and ankle in an elastic bandage to prevent further swelling, and elevating the leg to reduce swelling. The leg should be even with or slightly above heart level.
Diagnosis
Patients typically experience sudden pain and swelling in the Achilles region, often accompanied by an audible snap while forcefully dorsiflexing the foot. For instance, a ‘weekend warrior’ playing squash is a classic example.
If the injury is complete, minimal plantar flexion against resistance will be possible, and a defect may be felt. Obtaining a diagnosis can be aided by a clinical examination.
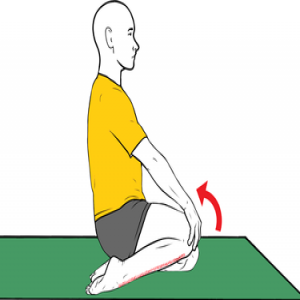
The calf-squeeze (Thompson) test can be used to examine the integrity of the Achilles tendon by squeezing the calf. The test is positive when the foot does not move or shows minimal plantarflexion. It has a sensitivity of 96%, specificity of 93%, positive likelihood ratio of 13.71, and negative likelihood ratio of 0.04. (Note: This information is based on one study).
Diagnosis of an Achilles tendon rupture is typically based on the symptoms reported by the person and their medical history. The sensation is often described as being similar to getting kicked or shot behind the ankle. During a physical examination, a gap above the heel may be noticeable, unless there is swelling present. One common physical test that a healthcare provider may perform is the Simmonds test, also known as the Thompson test. This test involves having the person lie face down on an exam table with their feet hanging off the edge.
If the test is positive, squeezing the calf muscles of the affected leg will not result in any movement (passive plantarflexion) of the foot. Conversely, if the test is negative, the person’s unaffected Achilles tendon will allow the foot to flex down when the calf muscle is squeezed. The injury will typically make walking difficult, as the person will be unable to step off the ground with the affected leg. Standing on the toes of that leg will also be impossible, and pointing the foot downward (plantarflexion) will be difficult. Swelling around the ankle is a common symptom, and pain can be severe.
Although diagnostic tests like an ultrasound scan are sometimes necessary to confirm the diagnosis, an Achilles tendon tear can often be diagnosed by history and physical exam alone. Ultrasound imaging is an effective method of monitoring the healing progress of the tendon over time and is recommended over MRI, which is generally not needed. Both MRIs and ultrasounds are useful diagnostic techniques, each with advantages and disadvantages. However, when it comes to an Achilles tendon tear, ultrasound is usually recommended first due to its convenience, quick availability, and lower cost.
Ultrasonography is a technique used to determine the thickness, character, and presence of a tear in the tendon. This method involves sending harmless high frequencies of sound waves through the body, which reflect off the spaces between fluid and soft tissue or bone. These reflected images are analyzed and turned into images. These images capture the movement of the tendon in real time and help visualize injuries or tears. Ultrasound imaging is inexpensive and involves no harmful radiation, but is operator-dependent and requires a level of skill and practice to be used effectively.
MRI can be used to distinguish incomplete ruptures from degeneration of the Achilles tendon, as well as identify para-tenonitis, tendinosis, and bursitis. This technique involves using a strong uniform magnetic field to align millions of protons running through the body, which are then bombarded with radio waves that knock some of them out of alignment.
When these protons return, they emit their unique radio waves that are analyzed by a computer in 3D to create a sharp cross-sectional image of the area. Excellent soft tissue imaging from an MRI makes it simpler for technicians to identify tears or other damage.
Radiography can also be used to identify Achilles tendon tears, albeit indirectly. X-rays are used in radiography to analyze the site of damage. However, this method is not particularly effective at identifying soft tissue injuries. X-rays are created when high-energy electrons hit a metal source, and the images are acquired by utilizing the different densities of the bone or tissue.
Soft tissue shows poorly on X-rays, while dense structures like bone are typically best seen. Radiography is not the best method for assessing an Achilles tendon injury, but it is useful for ruling out other injuries such as heel bone fractures.
Differential diagnosis
When diagnosing an Achilles tendon tear, it is important to consider certain conditions such as Achilles tendinitis, ankle sprain, and avulsion fracture of the calcaneus.
Treatment of Achilles Tendon Tear
For Immediate Symptom Relief
To relieve swelling
In case of an injury, it is recommended to apply an ice pack directly on the affected area as soon as possible. This is going to help in pain relief and edema reduction. Additionally, when sleeping, it is advisable to elevate your leg using pillows so that it is above your heart level. This promotes blood circulation and reduces inflammation in the affected area.
When sitting, it is important to keep your foot raised and supported with a cushion or stool for optimal healing. While walking, you can use a boot or crutches to keep the weight off your ankle and reduce pressure on the injured area.
To alleviate pain
To alleviate pain: over-the-counter medications such as ibuprofen (such as Advil or Motrin), naproxen (such as Aleve or Naprosyn), or acetaminophen (such as Tylenol) are recommended. However, it is important to consult your healthcare provider if you have a history of heart disease, liver disease, high blood pressure, kidney disease, or stomach ulcers or bleeding before taking these medications.
In addition, quitting smoking is recommended as it may affect the healing process after surgery. Children under the age of 19 shouldn’t be administered aspirin. Lastly, it is crucial not to exceed the recommended dosage of painkillers on the bottle or as directed by your healthcare provider to avoid any adverse effects.
- There are both surgical and nonsurgical options available for treating an Achilles tendon rupture. The decision of which method to use is based on factors such as the extent of the rupture and the patient’s overall health and activity level.
- Patients with minor ruptures or less active lifestyles, as well as those with medical conditions that make surgery impossible, may opt for nonsurgical treatment. This approach carries a higher risk of re-rupture and involves the use of a cast, walking boot, or brace to restrict movement and promote healing of the torn tendon.
Surgery
Surgery can offer significant benefits, including reduced risk of re-rupture, increased push-off strength, and improved muscle function and ankle movement. The approach utilized during surgery will be tailored to meet the specific requirements of the patient.
Following surgery, the foot and ankle will be immobilized in a cast or walking boot. The surgeon will determine when weight-bearing can begin. Possible complications of surgery include incision-healing issues, re-rupture, or nerve pain.
Physical therapy
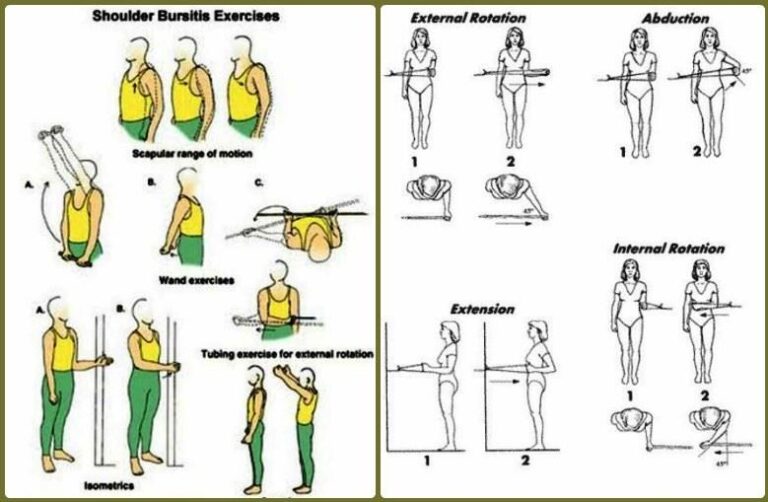
Physical therapy is a key part of the healing process, regardless of whether the rupture was treated surgically or nonsurgically. This involves exercises that strengthen muscles and improve the range of motion in the foot and ankle.
Rehabilitation and activity
Rehabilitation and activity are important aspects of the recovery process. Patients will be asked to begin moving the heel at some point, usually within 2 to 6 weeks after the injury, and physical therapy will help them return to normal activity within 4 to 6 months.
Stretching exercises should be done slowly and without bouncing or using too much force. After healing, patients should take steps to minimize the risk of re-injury, such as staying in good shape, avoiding high-heeled shoes, and properly warming up and stretching before playing sports like tennis, racquetball, or basketball.
How long does it take for recovery to occur after Achilles tendon surgery?
The recovery process for Achilles tendon repair surgery is lengthy and necessitates consistent rehabilitation to restore foot and ankle movement and tendon strength. Generally, patients can expect to be immobilized and non-weight-bearing (using crutches) for three to four weeks after an Achilles tendon repair. It typically takes around six to nine months to return to all activities, such as running or jumping.
Is physical therapy required following Achilles tendon surgery?
Yes, physical therapy is necessary to decrease scarring and swelling and to encourage the strengthening of the Achilles and other soft tissues in the ankle. Your physical therapist will usually employ blood flow restriction techniques during rehabilitation to enhance your strength without overloading the newly repaired tendon.
Ideally, you will commence a PT routine almost immediately after surgery and continue it until you have achieved your desired activity level. Physical therapy usually lasts for six months after surgery.
Who may sustain damage to their Achilles tendon?
- Achilles tendon injuries are more common in healthy, active men aged between 20 and 39.
- Nowadays, more older people are being treated for Achilles tears as people tend to stay healthy and active for longer.
- The incidence rate of Achilles tendon ruptures in the general public is 1.8 per 100,000 annually, but in athletic populations, it’s between 6,000 and 18,000.
- The sports most commonly associated with Achilles tendon rupture are basketball, soccer, football, tennis, and running.
- If you feel pain in your Achilles tendon, it is advisable to stop the activity and rest. Minor injuries may not need medical treatment. However, if the pain persists, it is best to see a doctor. If you hear a popping or snapping sound at the time of the injury, see your doctor right away, as it indicates a complete tear of the tendon.
How do you prevent an Achilles tendon rupture?
- It is not well known how to prevent Achilles tendon ruptures as they occur so rarely. However, a stretching program for the Achilles tendon is a good idea, although the benefit has not been proven. Stretching should be part of every athlete’s warm-up routine, and smoking should be avoided as it negatively affects tendon health.
- It is advisable to engage in stretching and warming up activities before any physical activity to prevent an Achilles rupture. Similarly, cooling down after exercise can also aid in preventing such an injury. Cross-training and varying your workout may help avoid overuse syndromes that can lead to tendon problems.
- Maintaining a healthy body weight can reduce the load on the tendons and muscles. Wearing appropriate footwear for the sport or exercise being undertaken, exercising within fitness limits, and following a sensible exercise program are also recommended.
- Gradually increasing exercise intensity and avoiding unfamiliar strenuous exercise can also help prevent Achilles tendon injuries. Additionally, a gradual “warm down” after exercising and calf muscle stretching and strengthening exercises can allow the Achilles tendon to absorb greater forces and prevent injury.
Overview
Injury to the Achilles tendon can cause the fibers to tear, resulting in loss of function and pain. A rupture can be either complete or partial and may require surgery for treatment. Well-trained professional athletes are less likely to experience an Achilles tendon rupture, which is more common in men than women. Additionally, the frequency of this injury increases as individuals age beyond 30 years.
FAQs
Can you still walk on a torn Achilles?
Patients who have experienced a rupture of the Achilles tendon can still walk, as well as actively move their ankle up and down. Patients with an Achilles tendon rupture may even be able to stand on tiptoes, but only on both feet together and not on the injured limb alone.
Can Achilles tear heal on its own?
Consulting with a physician is recommended for a proper diagnosis and guidance through rehabilitation in the case of an Achilles tendon tear. Although partial tears can heal without medical intervention, the term “heal on its own” can be problematic.
How long does a torn Achilles tend to heal?
It is important to note that the process of rehabilitating Achilles rupture can be lengthy, taking up to six months to return to lower-impact activities such as walking and hiking. Engaging in higher-impact activities like soccer and football may not be possible until after nine months of rehabilitation.
How serious is an Achilles tear?
If you experience a tear or rupture, probably, you won’t be able to participate in your preferred sport for at least one season. During the initial recovery period, even walking can be challenging, or it may not be possible at all for a few weeks. Several factors, including the extent of the injury, will determine your treatment plan.
Is Achilles tear worse than ACL?
Injuries to the ACL are certainly difficult to deal with, but injuries to the Achilles tendon are often considered the most severe. It can take up to a year to fully recover from a rupture of the Achilles tendon, and for professional athletes, such an injury could potentially end a promising career.
References
- Achilles tendon rupture (tear) – symptoms, causes, and treatment. https://www.southerncross.co.nz/medical-library/muscle-joint-and-bone-conditions/achilles-tendon-rupture-tear-symptoms-causes-and-treatment
- Achilles tendon tear. Radiopaedia.org. https://doi.org/10.53347/rid-836
- Achilles Tendon Tear | FootCareMD. https://www.footcaremd.org/conditions-treatments/ankle/achilles-tendon-tear
- Achilles Tendon Rupture: Symptoms, Treatment, Recovery | Hospital for Special Surgery.https://www.hss.edu/conditions_achilles-tendon-rupture-injuries
- Why does the healing process of Achilles tendon injuries take a long time?|Medical Center. (n.d.). https://utswmed.org/medblog/achilles-tendon-injuries-rehab/
- Achilles tendon rupture – aftercare: MedlinePlus Medical Encyclopedia.https://medlineplus.gov/ency/patientinstructions/
- Achilles Tendon Rupture – Foot Health Facts. https://www.foothealthfacts.org/conditions/achilles-tendon-rupture
- What Is an Achilles Tendon Injury? WebMD. https://www.webmd.com/fitness-exercise/achilles-tendon-injury
- Achilles Tendon Tear – Symptoms and Treatment – OrthoInfohttps://orthoinfo.aaos.org/en/diseases-conditions/achilles-tendon-rupture-tear-video/
- Achilles tendon rupture. Wikipedia. https://en.wikipedia.org/wiki/Achilles_tendon_rupture





One Comment