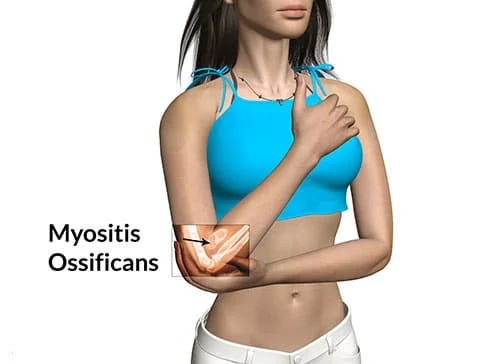
Myositis Ossificans (MO): Physiotherapy Treatment
What is Myositis Ossificans?
- Myositis ossificans results from a complication of a contusion injury and occurs when part of the hematoma is replaced with bone. This condition can occur anywhere in the body but more commonly occurs in the quadriceps.
- The bone deposits may occur as separate pieces or pieces of bone lying entirely within the muscle or attached to the bone (exostosis).
- These calcium deposits are thought to be caused by periosteal cells that invade the hematoma following the injury.
- This causes a partial avulsion of muscle fibers from the periosteum.
Mechanism of Injury
- Usually caused by injuries that result in severe contusion or chronic contusion injuries.
A patient will first present with severe pain at first usually with a contusion and a palpable mass within the muscle.
Pathogenesis:
- Muscle is commonly but not invariably involved, and fascia, tendon, and periosteum can also be the site.
- The process is a peculiar alteration within the ground substance of connective tissue, associated with the striking proliferation of undifferentiated mesenchymal cells.
- Initially there is degeneration and necrosis, in case of muscle, disrupted muscle fibers retract. In 3 to 4 days, fibroblasts from endomysium invade damaged area and rapidly form broad sheets of immature fibroblasts.
- At the same time, primitive mesenchymal cells proliferate within injured connective tissue. Intense cellular proliferation of fibroblasts and mesenchymal cells produces a histological picture that may be erroneously diagnosed as fibrosarcoma or myosarcoma.
- Ground substance becomes homogeneous or glassy or waxy, suggesting some type of edema. It increases in amount and encloses some mesenchymal cells, which then assume the morphological characteristic of osteoblasts. Mineralization follows and bone is formed. This event typically takes place first within the least damaged part i.e. periphery.
- As the process of osteoid formation and mineralization changing in mature bone evolves, it progressively extends towards the central, severely damaged area. When myositis is not removed and is allowed to mature, it becomes oriented and covered by a cartilaginous cap, because of muscle action over the lesion. This is called post-traumatic osteochondroma and is common in the region of the knee joint.
Classification of Myositis Ossificans
Physicians divide myositis ossificans into two categories:
Nonhereditary myositis ossificans:
The most prevalent kind of myositis ossificans is nonhereditary. It is the term that most people use to describe myositis ossificans. It happens following an injury, usually to the arms or thighs. The terminology myositis ossificans traumatica and circumscripta are commonly used.
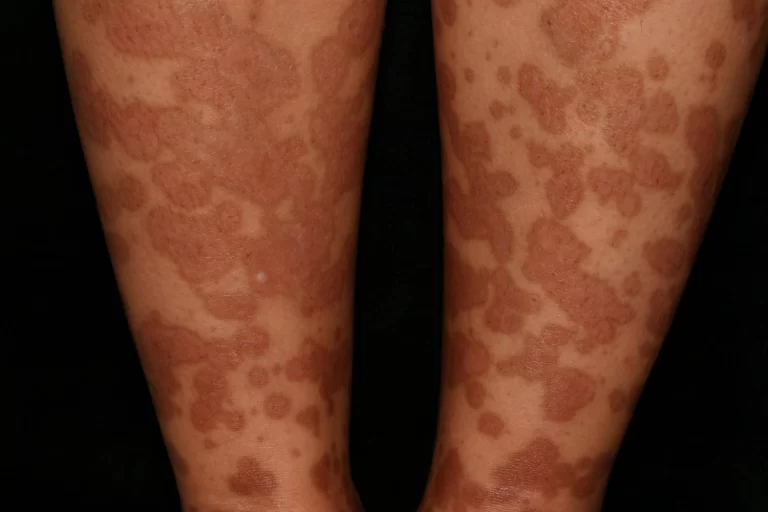
Myositis ossificans progressiva:
When referring to fibrodysplasia ossificans progressiva (FOP), some may still use the outdated name myositis ossificans progressiva. This condition mostly occurs due to a mutation in a gene.
Causes of Myositis Ossificans
- Contusions that are severe.
- Contusions result in a large loss of movement.
- Contusions that are inappropriately managed.
- Re-injury to the contusion (e.g. an additional impact).
- Patients who do not rest sufficiently following a contusion.
- Patients who do not use ice following a contusion.
- Patients who receive massage too soon or too vigorously following injury.
- Patients who exercise (e.g. stretch) or perform activities in pain.
- Patients who continue to play through injury.
- Patients who recommence sport too early following injury.
Signs and Symptoms
- Restricted range of movement.
- Bruising.
- Pain.
- Palpable mass in muscle.
- An X-ray can show bone growth.
Examination and Evaluation
- Observation.
- Look at how the athlete moves.
- Look for swelling, contusion, and ecchymosis.
- Check for a palpable mass within the muscle. Mass usually shows up within 2-3 weeks.
- Palpation.
- Palpate along the muscle and around the contused area to feel for a calcium deposit.
- Special Test.
- Manual Muscle Testing– assess the strength of the athlete you are testing.
- Check Range of Motion-check the athlete’s range of motion to see if calcium deposit is decreasing ROM.
Types of Myositis Ossificans
There are three types of myositis ossificans:
- Type 1: There is a thin stalk of bone formed between the ossified muscle and bone.
- Type 2: A broad area of ossified muscle located between muscle and bone.
- Type 3: The ossified muscle is not connected to the bone, and even appears to derive completely from muscle.
Diagnosis:

- Plain film radiographs.
- MRI.
- CT scan.
- Bone scan.
Treatment of Myositis Ossificans
- Rest.
- Immobilization.
- Anti-inflammatory drugs.
- Physiotherapy management.
- Surgical debridement.
Physiotherapy Treatment
- Rest.
- Immobilization.
- TENS.
- Pulsed Ultrasound and phonophoresis.
- Maintain available range of motion but avoid stretching and massage, until maturation.
- Iontophoresis with 2 % acetic acid solution.
- Extra-corporeal shock wave therapy.
- Pain-free gentle ROM exercises.
- Cold therapy application- Elevation.
- Compression.
Surgical Treatment
- Growth should not be removed in the premature stage as it will likely reoccur.
- The ossification becomes exuberant, infiltrates beyond the original site, and compresses the soft tissues around beyond hope of repair.
- When after serial x-rays the mass is dense, well delineated, and at a standstill, it may be safely removed. It may be possible to prevent myositis by aspirating the original haematoma.
How to Prevent Myositis Ossificans(MO)?
Myositis ossificans cannot be prevented with certainty. However, by appropriately managing injuries, particularly if you have significant bruising or swelling, you can lower your chance of developing nonhereditary myositis ossificans. Apply the RICE technique as soon as possible following an accident. RICE is an acronym for:
- Rest.
- Ice.
- Compression.
- Elevation.
Lowering your risk of injury can also help your chance of myositis ossificans. Injury prevention requires appropriate rest, stretching, and conditioning.
Return to Activity/Play
Without the bone growth reaching its full resolution, a full return to play is possible. Athletes’ comfort and functionality serve as the main guiding factors for their return to play. An athlete must have a complete range of motion and strength in the injured muscle before they may resume. They have to be capable of doing all the duties associated with their profession and sport. Sufficient protection of the area is necessary to prevent additional stress.
Epidemiology
Since trauma is the primary cause of myositis ossificans instances, young adults are the main population affected. Paraplegics are another population that is particularly vulnerable to myositis ossificans, typically in the absence of any signs of trauma.
Prognosis
Myositis ossificans typically resolves on its own without surgery if it arises following an accident. For several months following therapy, you can experience persistent stiffness or restricted range of motion.
Myositis ossificans progressiva is incurable. This serious illness shortens your life expectancy and produces symptoms that worsen with time.
Conclusion
When bone grows where it shouldn’t, usually in your muscles or other soft tissues, you get myositis ossificans. Myositis ossificans typically appears following a traumatic injury. More severe symptoms are caused by less common genetic variants of myositis ossificans. For these kinds of myositis ossificans, there is no specific treatment. Physicians usually use nonsurgical techniques to treat myositis ossificans traumatica. This kind of myositis ossificans typically heals up in a few weeks or months.
FAQs
What is the main cause of myositis ossificans?
Following a break in the bone or stress to the muscle, myositis ossificans (MO) develops. In between the damaged muscle fibers, new bone cells grow. Most frequently, this occurs near the thigh or elbow.
What is the most common muscle site for myositis ossificans?
Myositis ossificans most commonly develops in large muscles, particularly those around the:
Thighs: The quadriceps muscle on the front of the thigh is the most frequent site of myositis ossificans.
Upper arms: The brachialis muscle in the upper arm is another common location.
Buttocks: The gluteal muscles can also be affected.
How to fix myositis ossificans?
Treatment is conservative at first since calcifications can be reabsorbed by the body and, with appropriate management, some patients can recover completely even with calcifications. Conservative treatment consists of immobilizing the injured muscle or, less frequently, resting from activities that put a load on the muscles.
What is the difference between myositis ossificans and heterotopic ossificans?
Myositis ossificans is a particular kind of HO that develops in inflammatory muscle, while HO itself is the production of mature lamellar bone in nonosseous tissue.
What is the drug of choice for myositis ossificans?
Most of the time, myositis ossificans goes away on its own. Using an ibuprofen or naproxen pain medication can help ease pain. Resting the region is one of the other things one can perform at home.
Is myositis ossificans a tumor?
Myositis ossificans (MO) is a heterotopic bone formation that is non-neoplastic, self-limiting, and usually affects the major muscles in the extremities. While it is unusual in infants or elderly individuals, it can happen to anyone at any age.
Can you massage myositis ossificans?
You should never attempt to “stretch out” an injury if you have myositis ossificans or fear you may have it. Excessive stretching can worsen the injury, increase pain, promote bone growth, and slow down the healing process. For the same reason, deep massage over the injury should be avoided.
How is myositis ossificans treated in physiotherapy?
To relieve your pain, your physical therapist may use techniques like ultrasound, transcutaneous electrical nerve stimulation, interferential current, cold, heat, or other techniques. In order to relieve pain and promote tissue and limb mobility, they could also apply a light massage to the affected muscle.




5 Comments