Olecranon Fracture
Introduction
An elbow break in the bony tip is called an olecranon fracture. One of the three bones that join to form the elbow joint is the ulna, which includes this pointy section of bone.
An olecranon fracture is a fracture that occurs in the ulna or the “pointy bone” of your elbow that protrudes when you bend your arm. Commonly occurring in isolation with no other injuries, this kind of fracture can also be a component of a more complicated elbow injury.
Fractures of the olecranon are not uncommon. They can be a component of a more complicated elbow injury, even though they typically happen on their own without any other injuries.
A direct blow (such as a fall on the elbow or a direct impact from an object) or an indirect blow can result in an olecranon fracture. Landing on an outstretched arm is largely more important than the latter.
They manifest in young patients after high-energy injuries or, more frequently, in elderly patients after low-energy indirect injuries, with a bimodal age distribution.
The olecranon is exposed to little protection from muscles or other soft tissues because it is situated just beneath the skin of the elbow. If you take a direct hit to the elbow or trip over the elbow tip, it may break easily. Elbow motion may be extremely painful or impossible if you have a fracture.
A small crack or multiple broken pieces can occur in an olecranon fracture. The fractured bone fragments may align perfectly or they may be displaced, or out of alignment.

Sometimes a bone breaks so that pieces of the bone protrude through the skin, or a wound goes all the way down to the bone. This is known as an open fracture. Open fractures are especially dangerous because there is a higher risk of infection in both the bone and the wound after the skin is broken. Treatment must begin right away to stop infection.
These fractures are thought to be among the most straightforward articular lesions, and they can be easily treated surgically and physiotherapeutically. The majority of these fractures occur intra-articularly, and hematomas and joint effusions are frequently present. Avulsion fractures are classified as extra-articular fractures and are most frequently observed in the elderly.
Relevant Anatomy
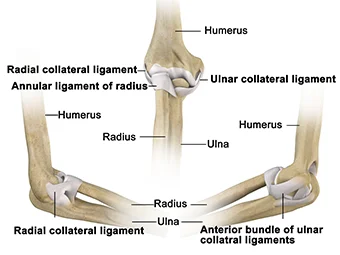
Three bones make up the elbow joint:
- The upper arm bone, or humerus
- The radius, or thumb-side forearm bone
- The pinky side of the forearm bone, or ulna
Like a hinge, the elbow joint can bend and straighten. Additionally, it is crucial for forearm rotation, or the capacity to turn your palm up (for example, when accepting change from a cashier) or down (for example, when typing or playing the piano).
The following joints comprise the elbow joint:
- The ulna-humeral joint
Function: Elbow flexion/extension; stability - The radio-humeral joint
Function: pronation/supination of the forearm; lateral stability - Proximal radio-ulnar joint
Function: Pronation and supination of the forearm
Olecranon Function:
- Consequently, the triceps insertion point plays an important role in the elbow’s extensor mechanism.
- Major elbow joint articulation
Parts of all three bones make up the elbow:
- The lower end of the humerus is called the distal humerus. It is the spool near which the forearm extends and straightens and forms the upper portion of the elbow.
- The knobby end of the radius wherever it joins the elbow is called the radial head. When you bend your arm, it slides up and down the anterior portion of the distal humerus, and when you rotate your wrist up or down, it circles the ulna.
- The portion of the ulna that covers the lower end of the humerus to provide a hinge for elbow movement is called the olecranon. Because there is very little tissue covering the bony point of the olecranon, it is easily felt beneath the skin.
The osseous structure of the elbow, along with muscles, tendons, and ligaments, hold it together. Three major nerves cross over the elbow joint.
Pathophysiology
In general, olecranon fractures affect the elbow’s articular surface. About 20% of cases result in posttraumatic arthritis, and this outcome is linked to persistent mal-reduction of the articular surface greater than 2 mm. By unintentionally narrowing the greater sigmoid notch, mal-reduction of fractures resulting in substantial comminution can additionally predispose the patient to arthritis.
The radial nerve innervates the triceps muscle, which inserts onto the olecranon and merges with the periosteum. Active elbow extension is lost when the extensor mechanism is disrupted by a displaced fracture. The primary deforming force, which pulls the separated fragment superiorly, comes from the triceps pull. Increased displacement indicates that the fibrous sheath covering the olecranon has torn.
By preventing the anterior translation of the ulna concerning the distal humerus, the olecranon stabilizes the elbow joint. Olecranon fractures may be related to radial head fractures, coronoid process fractures, and ligamentous injury (the medial, as well as lateral collateral ligaments, support valgus and varus stress, respectively). Restoring elbow stability after unstable injuries necessitates olecranon reduction and stable fixation.
The ulnar nerve is located on the medial aspect, running alongside the ulnar artery before crossing anteriorly and passing behind the medial collateral ligament. When working in this area, it’s important to be aware of these structures.
Epidemiology
Roughly 10% of fractures in the upper extremities are olecranon fractures. Twelve cases out of 10,000 occur. Men are more likely than females to suffer an injury at a younger age, with a mean age of occurrence of 57. Synchronous elbow injuries, most commonly to the radial head and coronoid, are often linked to these injuries. One-fourth of injuries involve open fractures.
Mechanism Of Injury
Direct:
- Fall onto your forearm: When the elbow is overextended with the hand extended, the olecranon is driven into the distal humerus.
- Articular surface penetration wounds, such as panga wounds
Indirect: By contracting the triceps
- The distal triceps expansion is torn and the olecranon is avulsed during triceps contraction.
- Sportsmen who exert a lot of isometric arm power, such as gymnasts and wrestlers, run the risk of injury
Clinical Features
After a fall from a standing height, people 50 years of age or older typically sustain olecranon fractures. Injuries linked to a higher energy trauma mechanism are more common in younger people. A direct hit to the elbow at a 90-degree angle of flexion or forced elbow hyperextension can result in olecranon fractures.
A triceps tendon’s eccentric contraction can also result in avulsion injuries. These are usually more common in patients with osteoporosis and have an oblique or transverse fracture line.
Olecranon fractures can occur as a result of direct force and elbow injuries. Olecranon fractures frequently result from the following:
- Falling entirely onto the elbow
- Fall onto an extended arm that is securely locked at the elbow to prevent falls
- A direct blow to the elbow during a collision with a hard object, like a baseball bat or a piece of machinery
Those who suffer from an olecranon fracture are typically 57 years old. An olecranon fracture is more common in men and occurs at a younger age.
Symptoms of Olecranon Fracture
The most common way that olecranon fractures manifest is with a history of elbow pain, swelling, and limited movement after falling on an outstretched hand.
Upon examination, the posterior aspect of the elbow usually feels tender to the touch, and there may even be a palpable defect. When the triceps mechanism is interfered with, it is frequently impossible to extend the elbow against gravity. Make sure to assess the affected limb’s neurovascular condition.
A fall on an extended hand can also cause radial head fractures, wrist ligament and bone injuries, and other injuries. Thus, it’s important to check the wrist and shoulder joints as well.
The soft tissue connections that remain intact allow for the preservation of extension, despite the pain, in little displaced olecranon fractures.
Signs and symptoms
An olecranon fracture can impair elbow mobility and typically causes abrupt, excruciating pain. Additional indications of a fracture could be:
- Swelling around the elbow’s back or tip.
- Bruises near the elbow joints. This bruise can occasionally move down the forearm and toward the wrist or up the arm and toward the shoulder.
- Tenderness.
- One or more fingers feeling numb.
- Soreness when rotating the forearm or moving the elbow.
- A sensation of instability in the joint, as though your elbow might break free.
Classification
Elbow stability, comminution, and olecranon displacement are the three main factors used in the Mayo classification system for olecranon fractures. Fractures come in three varieties, each with two subtypes.
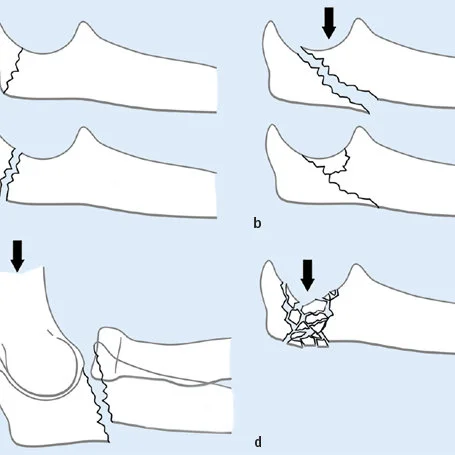
Type I: Fractures that are not comminuted or only slightly comminuted
Type II: A fracture that is displaced but leaves the ulnar collateral ligaments intact
Relocated versus non-relocated
steady-state fracture
Type III: A break that disrupts the humerus and forearm
Relocated versus non-relocated
unstable due to the medial collateral ligament’s disruption
Diagnosis
Physical Examination
After a fall, patients usually complain of elbow pain and swelling. There might be a noticeable deformity and palpable gap at the elbow if the fracture is displaced. The incapacity of extending the elbow against gravity is a characteristic of an olecranon fracture. The examiner has to make sure the patient isn’t imitating active elbow extension with gravity. Usually, to accomplish this, the patient is asked to straighten their elbow from this position after abducting their shoulder to 90 degrees and supporting their upper arm.
It is crucial to look for any related harm or lacerations that could point to an open fracture on the entire affected extremity. Radiographs may be used to assess for associated injuries of the radial head, proximal radioulnar joint (Monteggia fracture), or coronoid process.
The elbow and the surrounding joints should be palpated by the examiner. The affected extremity should undergo a thorough neurovascular examination of the upper extremities. Because of its superficial location on the medial aspect of the elbow, the ulnar nerve is most vulnerable.
Because the olecranon fracture can be distracting, the practitioner should be careful not to overlook injuries that result from high-energy mechanisms and which the patient may not notice. It is advisable to check all four extremities for crepitus, deformity, or pain with range of motion, and to ask the patient about any additional sources of pain.
The physician will ask you about your signs and symptoms and inquire about your general condition and past medical conditions. After that, they will assess your elbow to ascertain the severity of the damage. In the examination, your physician will:
- Examine your skin for bruises, blisters, edema, and cuts. Bone pieces may fracture through the skin in severe fractures, raising the possibility of infection.
- Feel (palpate) the entire area surrounding your elbow to see if there are any other tender spots. This can be a sign of additional fractures or traumas, like an elbow dislocation.
- To make sure there is adequate circulation to your hand and fingers, check your pulse at the wrist.
- Verify your wrist and finger movements, as well as your ability to feel objects with your fingers.
- Physicians may check your elbow, shoulder, upper arm, forearm, wrist, and hand to make sure you don’t have any additional injuries, even if your pain is limited to that area.
Investigation
It is recommended that all admitted patients undergo routine blood tests, such as clotting screens and group and save.
For the majority of fractures, anteroposterior (AP) and lateral elbow radiographs are adequate for the initial evaluation to identify the fracture pattern. If radial head and capitellum fractures are suspected, a specialized radio-capitellar view may also be carried out. Images need to be analyzed for humeroulnar congruity, radial head fracture as well as dislocation and associated coronoid.
Plain anteroposterior and lateral radiographs of the affected joint, as well as possibly the joints above and below, should be used for initial imaging.
When the triceps are pulled, olecranon fractures can usually be seen on a lateral projection and have some displacement. The Mayo classification and the Schatzker classification are two of the many classification schemes that are used to describe olecranon fractures.
When assessing more complicated injuries and the extent of comminution, CT imaging can be helpful.
Different Diagnosis
It’s critical to rule out any additional elbow injuries that could influence the course of treatment. An examination for open fractures of the skin is necessary. Coronoid fractures, radial head and neck fractures, radial head dislocations, and collateral ligament injuries are other commonly associated injuries.
Treatment of Olecranon Fracture
Treatment options for olecranon fractures can vary and may involve nonsurgical or surgical procedures. The physician will decide if surgery is necessary for your fracture. An operation is necessary for many olecranon fractures.
Immediate treatment options are:
- Splinting and slinging the elbow to stop it from moving
- Using ice to ease pain and reduce swelling
- Using drugs to relieve pain
Non-Surgical Treatment
A splint can be used to hold the elbow in place while it heals from a fracture if the bone fragments are not dislocated. Your doctor will take regular X-rays to ensure the bone has not moved during the healing process.
Usually, a splint is worn for six weeks before introducing mild motion. You might require surgery to realign the bones if the fracture moves during this period.
Surgical Treatment
If an olecranon fracture is displaced or open, the American Academy of Orthopedic Surgeons states that surgery is usually necessary.
Typically, an individual with an open fracture requires surgery as soon as they are diagnosed. To lower the risk of infection, they might get a tetanus injection and intravenous antibiotics before surgery.
To fix an open or displaced fracture, surgery may include:
- Cutting a hole in the elbow’s back to gain access to the bones
- Restoring the fractured bone segments to their original positions
- Applying metal plates, screws, or pins to hold the bone in place while it heals
Open fractures require preparation for surgery as quickly as possible, generally within several hours of the diagnosis, due to the increased risk of infection. In addition to receiving a tetanus shot, patients in the emergency room are given antibiotics intravenously. The surfaces of the fractured bone and the cuts from the injury are meticulously cleaned out during surgery. Usually, the bone repair is done in the same operation.
People may require a bone graft if certain areas of the bone are damaged or if a portion of the bone has been lost due to an open wound.
Open Reduction and Internal Fixation
When treating olecranon fractures, this is the method most frequently employed. The first step in the process is to reduce the bone fragments back into their proper alignment. After that, screws, wires, pins, or metal plates fastened to the outside of the bone are used to hold the bone fragments in place.
Bone Graft
A bone graft may be necessary to repair the fracture if part of the bone has been crushed or has been lost through the wound. An autograft or an allograft is a bone graft made from a different bone in your body. A synthetic material may be utilized in certain situations in place of a bone graft.
Postoperative Care
Institutions have different postoperative protocols. While deciding how long to immobilize a patient, most doctors take fracture stability, wound healing, and patient compliance into account. With the elbow in 90 degrees of flexion and the wrist in neutral, a posterior removable splint or above elbow back-slab can be used for 7–10 days following surgery. Range-of-motion exercises with the aid of gravity are performed after immobilization.
Active range of motion and strengthening starts about 6 to 8 weeks after surgery, or when radiographic signs of healing appear. After three to four months, one should be able to resume athletics or other activities requiring full, active elbow movement.
Physiotherapy Management
For optimum healing, precise post-operative care is essential. The restoration and normalization of daily living activities is the functional aim of the physiotherapist. The healing of the bones and rehabilitation will take about 12 weeks:
Stage 1 (Week 0 to 1)
- For fixation, a splint or cast is placed with the elbow flexed 60 degrees to reduce skin strain.
- Examine sensation, active and passive digit range of motion, capillary refill, and excessive swelling.
- Start the shoulder, hand, and digits’ active range of motion (splint to be kept on)
- Management of edema
- wrist exercises that are isometric
- Elbow flexion with gentle activity (no splint).
- Wrist’s active range of motion
- Instruct the patient in functional adaptations, such as using the unaffected extremity for personal hygiene tasks.
Stage 2 (Week 2 to 3)
- In a cast or splint, extension to the elbow less than 90 degrees is not allowed.
- In most cases, a splint or cast removed
- Moderately intense isometric bicep exercises
- Isotonic exercises for the fingers
Stage 3 (Week 4 to 6)
- Shoulder, elbow, and wrist range of motion, both active and active-assistive
- Avoid passive elbow range of motion.
- Isometric wrist and elbow flexion and extension exercises
- Daily living activities: use the afflicted limb for self-care and stability
Stage 4 (Week 8 to 12)
- Gradually applying weight on the afflicted limb
- Elbow flexor and extensor resistance exercises
- Range of motion in all planes for the elbow and wrist, both active and active-assistive
- Some restrictions might apply to elbow extension:
- It might be necessary to perform mild passive stretching
- A passive elbow stretch can be performed using a dynamic splint
Recovery
When an olecranon fracture is repaired with a splint, the patient may experience extreme stiffness in their elbow following the removal of the cast and may require physical therapy to restore their normal range of motion.
Six weeks may be required for people to refrain from heavy lifting or bearing weight.
After six weeks of wearing a splint, a patient may be able to start physical therapy to gradually move their elbow if they do not have a displaced fracture, which occurs when the pieces of broken bone stay in alignment.
During their recovery, people may discover that ice packs, elevation, and over-the-counter pain relievers help lessen pain.
Following surgery, patients can start gradually extending their elbow right away, under the guidance of a physical or occupational therapist.
Prognosis
Patients who receive treatment for an olecranon fracture typically experience good functional outcomes. There may be a loss of terminal extension of about 10 to 15 degrees, but this is typically not clinically significant. 96% of patients with a follow-up period of 15 to 25 years had good or excellent functional outcomes. With an approximate 1% nonunion rate, fractures heal quite quickly.
Prevention
Although there is no complete protection against elbow fractures, there are some steps you can take to lower your risk. As an example:
- While participating in sports, wear suitable safety gear.
- Regular exercise is necessary for maintaining maximum strength.
- Learn the right skills for playing sports.
- Make an effort to lessen the chance that you will fall.
Complication
Hardware Irritation: Because the proximal olecranon is subcutaneous, the most frequent complication is irritation that results in hardware removal. The literature describes a variable rate of component removal for plate fixation and TBW.
A current prospective random control study found that 22% of cases with plate fixation and 50% of cases with TBW had hardware removed. Less common and less likely to require a second operation for hardware irritation are intramedullary devices. In addition to fracture displacement and wire breakage, wire migration can also happen.
Infection: Soft tissue coverage over fixation hardware is limited due to the subcutaneous nature of the olecranon. It may be less risky to place plates on the side of the olecranon where the soft tissue envelope is stronger. K-wires, also known as Kirshner wires, have the potential to back out and cause soft tissue irritation or wound issues. The risk of the wires backing out can be decreased by burying them, rotating them 180 degrees, and engaging the distal end of the wire in the anterior cortex of the ulna.
By positioning wires at an angle of 20–30 degrees from the longitudinal plane of the ulna on the lateral side of the anterior cortex, damage to the anterior interosseus nerve and ulnar artery caused by the k-wire’s penetration can be lessened. Long pins can cause damage to the supinator muscle or biceps tendon, as well as impinge on the radial neck, which can limit supination. According to one series, patients receiving plate fixation had a higher infection rate (13% vs.0%) than those receiving tuberculosis.
Loss of Motion: Patients frequently experience a 10-15 degree loss of terminal elbow extension. Given that the functional elbow range of motion is a 30-to-130-degree arc, this is typically not clinically significant. According to one study, 39% of patients had flexion contractures greater than 10 degrees following plate fixation; however, these cases had no appreciable effect on functional outcome ratings. Although it is estimated that up to 50% of patients experience general stiffness, the function is typically unaffected.
Arthrosis: At long-term follow-up, radiographs from up to 50% of patients show degenerative changes. This is not always clinically important as 96 percent of this cohort indicated good or excellent final results. A reduction in the space between the olecranon’s tip and the coronoid may result in mal-reduction and arthrosis later on.
Heterotopic ossification: About 13% of patients may experience this.
Ulnar nerve neuritis: This is a rare side effect that happens in about 2-12% of cases. Conservative management will result in the resolution of most cases. Neurolysis and ulnar nerve transformation might be necessary in resistant cases.
Nonunion: There is a 1% chance of nonunion. Options for treatment include triceps advancement and excision, internal fixation either with or without bone graft, and elbow arthroplasty.
Malunion: This can occur extra- or intra-articularly. A comminuted fracture that is not adequately reduced can result in interarticular malunion and sigmoid notch narrowing. You’ll probably develop early-stage arthritis, which might need an arthroplasty procedure. An osteotomy is a possible treatment for extra-articular malunion, which manifests as radial head subluxation.
Summary
A fracture in the ulna bone, which forms the elbow point, is known as an olecranon fracture. A person who is struck directly in the elbow or falls on their elbow may sustain an olecranon fracture.
People may need surgery to fix the broken bone or a splint to hold the bone in place while it heals, depending on the type of fracture. Following treatment, physical therapy could aid in enhancing the elbow’s range of motion.
FAQs
What happens if an olecranon fracture is left untreated?
Untreated olecranon fractures may result in nonunion or malunion of the fractures along with chronic pain. There might be a decrease in the elbow’s typical range of motion. Additionally, you might have post-traumatic arthritis, elbow stiffness, or instability.
Can olecranon fracture heal without surgery?
There is proof that treating olecranon fractures non-operatively can be appropriate. Good results with conservative management of displaced olecranon fractures in elderly patients with low demand are reported.
How painful is an olecranon fracture?
The best position for someone with a broken arm or wrist is frequently propped up on pillows. This keeps the injured area elevated and relieves some of the strain on it thanks to gravity.
Are olecranon fractures common?
Any direct elbow impact or fall can result in an olecranon fracture. People may experience excruciating pain and lose elbow mobility. Physical therapy, surgery, or the use of a splint are possible forms of treatment.
How do you treat an olecranon fracture?
Treatment options for nondisplaced olecranon fractures include early progressive active range-of-motion exercises avoided during active extension and a beginning phase of immobilization in the posterior slab long arm splint that holds the elbow in 45–90 degrees of flexion.
Is an olecranon fracture serious?
The area surrounding the elbow’s blood vessels and nerves is not at high risk of injury. non-union. A fracture may not always heal. The screws, plates, or wires may break or shift as a result of the fracture pulling apart.
REFERENCES
- Olecranon Fracture (Elbow Fracture). (2021, August 8). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/olecranon-fracture-elbow-fracture
- Sissons, B. (2022, November 11). What to know about an olecranon fracture. https://www.medicalnewstoday.com/articles/olecranon-fracture#treatment
- Sullivan, C. W. (2023, August 14). Olecranon Fracture. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK537295/
- Olecranon Fracture. (n.d.). Physiopedia. https://www.physio-pedia.com/Olecranon_Fracture
- Olecranon Fractures – Pathophysiology – Management – TeachMeSurgery. (2023, April 29). TeachMeSurgery. https://teachmesurgery.com/orthopaedic/elbow/olecranon-fracture/
- Elbow (Olecranon) Fractures – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/elbow-olecranon-fractures
- Professional, C. C. M. (n.d.). Elbow Fractures. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22050-elbow-fractures





One Comment