Tendon Achilles Tendonitis
Introduction:
- The Achilles tendon or heel cord, also known as the calcaneal tendon, is a tendon at the back of the lower leg, and is the thickest in the human body.
- It serves to attach the plantaris, gastrocnemius (calf) and soleus muscles to the calcaneus (heel) bone.
- These muscles, acting via the tendon, cause plantar flexion of the foot at the ankle joint, and (except the soleus) flexion at the knee.
- Abnormalities of the Achilles tendon include inflammation (Achilles tendinitis), degeneration, rupture, and becoming embedded with cholesterol deposits (xanthomas).
Anatomy:
- The Achilles (Calcaneal) tendon is a common tendon shared between the gastrocnemius and soleus muscles of the posterior leg.
- It connects the two muscle groups (collectively, triceps surae) to the calcaneus bone.
- Generally, the tendon winds 90 degrees on its path towards the heel, such that the gastrocnemius attaches laterally and the soleus attaches medially.
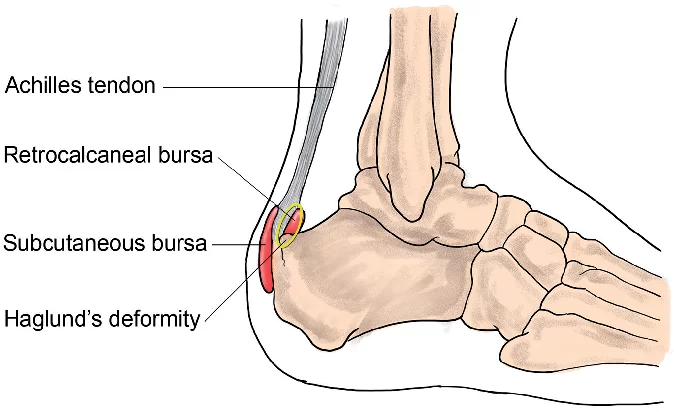
- A subcutaneous calcaneal bursa permits movement of the skin over the flexed tendon.
- A deep bursa of the Achilles tendon reduces friction to allow free movement of the tendon over the bone.
Attachment:
- The tendon provides a distal attachment site for the gastrocnemius (lateral and medial heads) as well as the soleus muscles.
- It inserts onto the posterior surface of the calcaneus (heel bone).
- The plantaris tendon also fuses with the medial side of the Achilles tendon proximal to its attachment site.
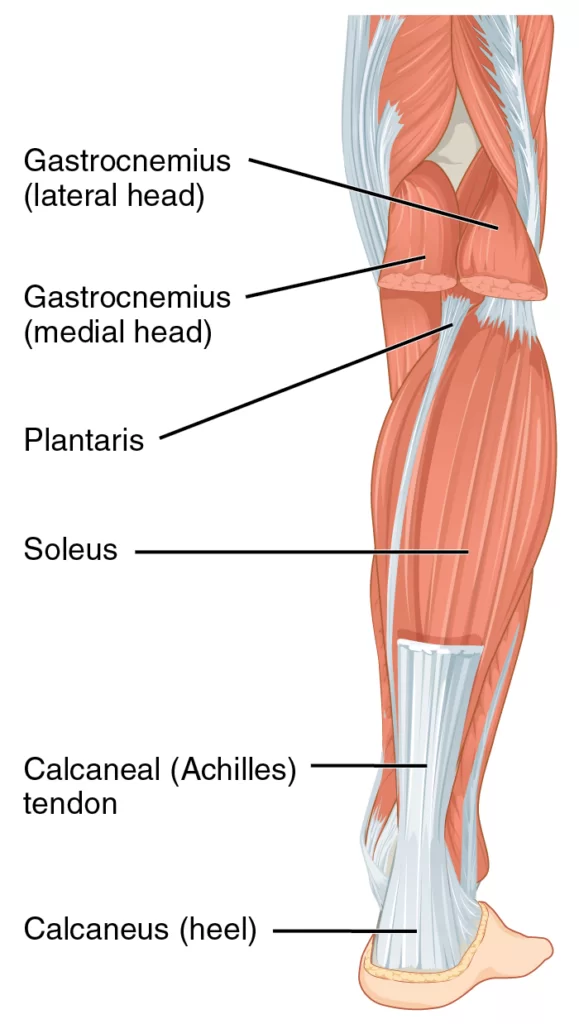
- The Achilles tendon connects muscle to bone, like other tendons, and is located at the back of the lower leg.
- The Achilles tendon connects the gastrocnemius and soleus muscles to the calcaneal tuberosity on the calcaneus (heel bone).
- The tendon begins near the middle of the calf and receives muscle fibers on its inner surface, particularly from the soleus muscle, almost to its lower end.
- Gradually thinning below, it inserts into the middle part of the back of the calcaneus bone.
- The tendon spreads out somewhat at its lower end so that its narrowest part is about 4 cm (1.6 in) above its insertion.
- The tendon is covered by the fascia and skin, and stands out prominently behind the bone; the gap is filled up with areolar and adipose tissue.
- A bursa lies between the tendon and the upper part of the calcaneus. It is about 15 centimetres (6 in) long.
- Along the side of the muscle, and superficial to it, is the small saphenous vein.
- The sural nerve accompanies the small saphenous vein as it descends in the posterior leg, traveling inferolateral to it as it crosses the lateral border of the Achilles tendon.
- The tendon is the thickest tendon in the human body.
- It can receive a load stress of 3.9 times body weight during walking and 7.7 times body weight when running.
- The blood supply to the Achilles tendon is poor, and mostly via a recurrent branch of the posterior tibial artery, and some through arterial branches passing through surrounding muscles.
Function:

- Acting via the Achilles tendon, the gastrocnemius and soleus muscles cause plantar flexion of the foot at the ankle.
- This action brings the sole of the foot closer to the back of the leg.
- The gastrocnemius also flexes the leg at the knee.
- Both muscles are innervated by the tibial nerve. Because the fibres of the tendon spiral about 90 degrees, fibres from the gastrocnemius tend to attach to the outer part of the bone, whereas fibres from the soleus tend to attach closer to the midline.
- Vibration of the tendon without vision has a major impact on postural orientation.
- The vibration of the tendon causes movement backward and the illusion of a forward body tilt in standing subjects.
- This is because vibrations stimulate muscle spindles in the calf muscles.
- The muscle spindles alert the brain that the body is moving forward, so the central nervous system compensates by moving the body backward.
Biomechanics:
- Posterior compartment muscles all pass posterior to the talocral joint axis and all planter flexors.
- The muscles in the posterior compartment are the gastrocnemius, soleus, tibialis posterior, flexordigitorum longus, and flexor hallucis longus muscles.
- The gastrocnemius muscle arises from two heads of origin on the condyles of the femur and inserts via the Achilles tendon into the most posterior aspect of the calcaneus.
- The soleus muscle is deep to the gastrocnemius originating on the tibia and fibula and inserting with the gastrominus into the posterior calcaneus.
- The two heads of the gastrocnemius and soleus muscles together are known as the triceps surae and are the strongest plantar flexors of the ankle.
- The volume of the triceps surae is strongly associated with its ability to generate torque.
- The Achilles tendon inserts perpendicularly on the calcaneus relatively far from the ankle joint axis.
- This efficient attachment provides a large moment arm to generate plantarflexion toque the Achilles tendon also passes just medial to the subtalar joint.
- However individual variation in the location of the subtalar axis can affect the ability of the muscles to supinate.
- The activity of the gastrocnemius and soleus on the weight-bearing foot helps lock the foot into a rigid lever both through direct supination of the subtalar joint and through indirect supination of the transverse tarsal joint.
- Continued plantarflexion force will raise the heel and cause elevation of the arch ( potentially assisted by the increased tension in the plantar flexors).
- Subtalar joint and through indirect supination of the transverse tarsal joint.
- Continued plantarflexion force will raise the heel and cause elevation of the arch ( potentially assisted by the increased tension in the plantar aponeurosis as the MTP JOINT extend
- Elevation of each by the triceps surae when the heel is lifted off the ground is observable in most people when they activity plantar flex the weight-bearing foot.
- The soleus and gastrocnemius together eccentrically control the dorsiflexion of the ankle while also supinating the subtalar joint after the foot is loaded instance.
- These muscles provide supination torque that contributes to making the foot a rigid lever for push-off the moment arm for plantar flexion for these muscles is so muscles is so small that they provide only 5% of the total plantar flexor force at the ankle.
- The plantaris muscle is so small that its function can essentially disregarded.
Clinical significance:
Inflammation:
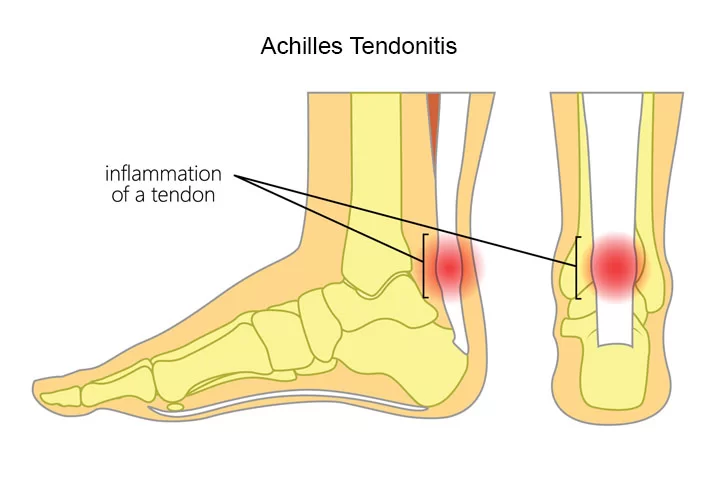
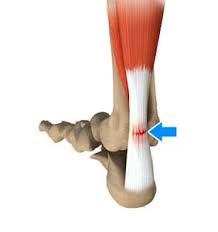
- Achilles tendinitis Inflammation of the Achilles tendon is called Achilles tendinitis.
- Achilles tendinosis is the soreness or stiffness of the tendon, particularly worse when exercising, and generally due to overuse.
Symptoms:
- Pain and swelling around the affected tendon.
- The pain is typically worse at the start of exercise and decreases thereafter.
- Stiffness of the ankle may also be present.
- Onset is generally gradual.
Causes:
- Overuse of muscle such as running.
Risk factor:
- Trauma
- A lifestyle that includes little exercise
- High-heel shoes, rheumatoid arthritis,
- Medications of the fluoroquinolone or steroid class.
Diagnosis:
- It is generally based on symptoms and examination.
- While stretching and exercises to strengthen the calf are often recommended for prevention, evidence to support these measures is poor.
Treatment:
- Typically involves rest,
- Ice,
- Non-steroidal anti-inflammatory agents (NSAIDs)
- Physical therapy.
- A heel lift or orthotics may also be helpful.
- In those in which symptoms last more than six months despite other treatments, surgery may be considered.
- Achilles tendonitis is relatively common.
Degeneration:

- Achilles tendon degeneration (tendinosis) is typically investigated with either MRI or ultrasound.
- In both cases, the tendon is thickened and may demonstrate surrounding inflammation by virtue of the presence of paratenonitis, retrocalcaneal, or retro-Achilles bursitis.
- Within the tendon, increased blood flow, tendon fibril disorganization, and partial thickness tears may be identified.
- Achilles tendinosis frequently involves the mid portion of the tendon but may involve the insertion, which is then known as enthesopathy.
- Though enthesopathy may be seen in the context of advancing age, it is also associated with arthritis such as gout and the seronegative spondyloarthritis.
- Achilles tendinosis is a known risk factor for calf muscle tears.
Rupture:

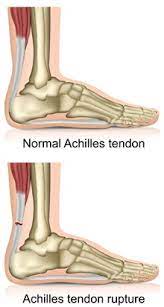
- Achilles tendon rupture:
- Achilles tendon rupture is when the Achilles tendon breaks.
Symptoms:
- The sudden onset of sharp pain in the heel.
- A snapping sound may be heard as the tendon breaks and walking becomes difficult.
- Rupture typically occurs as a result of a sudden bending up of the foot when the calf muscle is engaged, direct trauma, or long-standing tendonitis.
Diagnosis:
- It is typically based on symptoms and examination and supported by medical imaging.
Causes:
- Your Achilles tendon helps you point your foot downward, rise on your toes, and push off your foot as you walk.
- You rely on it virtually every time you walk and move your foot.
- Rupture usually occurs in the section of the tendon situated within 2 1/2 inches (about 6 centimeters) of the point where it attaches to the heel bone.
- This section might be prone to rupture because blood flow is poor, which also can impair its ability to heal.
- Ruptures often are caused by a sudden increase in the stress on your Achilles tendon. Common examples include:
- Increasing the intensity of sports participation, especially in sports that involve jumping.
- Falling from a height.
- Stepping into a hole.
Risk factors:
- Factors that may increase your risk of Achilles tendon rupture include :
- Age: The peak age for Achilles tendon rupture is 30 to 40.
- Sex: Achilles tendon rupture is up to five times more likely to occur in men than in women.
- Recreational sports: Achilles tendon injuries occur more often during sports that involve running, jumping, and sudden starts and stops — such as soccer, basketball, and tennis.
- Steroid injections: Doctors sometimes inject steroids into an ankle joint to reduce pain and inflammation. However, this medication can weaken nearby tendons and has been associated with Achilles tendon ruptures.
- Certain antibiotics: Fluoroquinolone antibiotics, such as ciprofloxacin (Cipro) or levofloxacin (Levaquin), increase the risk of Achilles tendon rupture.
- Obesity: Excess weight puts more strain on the tendon.
- Achilles tendon rupture occurs in about 1 per 10,000 people per year.
Prevention:
Stretching before activity.
Treatment:
- surgery or casting with the toes somewhat pointed down.
- Relatively rapid return to weight bearing (within 4 weeks) appears okay.
- The risk of re-rupture is about 25% with casting. If appropriate treatment does not occur within 4 weeks of the injury outcomes are not as good.
Xanthomas:

- Tendon xanthomas are cholesterol deposits that commonly develop in the Achilles tendon of people with lipid metabolism disorders such as familial hypercholesterolemia.
Causes:
- Xanthomas of the Achilles tendon are caused by very high cholesterol or triglyceride levels.
- High levels of cholesterol and triglycerides can lead to heart disease, so the appearance of xanthomas is a strong indicator that you should visit your doctor to check your heart health.
- If you suffer from familial hypercholesterolemia, a genetic disorder characterized by high cholesterol levels, you have an increased chance of developing xanthomas.
Symptoms:
- Xanthomas of the Achilles tendon appear as waxy, yellowish-to-white bumps under the skin along the Achilles tendon.
- At times, the xanthomas will not be visible without close inspection.
- If you are trying to determine if a bump near your heel is Achilles tendon xanthomas, determine if the bump is moving with the tendon as you flex it. Xanthomas of the Achilles tendon will move with the tendon.
Peritendinitis and Paratendinitis:
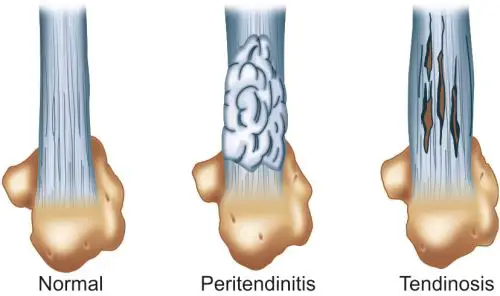
- Confusing terminology persists in describing the inflammatory and overuse changes of the structures surrounding the Achilles tendon.
Paratenonitis:
- It is popularly used to indicate inflammation of the paratenon.
- To better reflect the location of the abnormality, that surrounds the Achilles tendon.
- some authors prefer peritendinitis as a more accurate descriptor.
Peritendinitis:
- It can accompany tendon degeneration, but can also occur without underlying tendon pathology.
- This condition is activity-related and is most commonly seen in active, athletic patients.
- It often results from overuse injuries or abnormal biomechanics and is commonly an overtraining injury, especially in marathon runners.
- Fibrinous exudate, fibroblastic changes, and infiltration by inflammatory cells result in a thickened paratenon.
Diagnosis:
- It is typically made clinically based on the findings of swelling, pain, crepitus, tenderness, and warmth.
- On MRI, peritendinitis demonstrates hyperintense signal on STIR and fat-suppressed T2-weighted images surrounding or partially surrounding the Achilles tendon .
- Inflammation can also be seen within the pre-Achilles fat pad, with or without underlying Achilles tendon pathology.
- Based on its location adjacent to, but not surrounding the tendon, this has been described as Achilles paratendiniti On MRI, the fat signal of the pre-Achilles fat pad immediately adjacent to the Achilles tendon is replaced by increased signal on fluid-sensitive sequences, and the normal high signal of fat on T1-weighted images is replaced by intermediate signal.
Mid-substance Achilles tendon:
- The most common abnormality involving the Achilles tendon mid-substance is tendinosis.
- Tendinosis is a degenerative, non-flammatory process, most closely associated with aging 31.
- Combinations of hypoxic, mucoid, calcific, and fatty degeneration occur with aging or with overuse, resulting in a disorganized collagen structure and increased tendon stiffness.
- With progression, collagen fiber separation and disruption occur with the coalescence of mucoid material between the collagen fibers, which can progress to microtears, intrasubstance tears, surface partial tears, and even complete tears. Although all types of degeneration are frequently found, hypoxic and mucoid degeneration are the most prevalent degenerative findings in ruptured Achilles tendons.
- Hypoxic degenerative changes are felt to be caused by ischemia related to relative hypovascularity in the critical zone of the tendon.
- Mucoid degeneration results in large myxoid patches and vacuoles between the degenerated tendon fibers.
- The predominant hypoxic changes often present with multiple symptomatic episodes while mucoid changes of the Achilles tendon often remain clinically silent.
- A typical presentation of tendinosis is the middle-aged athlete who presents following an increase in training duration, intensity, and frequency with pain in the mid portion of the tendon.
Physical examination:
- The patient presents with swelling after activity and pain with active and passive motion.
- Visible or palpable tendon enlargement or a knot, which is painful to compression are common findings.
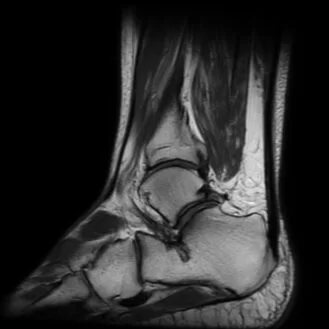
MRI:
- The changes associated with hypoxic degeneration tend to result in tendon enlargement without internal signal changes.
- Mucoid degeneration leads to enlargement with an altered T2-weighted signal, reflecting mucoid deposits and interstitial tears.
- When present, interstitial tears present as a longitudinally oriented linear increased signal on T1-weighted, proton-density-weighted, and T2-weighted STIR sequences, with intact surrounding fibers.
- Achilles tendon enlargement may also be seen in rheumatoid arthritis and gout.
- Xanthomas are the result of lipomatosis and are frequently correlated with a family history of coronary artery disease and certain metabolic diseases, in particular type IIa and type III hyperlipidemia.
- Typically, there is internal fat or intermediate signal enlarging the tendon and spreading the tendon fascicles, resulting in increased T1 and T2-weighted signal and a stippled pattern on the cross-section, but occasionally, the internal signal may be subtle.
Insertional Pathologies:
Insertional Tendinopathy:
- Insertional Achilles tendinopathy frequently coexists with adjacent soft tissue and osseous pathology.
- In contrast to tendinosis that is typically found in the tendon mid-substance, insertional tendinopathy is thought to have an inflammatory component initially, thus the frequent use of the term “insertional tendinitis” in describing this process.
- However, in its chronic form, histopathologic changes of inflammation are commonly no longer present and some authors prefer to use the term insertional tendinopathy or even tendinosis.
- Overuse is contributory with a reported prevalence of up to 18% in runners and 9% in dancers.
- Posterosuperior bony prominence of the calcaneus (Haglund’s deformity) is felt to contribute to the development of insertional Achilles tendinopathy.
causes :
- Inflammatory arthropathies,
- Corticosteroid use
- Diabetes
- Hypertension
- Obesity
- Gout
- Fluroquinolone antibiotics.
- Patients typically present with stiffness and a palpable, irritated, painful bump at the Achilles tendon insertion.
- Enthesophyte formation at the Achilles tendon insertion or calcification/ossification within the distal Achilles tendon are common and may lead to palpable abnormalities.
MRI:
- MRI depicts distal tendon thickening with ill-defined tendon signal heterogeneity.
- Partial tears demonstrate hyperintense defects on fluid-sensitive sequences.
- Edema within enthesophytes correlates with more acute symptoms.
- Retrocalcaneal bursitis is a frequent accompanying finding.
Haglund’s Deformity:

- Prominence of the posterosuperior angle of the calcaneus, referred to as a Haglund’s deformity.
- It is commonly described as a contributor to retrocalcaneal bursitis and insertional Achilles tendon pathology.
- While prominent contours of the posterosuperior angle of the calcaneus are recognizable as pathological studies have failed to demonstrate radiographic criteria that quantify the size at which the convex posterosuperior angle of the calcaneus becomes symptomatic and using various methods of radiographic measurement.
- Haglund’s deformities are found equally in symptomatic and asymptomatic individuals.
- Nevertheless, in symptomatic patients, the prominence of the posterosuperior angle of the calcaneus is felt by many to play a role in retrocalcaneal bursitis and distal Achilles tendinopathy, and when surgical intervention is necessary, relatively small bony convexities are often removed.
Retrocalcaneal Bursitis:

- In retrocalcaneal bursitis, the bursa between the posterosuperior calcaneus and the Achilles tendon becomes inflamed, hypertrophied, and adherent to the Achilles tendon.
- Haglund’s deformity has been associated with retrocalcaneal bursitis.
- Retrocalcaneal bursitis is commonly seen in runners resulting from repeated compression between the calcaneus and Achilles tendon with dorsiflexion of the ankle and often occurs without any calcaneal deformity.
- The mechanism of irritation is further exacerbated by uphill running, which results in increased and repetitive ankle dorsiflexion.
- Hindfoot varus and a rigid plantarflexed first ray also contribute to the development of retrocalcaneal bursitis.
- Bilateral involvement should alert the clinician to the possibility of a systemic inflammatory process, such as rheumatoid arthritis which may result in retrocalcaneal bursitis in up to 10% of patients.
- The clinical presentation is similar to insertional tendinitis with pain near the calcaneal insertion.
Causes:
- Are over 65 years old.
- Participate in high-activity sports.
- Don’t stretch properly before exercising.
- Have tight muscles.
- Have a job that requires repeated movement and stress on the joints.
Symptoms:
- The main symptom of retrocalcaneal bursitis is heel pain.
- You might only feel pain when you put pressure on your heel.
Other symptoms may include:
- Swelling around the back of your heel area.
- Pain when leaning back on your heels.
- Pain in calf muscles when running or walking.
- Stiffness.
- Red or warm skin on the back of the heel.
- Loss of movement.
- Crackling sound when flexing the foot.
- Shoes becoming uncomfortable.
A positive two-finger squeeze test:

It is indicates retrocalcaneal bursitis
It is performed with pressure applied by two fingers medially and laterally just superior and anterior to the Achilles insertion.
MRI:
- The retrocalcaneal bursa is distended with fluid signal and appears hyperintense on fluid-sensitive sequences.
- Enlargement of the bursal anteroposterior dimensions to greater than 2mm is consistent with bursitis.
- There is often an associated element of inflammation in the adjacent paratenon and Achilles tendon insertion.
- Associated partial Achilles tendon tear, peritendinitis, tendinopathy, or ossification is common.
Retro-Achilles Bursitis:
- The retro-Achilles bursa is an adventitious bursa that develops as a response to friction between the posterior aspect of the calcaneus or the Achilles tendon and the skin.
- It is most often seen at the posterolateral aspect of the calcaneus and is frequently associated with tight or poorly fitted shoes with a rigid heel counter.
Causes :
- A retrocalcaneal bursa mat occurs traumatically from a fall.
- A sport-related impact contusion.
- It can also present as a gradual onset due to repetitive trauma to the bursa from activities including running or excessive loading.
- Overtraining in an athlete.
- Tight or poorly fitting shoes that produce excessive pressure at the posterior heel.
- Haglund deformity.
- Altered joint axis.
- Inflammation of the calcaneal bursae is most commonly caused by repetitive (cumulative) trauma.
- Overuse
- The condition is aggravated by pressure, such as when athletes wear tight-fitting shoes.
- Retrocalcaneal bursitis may also be associated with conditions such as gout, rheumatoid arthritis, and seronegative spondyloarthropathies.
- In some cases, retrocalcaneal bursitis may be caused by bursal impingement between the Achilles tendon and an excessively prominent posterosuperior aspect of the calcaneus (Haglund deformity).
- In Haglund disease, impingement occurs during ankle dorsiflexion.
Signs and Symptoms:
- Pain at the back of the heel, especially when running uphill.
- Pain may get worse when rising on the toes (standing on tiptoes).
- Tenderness at the back of the heel.
- Swelling at the back of the heel.
- Increase in pain in activities that load the calf.
Haglund’s syndrome:

- The term Haglund’s syndrome was originally described as a radiographic combination of retrocalcaneal bursitis, insertional Achilles tendinitis, and retro Achilles bursitis.
- This may be associated with a prominent bursal projection of the posterosuperior calcaneus (Haglund’s deformity).
- Ventral tears of the Achilles tendon and insertional enthesophytes may also be seen.
- This condition was attributed to poorly fitting or tight low-back shoes, and the palpable soft tissue and osseous prominence that develops at the lateral aspect of the Achilles insertion was referred to as a “pump bump”.
Achilles Tendon Tears:
- Achilles tendon ruptures occur with a bimodal age distribution, with the first peak in 25-40-year-old males and the second peak in those older than 60 years.
- It is rare to tear a normal tendon.
Risk factors:
- Diffuse tendon degeneration
- Inflammatory conditions
- Previous tendon repair on the contralateral side.
- In one study fluoroquinolone usage resulted in a 4-fold increased risk of rupture, and concomitant use of corticosteroids resulted in a 10-fold increased risk.
- Haglund’s deformity may result in mechanical irritation and degeneration, raising the risk of rupture.
- The most common presentation is a 40-year-old weekend warrior who experiences a sudden pop in the distal leg after pushing off from a dorsiflexed position while running or jumping.
- In the US, basketball accounts for the most injuries, followed by tennis and football.
- In older patients, rupture may occur at sites of chronic degeneration during routine daily activities.
Physical findings:
- Bruising around the posterior ankle
- Weakened plantar flexion
- Limp
- Inability to bear weight.
Diagnosis:
Positive Thompson test:
- Decreased plantar flexion strength
- Palpable defect roughly 2 to 6 cm proximal to the insertion
- Increased passive ankle dorsiflexion.
- A positive Thompson test occurs when compression of the calf does not result in passive plantar flexion of the foot.
- Approximately 25% of acute ruptures are misdiagnosed due to a false-negative Thompson test, a large hematoma, or plantar flexion secondary to extrinsic foot flexors.
- Partial tears or tendon ruptures can occur anywhere along the Achilles tendon.
MRI:
- Partial tears demonstrate alteration in architecture with interruption of tendon fibers.
- Heterogeneous T2 hyperintense signal fills the tendon defect and outlines the ends of the torn fibers, which can partially retract.
- 60-year-old female with posterior pain after a fall.
- A sagittal STIR image demonstrates a high-grade partial tear (arrow) extending to the anterior surface of the Achilles tendon with thickening and heterogeneity of the Achilles tendon bordering the tear.
- Complete tears of the Achilles tendon resulting in tendon discontinuity with fluid or heterogeneous signal hematoma filling the tendon gap, and torn tendon fibers are distracted or overlapping.
- Peritendinous hemorrhage and edema are present with recent tendon tears.
- As the tear ages, organization of the hematoma, granulation tissue, and eventual scar tissue can make detection of the torn tendon edges difficult.
- Chronic ruptures often demonstrate muscle atrophy with further retraction of the tendon.
- Fatty infiltration portends a poorer prognosis for surgical repair.
- Thus, when reporting tears, it is essential to describe the size of the tendon gap, the quality of the torn tendon, an estimation of cross-sectional involvement, and the presence of atrophy of the soleus and gastrocnemius muscles.
- Most Achilles tendon tears occur in the relatively avascular zone located 2-6 cm from the insertion.
- Insertional tears are less common but partial tears or ruptures can occur as a result of incompletely treated insertional tendinitis.
Achilles tendon rupture:
- Rarely they may be iatrogenic or associated with systemic diseases like diabetes.
- Proximal tears are most commonly partial tears involving the medial head of the gastrocnemius myotendinous junction.
- Proximal ruptures (complete tears) at the myotendinous junction are less common.
Cause:
- Your Achilles tendon helps you point your foot downward, rise on your toes, and push off your foot as you walk.
- You rely on it virtually every time you walk and move your foot.
- Rupture usually occurs in the section of the tendon situated within 2 1/2 inches (about 6 centimeters) of the point where it attaches to the heel bone.
- This section might be prone to rupture because blood flow is poor, which also can impair its ability to heal.
- Ruptures often are caused by a sudden increase in the stress on your Achilles tendon.
Common examples include:
- Increasing the intensity of sports participation, especially in sports that involve jumping.
- Falling from a height.
- Stepping into a hole.
Symptoms:
- The feeling of having been kicked in the calf.
- Pain, possibly severe, and swelling near the heel.
- An inability to bend the foot downward or “push off” the injured leg when walking.
- An inability to stand on the toes of the injured leg.
- A popping or snapping sound when the injury occurs.
Risk factors:
- Age: The peak age for Achilles tendon rupture is 30 to 40.
- Sex: Achilles tendon rupture is up to five times more likely to occur in men than in women.
- Recreational sports: Achilles tendon injuries occur more often during sports that involve running, jumping, and sudden starts and stops — such as soccer, basketball, and tennis.
- Steroid injections: Doctors sometimes inject steroids into an ankle joint to reduce pain and inflammation. However, this medication can weaken nearby tendons and has been associated with Achilles tendon ruptures.
- Certain antibiotics: Fluoroquinolone antibiotics, such as ciprofloxacin (Cipro) or levofloxacin (Levaquin), increase the risk of Achilles tendon rupture.
- Obesity: Excess weight puts more strain on the tendon.
Aetiology and pathophysiology:
- Tendon injuries can be acute or chronic. Clearly, in acute trauma extrinsic factors predominate, whereas in chronic disorders intrinsic and extrinsic factors commonly interact.
- Examples of intrinsic factors are tendon vascularity, gastrocnemius–soleus dysfunction, age, gender, body weight and height, pes cavus, and lateral ankle instability.
- Excessive motion of the hindfoot in the frontal plane, especially a lateral heel strike with compensatory pronation, is thought to cause a ‘whipping action’ on the Achilles tendon and predispose it to tendinopathy.
- Also, forefoot varus is frequent in patients with Achilles tendinopathy.
- Extrinsic factors that may predispose to Achilles tendinopathy in athletes are changes in training pattern, poor technique, previous injuries, footwear, and training on hard, slippery, or slanting surfaces.
- Excessive loading of tendons during vigorous physical training is regarded as the main pathological stimulus for degeneration. Tendons respond to repetitive overload beyond the physiological threshold by inflammation of their sheath, degeneration of their body, or a combination of the two.
- Whether different stresses induce different responses remains unclear.
- Active repair of fatigue damage must occur, or tendons will weaken and eventually rupture.
- The repair mechanism is probably mediated by resident tenocytes that continually monitor the extracellular matrix.
- Failure to adapt to recurrent excessive loads results in the release of cytokines, leading to further modulation of cell activity.
- Tendon damage may even result from stresses within physiological limits, since frequent microtrauma may not allow enough time for repair.
- Microtrauma can also result from non-uniform stress within tendons, producing abnormal load concentrations and frictional forces between the fibrils, with localized fibre damage.
- The aetiology of tendinopathy remains uncertain and many factors have been implicated.
- 1 including free radical damage occurring on reperfusion after ischaemia, hypoxia, hyperthermia, and impaired tenocyte apoptosis.
- In animals, tendinopathy can be induced by local administration of cytokines and prostaglandins.
- Fluoroquinolones have also been implicated: ciprofloxacin enhances interleukin-1 ß mediated release of matrix metalloproteinase (MMP3) release, inhibits tenocyte proliferation, and reduces collagen and matrix synthesis.
- Changes in the expression of genes regulating cell–cell, and cell–matrix interactions have been reported, with down-regulation of MMP3 mRNA in tendinopathic Achilles tendon samples.
- Type I and type III collagen mRNAs have been found at higher levels in tendinopathic samples than in normal samples.
- In tendinopathic Achilles tendons, upregulation of MMP2 and vascular endothelial growth factor has been described, whilst MMP3 was down regulated.
- Imbalance in MMP activity in response to repeated injury or mechanical strain may result in tendon degeneration.
- The main symptom of Achilles tendinopathy is pain, but again the underlying mechanism is not fully understood.
- In the past it was assumed to arise through inflammation or via collagen fibre separation or degeneration, but chronically painful Achilles tendons show no evidence of inflammation, and some that show clear intratendinous defects on MRI or ultrasound are not painful.
- Since tendinopathies are degenerative rather than inflammatory conditions, pain may originate from a combination of mechanical and biochemical factors.
- Microdialysis sampling revealed twofold higher lactate levels in tendinopathic tendons than in controls. High concentrations of the neurotransmitter glutamate, but no increase in the proinflammatory prostaglandin PGE2, have been found in Achilles and patellar tendinopathy.
- Several studies have confirmed the occurrence of sensory neuropeptides in both animal and human tendons, and substance P has been found in tendinopathic Achilles tendons.
- Endogenous opioids provide a peripheral antinociceptive system, and morphine inhibits the release of substance P from peripheral sensory nerve endings.
- Under normal conditions, a balance probably exists between nociceptive and antinociceptive peptides.
Achilles tendonitis:
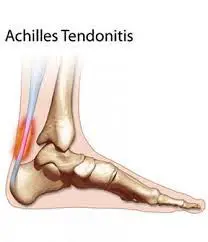
- Achilles tendonitis is an overuse syndrome associated with the calf muscles and the heel.
- The Achilles tendon is made up of the lower end of the two muscles in the calf on the back of the lower leg.
- These muscles assist in knee movement, and because they attach to the heel, they also move the foot.
- Achilles tendonitis is typically associated with foot movement.
- Pain with walking can be described as burning and radiating through the entire tendon.
- There may be some tightness in the tendon and calf muscles, and the area will be tender to the touch. Inflammation, warmth around the area, and swelling are all common signs of Achilles tendonitis.
- The main cause of Achilles tendonitis is repeated over-stretching movements in the calf muscle, which lead to micro tears that, over time, can cause chronic inflammation and eventually degeneration of the tissue.
- Other causes include tight hamstring muscles, tight calf muscles, a high foot arch, poor foot biomechanics, poor training mechanics, running on uneven surfaces, and improperly fitted footwear that does not adequately stabilize the heel.
Diagnosis:
- During the physical exam, your doctor will gently press on the affected area to determine the location of pain, tenderness, or swelling.
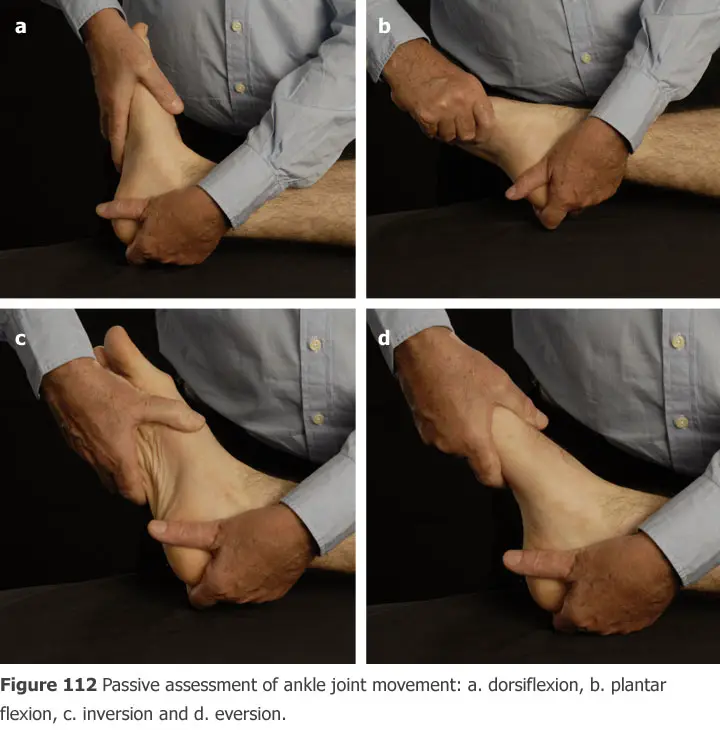
- He or she will also evaluate the flexibility, alignment, range of motion, and reflexes of your foot and ankle.
X-rays:

- While X-rays can’t visualize soft tissues such as tendons, they may help rule out other conditions that can cause similar symptoms.
Ultrasound:
- This device uses sound waves to visualize soft tissues like tendons.
- Ultrasound can also produce real-time images of the Achilles tendon in motion, and color-Doppler ultrasound can evaluate blood flow around the tendon.
Magnetic resonance imaging (MRI):
- Using radio waves and a very strong magnet, MRI machines can produce very detailed images of the Achilles tendon.
Treatment:
Phase – 1:
Early injury protection:
- Pain reduction & anti-inflammation phase.
- As with most soft tissue injuries, the initial treatment is rice – rest, ice, compression, and elevation.
- In the early phase, you will be unable to walk without a limb, so your Achilles tendon needs some active rest from weight-bearing loads, you may need to be non or partial-weight-bearing, utilize crutches, a wedged Achilles walking boot, or heel wedges to temporally relieve some of the pressure on the Achilles tendon.
- Your physiotherapist will advise you on what they feel is best for you.
- Ice is a simple and effective modality to reduce your pain and swelling. please apply for 20-30 minutes each 3 to 4 hours during the initial phase or when your is warm or hot.
- Anti-inflammatory medication and natural substances eg mica may help reduce your pain and swelling.
- However, it is best to avoid anti-inflammatory drugs during the initial 48 to 72 hours when they may encourage additional bleeding.
- Most people can tolerate paracetamol as a pain-reducing medication.
- As you improve a kinesio style supportive taping will help to both supports the injured soft tissue.
Phase-2:
Regain full range of motion:
- If you protect your injured Achilles tendon appropriately the torn tendon fiber will successfully reattach.
- Mature scar formation takes at least six weeks.
- During this time period, you should aim to optimally remold your scar tissue to prevent a poorly formed scar that will re-tear in the future.
- It is important to lengthen and orientate your healing scar tissue via massage muscle stretches, neurodynamic mobilization, and eccentric exercises.
- Sings that you have full soft tissue extensibility include being able to walk without a limb and being able to perform Achilles tendon stretches with a similar end-of-range stretch feeling.
Phase-3:
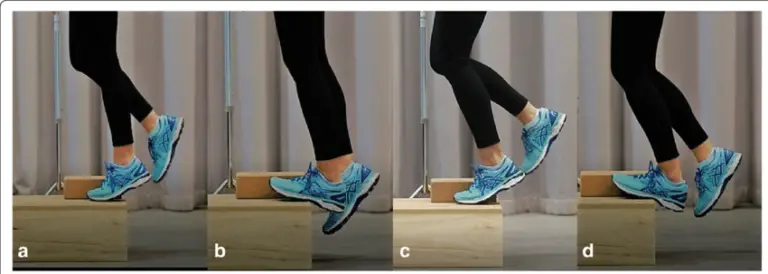
Restore eccentric muscle strength:
- The calf muscle works in two directions.
- They push you up concentric and control you down eccentrically.
- Most Achilles tendon injuries occur during the controlled lengthening phase. your physiotherapist will guide you on eccentric calf strengthening programmer when your injury healing allows.
Phase-4:
Restore concentric muscle strength:
- Calf strength and power should gradually progress from non-weight bear to partial and then full-weight bear and resistance-loaded exercises.
- You may also require strengthening for your other leg, gluteal, and lower core muscles depending on your assessment findings. your physiotherapist will guide you.
Phase:5
Normalize foot biomechanics:
- Achilles tendon injuries can occur from poor foot biomechanics eg flat foot.
- In order to prevent a recurrence. Your foot will be assessed.
- In some instances. you may require a foot orthotic or you may be a candidate for the active foot posture stabilization program.
Phase 6:
Restore high speed, power, preconception & agility:
- Most Achilles tendon injuries occur during high-speed activities, which place enormous force on your body (contractile and non-contractile).
- In order to prevent a recurrence return to your sport.
- Your physiotherapist will guide you with exercises to address these important components of rehabilitation to both prevent a recurrence and improve your sporting performance.
- Depending on what your sport or lifestyle entails, a speed, agility, preconception, and power programmer will be customized to prepare you for light sport-specific training.
Phase: 7
Return to sport:
- Depending on the demands of your chosen, you will require a specific sport, you will require specific exercises, and a progressed training regime to enable a safe and injury-free return to your chosen sport.
- Your physiotherapist will discuss your goals, time frames, and training schedules with you to optimize you for a complete return to sport.
- The perfect outcome will have you performing at full speed, power, agility, and function with the added knowledge that a thorough rehabilitation programmer has minimized your chance of future injury.
Stage:
- Acute stage.
- Sub-acute stage.
Acute stage:
- Ice massage or ice pack.
- Deep transverse friction massage, if not painful.
- Pulse ultrasounds.
- Shock-absorbing heel cushion or appropriate heel raise.
- Gentle range relaxed passive movements to the raise.
- Gentle range relaxed passive movements in the ankle and foot.
- Resisted toe movements with the foot in the neutral position.
- Avoidance of weight-bearing or straining activities.
- Non-weight-bearing exercise.
Sub-acute phase:
- Passive full-range stretching to avoid adhesion.
- Pulsed ultrasound to resolve adhesion and to improve the tendon-extensibility.
- Gradual signal leg weight bearing is to be initiated against wall bars with the knee in flexion to avoid undue stretching.
- To be progressed to bilateral toe standing, jogging, and spot running.
- Proper gait training.
Physiotherapy Management:
- It is good to educate your patients on activity modification and counsel them appropriately.
- For patients with non-acute Achilles tendinopathy, clinicians should advise that complete rest is not indicated and that they should continue with their recreational activity within their pain tolerance while participating in rehabilitation.
- Clinicians may counsel patients with Achilles tendinopathy. Key elements of patient counseling could include.
- Theories supporting the use of physical therapy and the role of mechanical loading.
- Modifiable risk factors, including body mass index and shoe wear.
- Typical time course for recovery from symptoms.
Adjunct Therapies:
- In combination with approaches to optimize biomechanics and prescribe exercise therapy, adjunct therapies may be used.
- These forms of therapy usually cannot resolve or prevent injury, they are used more for symptom management.
Manual Therapy:
- There is no clinical evidence but there is expert-level consensus to support the use of joint mobilizations in the acute stage if assessment reveals joint restriction.
- There is a small amount of clinical evidence and more substantial expert-level consensus to support the use of joint mobilizations in the chronic stage if assessment reveals joint restriction May consider using manual therapy after a comprehensive evaluation of the hip, knee, foot, and ankle reveals joint dysfunction.
- In the ankle, mobilizations can be used for dorsiflexion limitation of the talocrural joint and varus- or valgus limitation of the subtalar joint.
- The effectiveness of deep cross friction is not scientifically proven and gives limited results.
- There is a small amount of clinical evidence to support the use of soft tissue techniques, such as friction, in the chronic stage.
- May consider a trial of soft tissue techniques, such as friction, in the chronic stage.
Electrotherapy Modalities:
- There is conflicting evidence to support the use of Extracorporeal Shock Wave Therapy (ESWT) in the chronic stage.
- There is evidence suggesting that the outcomes are dependent upon the dosage of the shock wave energy (EFD – energy flux density = mJ/mm²), rather than the type of shock wave generation (focused vs. radial ESWT).
- There is also evidence that the use of anesthetic required in high-energy protocols decreases the effectiveness of ESWT.
- Therefore, using low-energy ESWT protocols without the need for anaesthetic is recommended as more practical, more tolerable, and less expensive with equivalent results.
- Low-energy ESWT protocols can apply to both focused and radial ESWT.
- Consider a trial of ESWT in the chronic stage, especially if other interventions have failed, at the following parameters:
-Low energy SWT: EFD = 0.18 – 0.3 mJ/mm² (2-4 Bars)
-2000-3000 shocks
-15-30 Hz
-3-5 sessions, weekly intervals.
- There is no clinical evidence to support the use of Ultrasound and Low-Level Laser Therapy.
Iontophoresis :
- There is a small amount of evidence to support the application of iontophoresis using dexamethasone in the acute stage but not in the chronic stage.
- The role of iontophoresis is still investigational.
- May consider, in the acute stage, a trial of iontophoresis, 0.4% dexamethasone (aqueous), 80 mA-min; 6 sessions over 3 weeks.
- A program of concentric-eccentric exercises should be continued in combination with iontophoresis if exercise loading is tolerated.
Taping:

- Antipronation taping is supported by expert opinion, not clinical evidence.
- May consider using taping, possibly prior to orthotics in the acute stage.
- Clinicians should not use therapeutic elastic tape to reduce pain or improve functional performance in patients with Achilles tendinopathy.
- Clinicians may use rigid taping to decrease strain on the Achilles tendon and/or alter foot posture in patients with Achilles tendinopathy.
Night Splints:

- There is expert opinion to support the use of night splints and braces in the acute stage and a moderate amount of evidence against the use of night splints and braces in the chronic stage.
- Consider a trial of night splints and braces in the acute stage but NOT using night splints and braces in the chronic stage in conjunction with exercise.
Dry Needling:

- Clinicians may use combined therapy of dry needling with an injection under ultrasound guidance and eccentric exercise to decrease pain for individuals with symptoms greater than 3 months and increased tendon thickness.
Ice pack:
- Appling tissue to the tendon
- When in pain or after exercising
- It can alleviate pain and inflammation.
Resting:
- This gives the tissue time to heal.
- The type of rest needed depends on the severity of the symptoms.
- In mild cases, it may mean reducing the intensity of a workout, but in severe cases, it might require rest for days or weeks.
Elevating of the foot:
Keeping the foot raised above the heart can reduce swelling.
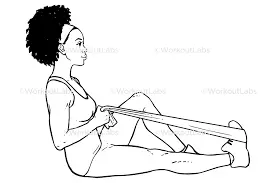
Exercise and stretching:
A physical therapist can teach stretching exercises to improve flexibility and increase strength. this may help the Achilles tendon to heal and prevent future injury. physical therapy is normally more effective for noninsertionally Achilles tendinitis.
FAQ
What is the best way to treat Achilles tendonitis?
The best ways to treat Achilles tendonitis are:
Rest.
Ice.
Nonsteroidal anti-inflammatory drugs (NSAIDs) to relieve pain eg. ibuprofen
Exercises for your calf muscles – Stretch and Strength Exercise
Physical therapy.
Can you walk with Achilles pain?
Your tendon can probably withstand some walking at this time, but it might not be able to handle all of it. By keeping yourself active and restricting your walking and other activities to a level that doesn’t exacerbate your symptoms, you can aid in the healing of your Achilles tendon.
Is it OK to massage Achilles tendonitis?
One effective therapy for Achilles tendinopathy is pressure massage. When compared to eccentric activity therapy, pressure massage produces comparable outcomes. The results were not improved by combining the therapies.
Is Achilles tendonitis serious?
Under your doctor’s guidance, the majority of instances of Achilles tendinitis may be managed with quite straightforward at-home treatment. In most cases, self-care techniques are required to stop recurrent episodes. Severe instances of Achilles tendinitis can result in tendon ruptures or tears, which may need to be surgically repaired.
What worsens Achilles tendonitis?
Being overweight may exacerbate the issue. footwear: wearing high heels or shoes with little support when jogging or walking might raise the risk. Obesity and overweight: Being overweight puts additional strain on the Achilles tendon as well as other body components.
How do you sleep with Achilles tendonitis?
With your heel and ankle flexed at the ideal angle while you sleep, a standard night splint or Sock Night Splint can help your Achilles tendon become more flexible and aid in recovery. Achilles tendonitis-related stiffness and morning discomfort can also be lessened using a sleep splint.
How do you treat the Achilles tendon naturally?
To treat Achilles tendon naturally:
Calf Stretch
Calf Strength Exercise
Hot Pack
Ice Pack
Vitamin E Oil
Turmeric
Resting The Affected Leg
Gentle Massage
Avoid Tobacco
Wear Protective Footwear
How long can Achilles tendonitis last?
The healing process of a tendon can be hampered by early exercise, and Achilles tendinitis typically takes 6 to 8 weeks to heal. Patients may experience severe frustration and a twofold increase in recovery time if they fail to comply. It is advised to seek early and vigorous conservative therapy in order to stop more tendon damage.




2 Comments