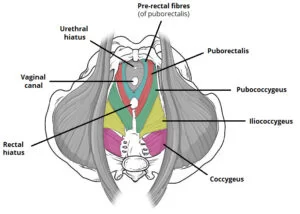
Pelvic Floor Muscles
What is a Pelvic Floor Muscles?
The pelvic floor muscles are a crucial group of muscles located at the base of the pelvis, forming a supportive hammock-like structure that plays a vital role in various bodily functions.
Comprising layers of muscle fibers, ligaments, and connective tissues, the pelvic floor provides essential support for the pelvic organs, including the bladder, uterus (in females), and rectum.
Introduction
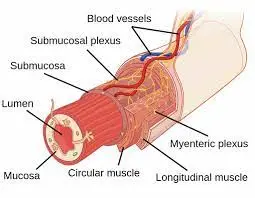
The pelvic cavity, referred to as the true pelvis, is home to the pelvic viscera, involving the bladder, rectum, pelvic genital organs, and terminal part of the urethra. This cavity is located beneath the pelvic brim in the lesser part of the pelvis.
The obturator internus and the piriformis muscle, which also forms the posterior wall, are two of the muscles that contribute to the shape of the cavity’s walls. We will discuss the structure of the pelvic floor muscles, which make the cavity’s inferior lining, in this section. Another name for the pelvic floor is the pelvic diaphragm.
We will examine the distinct functions of these muscles, their blood supply and innervation, and any potential clinical associations.
Your pelvic floor muscles support important physiological processes like urinating, defecating, and engaging in sexual activity while also improving your core. Incontinence and pelvic organ prolapse are two different conditions that may occur from their gradual weakening from injury and even aging. You may inhibit the negative effects of weak pelvic floor muscles by exercising your pelvic floor muscles.
What are the structures of pelvic floor muscles?
The anatomy of the pelvic floor looks like a funnel. It connects to the walls of the smaller pelvis, dividing the inferior perineum—which contains the genitalia and anus—from the pelvic cavity.
There are a few gaps in the pelvic floor to allow urination and defecation. There are two “holes” with important benefits:
- Urogenital hiatus – a hole that is located anteriorly that permits the urethra (and the vagina in females) to pass through.
- Rectal hiatus – a central opening that permits the anal canal to pass through.
The fibrous node known as the perineal body, which relates the pelvic floor to the perineum (explained further here), is located between the urogenital hiatus and the anal canal.
What are the pelvic floor muscles?
You may control the release of pee (wee), feces (poo), and wind (windus) and postpone emptying until a time that is convenient by using the pelvic floor muscles.
The pelvic floor muscles tighten the urethral, vaginal, and anus openings as well as increase the pelvic internal organs when you contract them. Pelvic floor relaxation improves feces and urine flow.
This function is particularly important if you have abnormal function of your urethral or anal sphincter muscles, which may happen after giving birth or after prostate surgery.
For both men and women, the muscles of the pelvic floor are necessary for sexual function. They are essential for the erection and ejaculation processes in men. Sexual sensation and arousal in women are affected by voluntary pelvic floor contractions or squeezing.
Women’s pelvic floor muscles must be relaxed during childbirth because they support the developing fetus during pregnancy.
The muscles and connective tissues that support the essential organs in your pelvis, such as your bladder, bowel (large intestine), and internal reproductive organs, make up your pelvic floor. Your pelvic floor muscles give flexibility to help with sex, urination, and other bodily functions while also supporting the position of these organs.
Your pelvic floor muscles, along with other essential torso muscles, help your body absorb external pressure (from coughing, lifting, etc.) in a way that protects your organs and spine. Additionally, these muscles help in the regulation of your bowel and bladder movements (continence).
What are the functions of pelvic floor muscles?
These muscles are essential to the proper functioning of the abdominal and pelvic viscera because they form the floor of the pelvic cavity.
The pelvic floor muscles play the following roles:
- Abdominopelvic viscera support: using tonic contraction.
- Resistance to intra-pelvic/abdominal pressure: rises brought on by actions like coughing or moving large, heavy objects.
- Urinary and fecal continence: On the rectum and urethra, the muscle fibers act as sphincters. To promote urination and defecation, they relax.
Muscles
It is important to keep in mind the funnel-shaped structure of the pelvic floor when understanding its muscles. The pelvic floor includes three main parts:
- Levator ani muscles (largest component).
- Coccygeus muscle.
- Fascia coverings of the muscles.
We will now take more detail at each of these parts.
Levator Ani Muscles
The levator ani is a big muscle sheet. Pubococcygeus, Puborectalis, and Iliococcygeus are the three separate paired muscles that make up this structure.
Puborectalis
The puborectalis is the most essential member of the levator ani group for maintaining fecal continence.
- Attachments: originates on the pubic posterior surface. It joins to the pubis on the opposite side of the anal canal, creating a U-shaped sling.
- Actions: The anterior anal canal is bent during tonic contraction.This results in forming the anorectal angle, which helps fecal continence. Defecation is voluntary inhibition of it.
- Innervation: Pudendal nerve and levator ani nerve.
In the male, the urethra and vagina, and in the female, the urethra and some pre-rectal muscle fibers form another U-shaped sling. These fibers play an important part in maintaining urinary continence, particularly when there is a sudden rise in intra-abdominal pressure, as occurs when sneezing.
Pubococcygeus
The majority of the levator ani complex is composed of the pubococcygeus. It is located in the pelvic floor, in between the iliococcygeus and the puborectalis.
- Attachments: originates on the pubic posterior surface. It blends with the pelvic floor’s contralateral muscle in the midline.
- Actions: The organs in the abdomen and pelvis are stable and supported.
- Innervation: Pudendal nerve branches and the nerve to the levator ani.
The posterolateral portion of the levator ani muscle group is made up of the slender iliococcygeus muscle.
- Attachments: originates from the internal obturator fascia’s posterior tendinous arch and ischial spines. It inserts onto the anococcygeal ligament, perineal body, and coccyx. It blends with the contralateral muscle fibers in the pelvic floor’s midline.
- Actions: the anorectal canal and pelvic floor are elevated.
- Innervation: branches of the pudendal nerve and the nerve to the levator ani.
Coccygeus
A small triangular muscle, the coccygeus is located behind the levator ani muscle group.
- Attachments: starts at the ischial spines and ends at the inferior end of the sacrum and coccyx.
- Actions: supports and flexes the coccyx and pelvic viscera.
- Innervation: Anterior Rami of S4 and S5.
- Blood supply: Pudendal, inferior gluteal, and inferior vesical arteries.
What do pelvic floor muscles do?
The main organs in your pelvis are protected and kept in place by the muscles of your pelvic floor. The ability to contract and relax your pelvic floor muscles is known as muscle control, and it aids in the removal of waste from your body. Organs like your urethra, which is a tube that exits your body, and your anus, which is an organ where stools pass, are coordinated with the muscles of your pelvic floor. Your pelvic muscles can be contracted to make these openings smaller, which keeps waste from leaving. The pathways become wider when these muscles relax, allowing you to urinate or waste.
Having strong pelvic floor muscles helps you to automatically contract and release. Similar to flexing a bicep, you can also actively control these muscles.
Your pelvic floor muscles function differently according to your reproductive system. Depending on whether you are assigned male (AMAB) or female (AFAB) at birth, your pelvic floor muscles perform differently. Cisgender women, some transgender men, and nonbinary people with vaginas are regarded as people of the AFAB community. AMAB people include nonbinary people with penises, cisgender men, and some transgender women.
Pelvic floor muscles in AFAB people
Your pelvic floor muscles:
- Provide support to your uterus, large intestine, rectum, bladder, urethra, and vagina.
- To maintain control over when you pass urine, defecate, or pass gas, squeeze and relax.
- To promote vaginal contractions and blood flow during orgasm and sex.
- Promote women to provide birth vaginally.
Pelvic floor muscles in AMAB people
Your pelvic floor muscles:
- Give support to your rectum, anus, large intestine, bladder, urethra, and prostate.
- To have control over when you pee, defecate, or pass gas, squeeze and relax.
- Support you in ejaculating and keeping an erection during sexual activity.
Where are your pelvic floor muscles located?
The basis of your core is formed up of the muscles in your pelvic floor. Your core muscles involve your pelvic floor muscles, abdominal muscles, back muscles, and diaphragm (the muscle that controls breathing). These muscles work together to support the center of your body by connecting to your pelvis and spine.
Your pubic bone in the front of your body and your tailbone (coccyx) in the back are the locations of your pelvic floor muscles. On the left and right sides of your pelvis, the muscles on the ischial tuberosity, or sitting bones, extend outward. A single-minded layer of layered muscle with anus, urethra, and vaginal openings is formed by the cooperation of several pelvic floor muscles.
Take squeezing these three openings to feel where your pelvic floor muscles are located.
- Vaginal opening: Try to squeeze your vagina by inserting one or two fingers inside.
- Urethra: Squeeze as if you were preventing the flow while picturing yourself urinating.
- Anus: As though you were trying to stop yourself from breaking wind, squeeze your anus.
You should feel a pull inward and upward from the muscles inside your pelvis in each scenario. Your pelvic floor muscles are these.
What are the main pelvic floor muscles?
Layers of muscles and the connective tissues (ligaments) that join them form your pelvic floor. Your pelvic floor muscles are formed up of two main muscles that combine:
- Levator ani: The majority of your pelvic floor muscles are made up of the levator ani, which is divided into three different muscle groups: the puborectalis, iliococcygeus, and pubococcygeus: Your pelvis is fully encircled by the levator ani.
- Coccygeus: The smaller muscle in your pelvic floor is called the coccygeus. It is situated in the rear of your pelvis.
Which common diseases and disorders are related to the pelvic floor muscles?
Weakened or extremely relaxed pelvic floor muscles can lead to a variety of pelvic floor disorders. However, overly tight muscles can also lead to issues. Balance is the aim.
Although they should be flexible enough to allow for stretching and relaxation, your pelvic floor muscles should be strong enough to support your organs and stabilize your core.
Weak (too loose) pelvic floor muscles
Trauma or injury, such as childbirth or surgery, can cause the pelvic floor muscles to weaken. During pregnancy or from overuse (frequent heavy lifting, persistent coughing, constipation), they may experience stress. As they age naturally, they may become weaker as a result of hormone changes that happen during menopause. Diabetes and other diseases may also contribute to the weakening of the pelvic floor muscles.
Weak pelvic floor muscles may bring on the following disorders:
- Stress incontinence: When you cough, sneeze, laugh, or lift something, you might pee or drip. It happens more frequently after giving birth, after prostate surgery, or when there has been a pelvic injury.
- Urge incontinence: unable to resist the constant need to urinate.
- Fecal incontinence: Having difficulty controlling bowel movements.
- Anal incontinence: Having difficulty keeping your gas under control.
- Pelvic organ prolapse: Your uterus, rectum, and bladder are examples of unsupported pelvic organs that can protrude from the opening of your vagina or bulge into it. After menopause, this condition is most common in AFAB humans, such as cisgender women.
Having weak pelvic floor muscles can cause symptoms like incontinence, which is the inability to control when you urinate, poop, or pass gas.
Some causes of weak pelvic floor muscles include:
- surgery for bowel or bladder issues.
- constipation.
- being overweight.
- repeated heavy lifting.
- high-impact workout.
- chronic coughing that doesn’t go away (such as smokers cough, bronchitis, or asthma).
- aging.
Exercise for the pelvic floor muscles can almost always strengthen weak pelvic floor muscles.
Too tight pelvic muscles
The conditions related to hypertrophic pelvic floor, or excessively tight pelvic muscles, are less well understood. However, having too little give in your pelvic muscles can cause pelvic pain, back, hip, and leg pain, difficulty urinating, constipation, and increased frequency or urgency of urination.
Stress, childbirth, other gynecologic conditions, trauma or accidents of any kind, and overly taut pelvic muscles are all potential reasons for this problem.
When the muscles in the pelvic floor become tense and unable to relax, the result is a hypertonic pelvic floor. Pelvic pain, painful sex, constipation, and urgency are common symptoms of a tense pelvic floor.
To manage or treat your hypertonic pelvic floor, consult a women’s, men’s, or pelvic health physiotherapist.
Which conditions involving weak pelvic floor muscles are treated commonly?
To strengthen the muscles in the pelvic floor, people frequently perform exercises known as Kegels. The Kegel exercises require you to regularly contract and relax your pelvic muscles to gradually gain control.
Another approach to treat incontinence is with kegel exercises. When you train your muscles with Kegel exercises, your provider may use biofeedback. Biofeedback occurs by using a sensor in your vagina to identify the muscles you squeeze and the force with which you squeeze.
You should seek help from your provider before attempting Kegel exercises, depending on your medical condition. As an example, if you have recently strained or injured your pelvic floor muscles (for example, during childbirth), you should not attempt Kegel exercises.
Other treatments involve:
- Managing constipation: Many different ways of treating constipation (diet, exercise, drugs, etc.) can help you avoid straining your pelvic floor muscles when using the restroom.
- Vaginal weights/Kegel balls: You can gradually strengthen your pelvic floor muscles by placing specially designed balls into your vagina and holding them there. At the same time, you go about your regular daily activities.
- Medical devices: If your pelvic floor muscles are insufficiently strong to support your pelvic organs, devices such as a vaginal pessary can hold them in place.
- Physical therapy: You can improve the coordination and strength of important core muscle groups, including your pelvic floor muscles, with the assistance of a qualified physical therapist who specializes in treating pelvic floor disorders.
- Surgery: Reconstructive surgery or obliterative procedures such as colpocleisis may be essential to secure your pelvic organs into place if you have pelvic organ prolapse. The condition known as colpocleisis causes the walls of your vagina to close together, preventing organs from protruding outside of it.
What common therapies are used to treat hypertonicity or abnormally tight pelvic floor muscles?
For pelvic floor hypertonicity, treatments involve physical therapy, breathing/relaxation techniques, injections into your pelvic floor muscles, medications, and cognitive behavioral therapy.
What small lifestyle adjustments can you make to maintain the health of your pelvic floor muscles?
You can strengthen your pelvic floor muscles by performing Kegel exercises regularly, depending on your health. The benefits involve improved muscle control to help with continence and raise sexual function. In the past, Kegel exercises were generally associated with an increase in vaginal sex satisfaction. The benefits of sex may be universal, irrespective of gender, according to recent research.
When performing Kegel exercises, you must be working the right muscles. To make sure you’re exercising the appropriate muscles and contracting/properly releasing them, pay attention to the advice of a doctor or a physical therapist.
You can work on your pelvic floor muscles in a seated, standing, or lying down position.
- Make sure not to squeeze your legs, butt, or any other muscle as you squeeze the pelvic floor muscles for eight seconds. As you squeeze, make a conscious effort to breathe freely.
- Take eight seconds to relax your pelvic floor muscles. Kegel exercises are as much about relaxing as they are about squeezing. Breathe freely as before.
- Squeeze for eight seconds, then release the pressure for eight more, repeating this sequence eight times.
Three times a day, repeat this exercise. Work out your Kegels at times when you’re most likely to incorporate them into a routine you’ve already created, like in the morning while you brush your teeth, during lunch when you check social media, in the evening when you drive home from work, etc.
Instead of eight seconds, you may need to start out aiming for three seconds of squeezing and relaxing. As you get better, you could extend your relaxation and squeezing time from eight to twelve seconds. To prevent overstretching your muscles, start slowly and increase your time gradually.
Your pelvic floor muscles should become stronger in four to six months.
Pelvic floor muscle exercises
The advantages of Kegel exercises, or exercises at the pelvic floor muscles.
Similar to other body muscles, the pelvic floor muscles become stronger with regular exercise.
- Exercises affecting the muscles of the pelvic floor can help men who have stress incontinence (men who urinate when they cough, sneeze, or are active).
- Men who tolerate frequent, urgent urges to urinate may find that pelvic floor muscle exercise is helpful as well (called urge incontinence).
- Exercises focusing on the muscles of the pelvic floor may help men who struggle with bowel control by strengthening the muscle that closes the anus (back passage). One of the pelvic floor muscles is this one.
To help them become stronger and function better, it is recommended that you exercise your pelvic floor every day.
Finding the right muscles
You must first determine which muscles need to be trained before starting pelvic floor muscle training. There are various ways you can do this:
- Try to slow or stop the flow of pee when you go to the bathroom halfway through emptying your bladder. You are working the right muscles if you can do this. Try this technique just once a week. Your bladder cannot empty as it should if you do this too frequently.
- Relax the muscles in your buttocks, stomach, and thighs when you sit or lie down.
- As though trying to halt the passage of wind, squeeze the ring of muscle around the anus (back passage).
- Now enable this muscle to relax. Until you are certain that you have located the right muscles, squeeze and release a few times.
- Try to avoid squeezing your posterior.
- Remove your clothes and stand in front of the mirror. Properly pull and hold your pelvic floor muscles in place. Your scrotum should lift and the penis should draw in.
How to do pelvic floor muscle exercise
You can start exercising your pelvic floor muscles as soon as you can feel them contracting:
- It is possible to perform exercises for the pelvic floor muscles anywhere—while sitting, standing, or lying down.
- Squeeze and tighten the muscles surrounding your back passage, or anus. Raise them up and inside. Each time you squeeze your pelvic floor muscles, you should feel a “lift.”As you count, try to hold them tightly and firmly. Let them go now, and relax. You should experience a clear sense of “letting go.”
- Just hold for as long as you can if you are unable to hold for eight.
- “Squeeze and lift” once more, then release. The best period to relax is eight seconds or so between muscle lifts.
- You should try to squeeze and lift as many times as you can, no more than eight or ten times. One set is equal to this.
- Aim for three sets of eight to ten squeezes every day.
When performing pelvic floor muscle training:
- keep breathing.
- Only squeeze and lift.
- Do not tighten your buttocks.
- keep a relaxed thigh.
The best results from pelvic floor exercises are achieved through individualized programming and close supervision. See your physician (GP), a women’s, men’s, or pelvic health physiotherapist, or a nurse continence specialist for help if you are unsure that you are performing the squeezes correctly or if your symptoms have not improved after three months.
The exercises given below should be performed three times a day. They are almost always possible to perform anywhere.
Techniques
Your pelvic floor muscles can be situated in a few different ways. Women will feel a slight pulling in the vagina and rectum when using the pelvic floor muscles. Men will experience a pulling-in of the anus and movement of the penis. Each person is different, different approaches will work for them.
General Technique
Envision yourself in a crowded room, feeling required to pass gas or “wind.” To stop ourselves from passing gas, most of us will clench our rectum and anus muscles (back passage). You contract your pelvic floor muscles. You are using the right muscles if you experience a “pulling” feeling at the anus. This is the most effective method for the majority of patients.
Technique for Women
Laying down, reach a finger inside your vagina. Squeeze the muscles in your vagina around your finger. The pressure on your finger may also be felt, in addition to the sensation that should be felt in your vagina. By feeling this, you are activating the correct muscles. Use two fingers to feel for movement if you can’t with just one.
Technique for Men
Watch your penis as you stand in front of the mirror. Without moving the rest of your body, attempt to raise and lower your penis. You are using the correct muscles if you can perform this.
Your pelvic floor muscles might not come to mind right away. It needs a lot of people to take their time.
Don’t Exercise the Wrong Muscles
The most frequent error is to exercise the incorrect muscle or muscles. Most people tighten other muscles in a move to find a new muscle, especially a weak one. Some might hold their breath, clench their teeth or fists, or make an expression. This is useless. It is very tempting to use stronger muscles to support weaker muscles, like the pelvic floor muscles, because they are smaller. However, learning how to use the correct muscles is hampered by using other muscles. It is best to just focus on your pelvic floor muscles and try to relax your body as much as possible.
Not Your Abdominal Muscles
Squeeze your pelvic floor muscles while keeping your hand lightly on your belly to prevent using your stomach muscles. Relax and try again if you do. Make sure that there is no movement in your stomach.
Not Your Chest Muscles
Your chest muscles are most likely being used if you find yourself holding your breath. To prevent this, relax fully and take a moment to become aware of your breathing. Hold the contraction of your pelvic floor muscles while maintaining a regular breathing pattern. Keeping your chest muscles relaxed during breathing can help ensure that you are not using them.
Not Your Buttock Muscles
The muscles in the buttocks are the other group of “wrong muscles”.Squeeze your pelvic floor muscles while seated in front of a mirror to see if you are casually tightening your buttock muscles. You are also using your buttock muscles if you find that your body is making a slight up-and-down movement.
Not Your Thigh Muscles
It is also not advised to use the thigh muscles. You are using the wrong muscles when you sit and notice that your upper legs are moving and your entire body is lifting. No one else should be able to tell that you are squeezing your pelvic floor muscles if you perform this technique correctly.
Reasons
You can begin your daily exercise routine once you can locate your pelvic floor muscles and squeeze them without using your other, stronger muscles.
For two reasons, you should work out every day:
- Your pelvic floor muscles become stronger through exercise, making them capable of stopping urine leaks.
- You become able to control these muscles with continued practice. After that, you can use them right away to stop pee loss or lessen the urge to urinate.
You will squeeze your muscles for five seconds when each exercise, and then you will relax them for five seconds. Most people frequently don’t give themselves enough time to relax in between squeezes. Between squeezes, you have to give the muscles time to relax so they can rest before you squeeze again.
Applying Pelvic Muscle Tone to Control the “Urge”
It’s a common misconception that emptying the bladder is the only way to get rid of the uneasy, sudden sense of urgency. You don’t have to go potty when an urge strikes. All urges are alerts that tell you to urinate at some point. The urges to go are frequently “false” signals if you have an overactive bladder. However, urges shouldn’t be used as orders. They need to act as an early warning system, preparing you to locate a restroom once you’ve calmed down and repressed the urge.
Your pelvic floor muscles will be used to reduce or eliminate the urge to urinate. When the urge strikes, you will need to rapidly contract your pelvic floor muscles several times. Squeeze and relax the pelvic muscles as quickly as you can to achieve this. Keep your muscles taut between squeezes. Now try this.
In this way, you can instruct your nervous system to stop your bladder from contracting by squeezing your pelvic floor muscles. The urge will fade as your bladder starts to relax and stop contracting. There’s a safe window of time when the bladder is calm after the urge to urinate passes. The optimal time to use the restroom is during this “calm period”.
These Exercises Cannot Harm You
These workouts don’t cause any harm. They should be simple and relaxing for you. You are probably trying too hard and using your stomach muscles if you exercise and then get back pain or stomach pain. You are tensing your chest muscles and most likely holding your breath if you have headaches. It is not advised to perform these exercises while urinating by alternating the flow of urine.
Routines
You should alternate between squeezing and relaxing your pelvic floor muscles to strengthen them. To help, take the actions listed below.
- Give your muscles a quick squeeze, then hold it.
- Take a two-second break from your muscles.
- Every time you squeeze and release tension, one set is completed.
- Complete all five sets.
How can I strengthen my pelvic floor muscle?
Pelvic floor muscles can be trained and strengthened with consistent, focused exercise, just like any other muscle in the body.
It is practically always possible to regain control over the pelvic floor muscles and show them how to perform their functions properly.
Pelvic floor muscle exercises can support with:
- increase bladder and bowel control.
- decreasing the risk of prolapse (in women).
- help recovery after childbirth and surgery (in women).
- help recovery after prostate surgery (in men).
- raise sexual sensation.
- raise social confidence and quality of life.
The first thing you need to do is find out which muscles you necessary to train. Before starting a regular pelvic floor muscle exercise program, it is important to identify your pelvic floor muscles correctly. A pelvic floor physical therapist can help with this and ensure you use these muscles properly.
Once you are comfortable performing the exercises, up the number to ten times a day. As it becomes easier, try squeezing and holding your muscles for three seconds, followed by three seconds of relaxation. With increased strength in your pelvic muscles, you can advance to longer squeezes lasting roughly 10 seconds. It’s important to let your muscles rest in between squeezes so that you can squeeze again.
Keep in mind that every squeeze and release constitutes a single, full set. Perform the following three sets of exercises each day: ten in a seated, ten in a standing position. It makes no difference when in the day it is. You must make it a habit to complete the exercises each day.
You will initially need to schedule some time to focus on the exercises. Find a cue, or a habitual activity, that will serve as a reminder to practice. For instance, it could be a good idea to work out right before bed and before you go to sleep.
Sample Exercise Schedule
Try these exercises:
- Squeeze for 5 seconds while lying down, then relax for 5 more. Repeat this technique 10 times.
- Squeeze for five seconds while seated, then let go for five more. Repeat ten times.
- As you stand up, squeeze for five seconds, then let go for five more. Repeat this process ten times.
Squeeze and count slowly, “1 and 2 and 3 and 4 and 5,” then let your muscles relax for five seconds while you continue to count. You can squeeze for an extra ten seconds or so once you can perform the exercises with ease. Repeat twice a day for thirty full sets.
After starting the exercises, pelvic floor muscle support usually improves in six weeks. There should be noticeable improvements after three months. It’s important to monitor your progress over time, as symptoms might not improve right away.
Making These Exercises Part of Your Life
Incorporate the exercises into your everyday routine to help them become routine to you. Do your workouts while going about your regular workplace. After practicing the exercises for six weeks, you won’t need to set aside specific times to focus on them because they will become easier to perform.
For instance, tense your muscles when you walk, before you cough, when you stand up, and when you’re on your way to the restroom. When you feel a strong urge that you can’t resist, try tensing up the muscle. All it needs is practice.
Perform your workouts at:
- brushing your teeth when standing at the sink.
- awakening in the morning.
- washing dishes.
- putting on your makeup.
- sitting in the car at a stoplight.
- sitting and having dinner.
- reading a book in bed.
- watching TV – during each commercial.
- going for a walk.
- talking on the phone.
- having sex.
It’s not required to maintain an official tally of how many times you complete each exercise. Simply repeat the process multiple times. Perform in them frequently enough to form a habit.
Clinical significance
Pelvic Floor Dysfunction
A variety of indicators and symptoms connected to improper pelvic floor muscle function are collectively referred to as pelvic floor dysfunction.
The urethra, vagina, and anal canal have support in women by the pelvic floor muscles. A loss of structural support for these organs may arise from the weakening of these muscles and present as:
- Urinary incontinence.
- Fecal incontinence.
- Genitourinary prolapse.
- Pelvic pain.
- Sexual dysfunction.
The causes of pelvic floor dysfunction are understood to be multifactorial and involve obstetric trauma, raised age, obesity, and chronic straining.
Clinically significant alterations to the pelvic floor can lead to the following outcomes:
Anterior vaginal wall prolapse
- Cystocele (bladder into vagina).
- Urethrocele (urethra into vagina).
- Cystourethrocele (both bladder and urethra).
Posterior vaginal wall prolapse
- Enterocele (small intestine into the vagina).
- Rectocele (rectum into the vagina).
Apical vaginal prolapse
- Uterine prolapse (uterus into vagina).
- Vaginal vault prolapse, or vaginal roof, following a hysterectomy.
Gynecological cancer treatment may lead to pelvic floor dysfunction.
In addition to causing urine incontinence, pelvic floor damage can result in the prolapse of pelvic organs. When a woman’s pelvic organs—such as her vagina, bladder, rectum, or uterus—protrude into or above her vagina, it is known as pelvic organ prolapse. Urinary incontinence is also caused by many of the same factors that cause pelvic organ prolapse.
These include unusual (asymmetrical, excessive, or insufficient) muscle tone and pelvic trauma-related asymmetries. Pelvic organ prolapse is affected by several factors, including age, pregnancy, family history, and hormonal state.
The vagina is supported by attachments formed by smooth muscle, collagen, and elastin that are attached to the sacrum, pelvic side wall, and perineum. Pelvic floor muscle repair is a surgical procedure. The pelvic floor muscles can be strengthened using kegel exercises.
Rectal prolapse, rectocele, perineal hernia, and several functional disorders, such as anismus, are examples of disorders affecting the posterior pelvic floor. Any of these disorders may cause constipation, which is known as “functional constipation” and can be determined using clinical diagnostic criteria.
Exercises known as Kegel exercises, or pelvic floor exercises (PFE) can assist the pelvic floor muscles to become more toned and functional. This is especially beneficial for women (and less frequently, men) who have stress urinary incontinence. PFE is generally ineffective for urinary incontinence unless used under trained supervision and with biofeedback; in severe cases, however, it may not be helpful.
Moreover, there is frequently low compliance with PFE programs. A perineometer, which gauges the vaginal pressure, can be used to estimate the tone of the pelvic floor muscles. Moreover, medication can be used to enhance continence. Surgery may be necessary in extreme situations to reconstruct or even repair the pelvic floor.
A specialty focusing on problems with the three axes (urological, gynecological, and coloproctological) of the pelvic floor is called perineology, or pelviperineology.
Summary
The muscles of the pelvic floor provide the uterus, bowel, and bladder. The uterus, colon, and bladder are all provided by the pelvic floor muscles. They are essential for maintaining sexual function as well as preventing prolapse and bladder and bowel incontinence.
Pregnancy, childbirth, prostate cancer treatment, obesity, and the strain of long-term constipation can all weaken the pelvic floor. Changes in the pelvic floor muscles may occur from pregnancy, childbirth, obesity, long-term constipation, or surgery for prostate cancer. These changes can cause problems.
Your pelvic floor muscles may not be strong or quick enough to work well for you, and you might have difficulties with your bladder, bowel, or sexual function as a result.
The goal of pelvic floor exercises is to improve muscle strength. Should your pelvic floor muscles be overworked or overactive, you might have difficulties with them. Flexible muscles are strong muscles. This could affect men who suffer from chronic prostatitis or pelvic pain, women who have not given birth, and women who experience painful periods.
All genders have pain during sexual activity, when peeing, or when having bowel pain as additional issues related to having a weak but overactive pelvic floor. Although common, pelvic pain is abnormal and treatable.
FAQs
How do I strengthen my pelvic floor?
Squeeze your pelvic floor muscles as much as ten times when standing, sitting, or lying down to strengthen them. Avoid holding your breath or contracting your thigh, butt, or abdominal muscles at the same moment. Once you become comfortable performing pelvic floor exercises, you should try holding each squeeze for a little moment.
What causes tight pelvic floor muscles?
Pelvic infection: The stressed tissue will contract and bulge if you have an infection. Emotional or mental factors: Traumas or traumatic experiences in the past may cause you to contract your pelvic floor. Muscle tensing behaviors may occur from everyday stress. Muscles that are constantly contracted might become painful.
What are the abdominal and pelvic floor muscles?
The structure of the muscular group known as the “core” is formed up of the pelvic floor muscles. These muscles support the spine and maintain the pressure inside the abdomen by connecting with the diaphragm, the breathing muscle, and the deep abdominal (tummy) and back muscles. The internal pressure in the abdomen rises with physical activity.
How do you fix a weak pelvic floor?
Exercise 2: Lie and tighten
Knees bowed, feet flat on the floor, you should lie on your back.
For a count of five or for as long as it feels comfortable, tighten your pelvic floor muscles and squeeze, raise, and hold.
Let go and count to five gently.
Attempt to perform the pelvic floor exercises thrice daily.
Can a weak pelvic floor be cured?
Since most cases of pelvic floor dysfunction can be resolved with medication, physical therapy, and biofeedback. Get medical care if you start showing any of the signs of pelvic floor dysfunction.
How can I determine whether my pelvic floor is weak or tight?
Symptoms of pelvic floor dysfunction often include:
sneezing, laughing, coughing, or exercising and unintentionally releasing pee.
being rushed and running out of time to use the loo.
having to go to the toilet constantly.
having difficulty passing gas or urine.
How can I determine whether my pelvic floor is tight?
Pelvic floor tension myalgia
Pain that goes away when the body is repositioned or that gets more difficult with specific movements.
Pain experienced during a sexual encounter.
having trouble urinating.
uncomfortable or often occurring urination.
Urinary incontinence.
Stool passage is difficult.
Bloating and constipation.
Lower back pain.
What signs of a tight pelvic floor are present?
Constipation, uncomfortable sex, urgency, and pelvic discomfort are among the pelvic problems that many people with a stiff and non-relaxing pelvic floor face. The piriformis, obturator internus, coccygeus, and hamstrings belong to the surrounding hip and pelvic muscles that may tense up in response to a hypertonic pelvic floor.
What are the 4 pelvic floor muscles?
The muscles of the pubococcygeus, ileococcygeus, coccygeus, and puborectalis make up the deep pelvic floor.
Is walking good for the pelvic floor?
Weak muscles can be strengthened and recovered to optimal function with consistent, progressive exercise. You can strengthen your pelvic floor muscles by engaging in regular, mild activities like walking.
Can I fix my pelvic floor at home?
Strengthen your core.
The purpose of Arnold Kegel’s 1940s design was focused on the pelvic floor region. The pelvic floor muscles are strengthened in cooperation with the core muscles. Strengthening the entire pelvic floor can be accomplished by exercises like yoga and Pilates.
Do squats strengthen the pelvic floor?
Squats assist with developing a stronger pelvic floor and buttocks in addition to the bridge. Maintaining flat feet on the ground, position yourself with your feet hip-width apart. Bring the buttocks as near to the floor as comfortable by bending at the knees.
What medication is used for the weak pelvic floor?
Urinary incontinence can be treated with once-daily oral antimuscarinic medicines. Solifenacin, fesoterodine, trospium, tolterodine, darifenacin, and oxybutynin are a few examples.
Why did my pelvic floor get weak?
Pregnancy, childbirth, prostate cancer therapy, obesity, and the pressure of long-term constipation can all impair the pelvic floor. Obesity,
delivery, prolonged constipation, pregnancy, and prostate cancer surgery can all result in alterations to the muscles that make up the pelvic floor, which can cause problems.
How long does it take to make the pelvic floor stronger?
It’s unlikely that you’ll see any results for a few weeks, so persevere! It will take at least three months of consistent workouts before your muscles reach their maximum strength. Make the practice of exercising while going about your daily business.
Can a tight pelvic floor go away on its own?
Make a consult with your general practitioner (GP) if you suffer from pelvic pain, problems urinating, difficulty during bowel movements, or discomfort during sex. Contacting a physician is advised as these symptoms frequently do not go away on their own.
Do weights strengthen the pelvic floor?
Many problems, such as pelvic organ prolapse and female urine incontinence (UI), may result from this. Paradoxically, weight-bearing exercises can strengthen the core and assist in preventing prolapse and UI when performed correctly. It’s crucial to finish the activities properly.
Is sitting bad for pelvic floor muscles?
The pelvic floor may get damaged as a result of prolonged sitting, although proper posture and regular rests can help. Whether your incontinence stems from injury to your pelvic floor or another underlying condition, Byram Healthcare may help you if you do experience it.
How many Kegels should I do per day?
Before you get out of bed in the morning and before every meal during the day, I advise finishing a set of 10 repetitions. Do this every day. Similar to other workouts, Kegels provide better effects the more frequently you perform them. Aim for 40 Kegels per day, which is four sets of 10 reps.
References
- TeachMeAnatomy: The Pelvic Floor: Structure, Function, and Muscles. (2023, January 19). TeachMeAnatomy. https://teachmeanatomy.info/pelvis/muscles/pelvic-floor/.
- Professional, C. C. M. (n.d.). Pelvic Floor Muscles. Cleveland Clinic. https://my.clevelandclinic.org/health/body/22729-pelvic-floor-muscles.
- A. (2022, August 3). Pelvic floor muscles. Continence Foundation of Australia. https://www.continence.org.au/about-continence/continence-health/pelvic-floor.
- The Pelvic Floor Muscles: Signs, Evaluation, and Management – Urology Care Foundation.. (n.d.). https://www.urologyhealth.org/urology-a-z/p/pelvic-floor-muscles.
- Pelvic floor. (2023, December 24). Wikipedia. https://en.wikipedia.org/wiki/Pelvic_floor.
- Pelvic floor. (n.d.). Better Health Channel. https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/pelvic-floor.


2 Comments