Periarthritis
What is Periarthritis?
Periarthritis, also known as calcific periarthritis, is a painful condition that occurs when calcium crystals construct around your joints or in the soft tissues and form a circle around the joint. This can make pain and swelling. The joints may also feel thick and stiffened, or “frozen.”Calcium crystals are naturally seen in your body. You require them to make strong teeth and bones.
However, an increased level of calcium crystals can build up around tendons and joints. The crystals can rub opposite to the tendons and muscles and lead to aches and swelling. This leads to periarthritis. This condition is most general in the shoulder joint, but it can affect your hips joints, hands, and other joints, as well.
Stages of Periarthritis
Stage #1 Freezing:
- Pain (sometimes severe) in the joint when you move joint
- The ache gets worse over time and hurts more at night
- Pain that lasts anywhere from 6 to 9 months
- Limitation in how away you can move your joint
Stage #2 Frozen:
- Ache can get better but stiffness gets worse
- Moving your joints gets harder and therefore activity becomes difficult
- Muscles around the joint may waste since they are not being used
- Stiffness that lasts 4 to 12 months
Stage #3 Thawing:
- Pain and stiffness gradually subside
- Range of motion starts to improve
- This takes about 6 months to 2 years
What are the symptoms of periarthritis?
The primary symptoms of periarthritis are pain (ache), swelling, and stiffness of the harmed joint. Symptoms can come on suddenly and might be severe in a few cases. Other symptoms might include:
- tenderness in the harmed joint
- pain that makes it difficult to move the harmed joint or limb
- pain that is worse when you move the harmed joint
- The ache that gets worse at night
- pain that makes it hard to sleep
- A decreased range of motion (motions of the joint causes stiffness or severe pain)
Causes and risk factors for periarthritis?
Periarthritis is a general condition. It’s the outcome of too much calcium in the body, and it can happen to anyone, specifically as your body ages. However, there are a few factors that expand your risk of periarthritis. These involve:
- living between the ages of 40 and 65 years old
- being a female
- having a hyperactive parathyroid gland or any other thyroid problem
- having health problems that affect your kidney function
- having diabetes
- having any heart health disorder
- having Parkinson’s disorder
- having had a stroke
- having had recent trauma to a joint or hyper using a joint
- having had a rotator cuff trauma
- having postsurgical scarring, particularly on your shoulders
- having taken certain drugs
- leading an inactive lifestyle
Diagnosis
A doctor will say to take several tests if they suspect that your ache and stiffness are caused by periarthritis. After a physical examination and exchange of your symptoms and medical record, you’ll likely have a series of tests, involving:
- imaging tests: Imaging tests such as X-rays and ultrasounds can assist doctors to look for calcium crystals surrounding your joint and tendon.
- blood work: Blood work can test for inflammation and for the quantity of calcium in your blood. It can also assist doctors to rule out other problems that could be causing your symptoms.
What are the treatment options for periarthritis?
Medication
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs can assist to decrease the ache and inflammation in your harmed joint. For mild aches, your doctor might suggest over-the-counter NSAIDs. If your ache is moderate or severe, your doctor might write you a prescription for harder NSAIDs.
- Needle aspiration: Periarthritis can cause swelling in the bursa in the middle of your joints. Aspiration is a method that uses a syringe to remove excess fluid from the bursa for instant relief of pain and swelling.
- steroid injections: Steroid injections can assist to decrease pain and swelling. Your doctor can insert the steroid drugs directly into the harmed area.
- surgery: Occasionally, surgery is done to separate very large calcium crystals that are causing severe aches or that are making motion difficult.
Physiotherapy treatment
General Mobilization Techniques
- Passive gliding with longitudinal traction
Take a supine position. Full abduction and neutral rotation with an elbow joint in 90-degree flexion done by the patient. The therapist put in longitudinal traction along the axis of the humerus. Glide in a slow rhythmic manner done by the therapist.
- Forward stooping glide
Fix the shoulder joint with one hand and another hold of the wrist joint then slow circumduction motion is carried out to limit ache.
Pendulum stretch
First, do this exercise. Relax your shoulders joints. Stand and lean over slightly, permitting the injured arm to hang down. Oscillate the arm in a small circle — about a foot in broadness. Perform 10 repetitions in each direction, you can do it once a day. As your symptoms enhance, enlarge the diameter of your swing, but never force it. When you’re ready for more, enlarge the stretch by holding a lightweight (3 to 5 pounds) in the swinging arm.

Towel stretch
Hold one end of a 3-foot-long towel at the back of your back and grasp the opposite end with another hand. Grasp the towel in a straight position. Use your good arm to drag the harmed arm upward to stretch it. You can also do a new version of this exercise with the towel covered over your good shoulder. Hold the bottom of the towel with the injured arm and drag it toward the lower back with the normal arm. Do this 10 to 20 times a day with rest.

Finger walk
Face-to-wall distance is three-quarters of an arm’s length away. Extend out and touch the wall at waist level with the fingertips of the injured arm. With your elbow joint slightly flex, slowly walk your fingers up the wall like a spider, until you’ve elevated your arm as away as you comfortably can. Your fingers should be doing the motion, not your shoulder muscles or accessory muscles. Slowly down the arm (with the assistance of the good arm, if necessary) and repeat it. Perform this exercise 10 to 20 times a day with the affected arm.
Cross-body reach
Sit or stand position. Use your better arm to raise your affected arm at the elbow joint, and bring it up and over your body, applying gentle pressure to stretch the shoulder joint. Hold the stretch for 15 to twenty seconds. Do this 10 to 20 times per day for both arms.

Armpit stretch
Using your normal arm, raise the affected arm onto a shelf about breast-high. Gently flex your knee joint, opening up the armpit. Deepen your knee flex slightly, delicately stretching the armpit, and after then straighten. With each knee flex, stretch a little more, but don’t force it. Do this 10 to 20 times each day bilaterally.
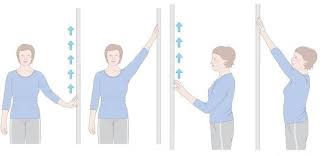
Finger ladder
ask the patient to stay standing (front and side) position and facing the ladder and moves the finger of the involved side shoulder upward along with the ladder to outstretch the highest limit of 10 repetitions 3 times a day
shoulder wheel
Instruct the patient to stand sideways on the shoulder wheel and clasp the holder and move the shoulder wheel clockwise and anticlockwise 10 counts 3 times a day
rope and pulley
Instruct the patient to stand or seat in the chair with back assistance then hold the handle of a pulley with both hands then move the acheful hand skyward side in form of shoulder flexion 10 repetitions 3 times a day
Shoulder abduction with theraband
Grasp one end of the theraband by the patient and other ends of the theraband put below the sole of the foot
Instruct the patient to grab theraband away from the body
come back to the starting position
Show shoulder abduction with theraband 2 to 3 times daily
10 repetitions each time
Shoulder adduction with theraband
Clasp one end of the theraband by the therapist or doctor and another end of the theraband by the patient
Instruct the patient to grab theraband outside away from the body
come back to the starting position
Perform shoulder adduction with theraband 2 to 3 times daily
10 repetitions each time
these exercises demonstrated by the therapist
stick shoulder flexion
seated, standing position
Grasp the stick upright in front of yourself
Bent forward onto the stick
feel some stretch while shoulder flexion
hold it for 30 seconds
3 sets 30-second with proper rest
3 to five times per week
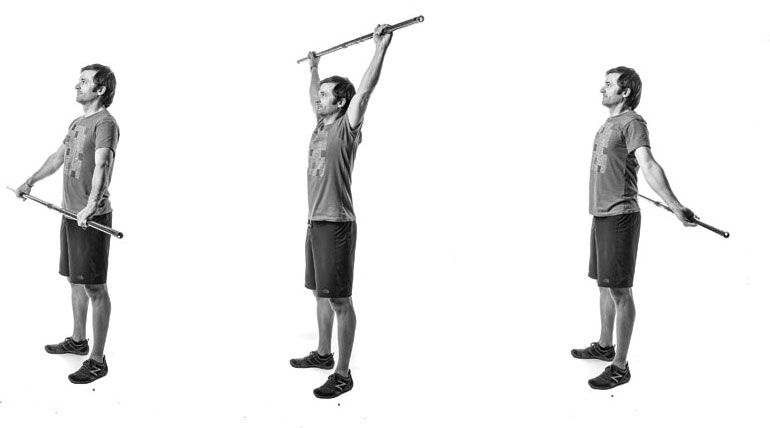
stick shoulder abduction
stand straight or supine position
Clasp the stick with the palm on the right-hand point far from the body, the left palm facing the body
keep your elbow joint straight and place it on your own site
use the left arm to thrust the right arm as high as it will go to the right side
slowly down the right and left arm, repeat for the opposite side, and switch the hand position such as left palm far from the body, right palm facing the body
10 to 15 times on both sides
3 sets with a rest
3 to five times per week
stick shoulder rotation
stand or supine position
Clasp the stick or towel with both hands, keep the elbow bent 90 degrees, and place it on the inward side
circumductory movement of the hands all the way clockwise, repeat the movement of the hands all the way to anti-clockwise (left side)
10 to 15 times on each side
3 sets
3 to 5 times per week
Stick overhead shoulder stretch
supine position
lies on the back with a stick held overhead
lower the hands overhead and feel the stretch
try to keep the back of the shoulder against the floor and core muscles tighten throughout the movement
hold for 5 to 10 seconds
raise your arm overhead and repeat
8 to 10 times
3 sets
3 to 5 times per week
stick shoulder extension
standing position
hold stick, broom, and cane behind the back and extend arm behind the back
keep shoulder blade squeezed together, and feel the stretch in chest muscle while avoiding pain and tension in the shoulder
hold for 30 seconds
3 sets with a 30-second break with each set
3 to 5 times per week
All exercises in the intermediate stage improve range of motion, stretching, mobility
Hip circles
This motion increases flexibility and stability. For more assistance, use a static object for support.
Stand on your right leg with your other leg lifted.
Shift your left leg in circles.
Do 20 circles in every direction.
Then do the opposite leg.
To make this exercise more hard, increase the diameter of the circles and do 2–3 sets.
Clamshell exercise
This exercise increase strength in your hips, thighs, and glutes. It fixes your pelvic muscles and can decrease tightness in your lower back, which assists to prevent hyper use and injury. Once you’ve easily done the basic pose, check out some variations.
Lie on your side in a side-lying position with flex knees and a resistance band surrounding your lower thighs.
Twist your top leg up as high as you can, then hold for a moment.
Down to the starting position.
Do 1–3 sets of 8–15 repetitions with rest.

Hip marching
This exercise increase strength and flexibility in your hips and thighs.
Sit toward the forward edge of a chair.
Lift your left leg as high as you can, keeping your knee flexed.
Slowly and with control, down your foot.
Then do the opposite side.
This is 1 repetition done by both legs.
Do 2–3 sets of 5–12 repetitions with rest.
Floor hip flexors
This movement stretches your hip flexors, thighs, and glutes.
Lie on your back or supine position and bring your right leg toward your chest.
Press the back of your opposite knee into the ground, sensing a stretch in your hip.
Hold this position for up to 30 seconds and put it down.
Do each side 2–3 times with rest.
Butterfly pose
This movement stretches your hips while enhancing blood circulation. Sitting position with rest your sitting bones on the edge of a cushion or folded blanket to assist the pelvic tilt. If you sense tight, put blocks or cushions under your thighs for assistance.
Sitting with your knees flexed and the soles of your foot jointly.
Clasp your fingers under your feet. Use your elbow joints to gently depress your knees down to the ground.
Since an opening in your hips as you release tension.
After 30 seconds, expand your arms in front of you and come into a further fold.
Hold this position for at least one minute.
You can increase the stretch by riching your heels closer to your body.

Knee-to-chest pose
This pose fixes your pelvis and stretches your hips.
Supine position with rest your head on a flat cushion or folded blanket for extra assistance. If you can’t bring your arms around your shins, place your hands around the backward side of your thighs.
For added ease, do the exercise with one leg at a time, and carry the other leg extended straight out or with a flexed knee.
Lie on your back in a supine position with your knees flex in toward your chest.
Fold your arms around your legs to take hold of your both hands, forearms, or elbows.
Smoothly tuck your chin into your chest to increase the length of the back of your neck.
Hold this position for thirty seconds and then relax.
Do this stretch 2–3 times with rest.

Side leg raises
This movement strengthens your glutes and thigh muscles. To increase trouble, put some weight on your thigh.
Lie on your right side in a side-lying position with your legs stacked.
Lift your left leg as up as you can.
Pause there, then return to the beginning position.
Do 2–3 sets of 12–15 repetitions on both sides with rest.

Thermotherapy
Deep heating modalities like Short Wave Diathermy (SWD), Long Wave Diathermy (LWD), etc. Using before passive mobilization for proper relaxation of muscle and ligament.
shockwave treatment: Shockwave treatment uses high-frequency shock waves to crack up calcium crystals that are causing serious symptoms.
How can you manage periarthritis at home?
You can also take steps at home to help decrease the ache of periarthritis. Lifestyle steps are a great way to handle your problem between appointments and decrease your symptoms. Your doctor might suggest lifestyle steps that are specific to the joint or junction your periarthritis effects and the severity of your symptoms. General lifestyle management steps involve:
Try to stop smoking: Smoking can raise inflammation in your body. When you quit, you can decrease inflammation and ache.
Apply ice: Ice packs are a simple way to reduce swelling and relieve pain. You can use ice throughout the day to help treat your periarthritis.
Rest: It’s important to get a better night’s sleep as your body heals and restores.
Exercise: Keeping your involved joint moving can assist to promote healing and prevent stiffness. Your doctor might suggest a few physical therapy sessions to assist you to learn exercises tailored to your periarthritis that you can do at home.
Manage your weight. Obesity is hard on your joints or junction. Achieving and maintaining a healthy weight can assist you to decrease pain.
Consider your diet. The quantity of calcium you eat or don’t eat, won’t impact periarthritis. However, there are foods that have been shown to decrease inflammation.
FAQ
Can periarthritis be cured?
Periarthritis isn’t a chronic disease. It will go away in about 2 to three years, even without taking any treatment. However, treatment can assist to manage acheful symptoms. And if symptoms are severe, certain medical treatments can assist resolve periarthritis very sooner.
How do you diagnose periarthritis?
There are many tests that can assist make a diagnosis of calcific periarthritis. X-rays or ultrasound scans can display any calcium crystals forming in a
tendon. Blood tests can measure inflammation in the body.
Is periarthritis the same as adhesive capsulitis?
One of the most general and acheful conditions of the shoulder is a frozen shoulder (adhesive capsulitis or periarthritis.) It can follow injury to the
shoulder joint, like dislocation or fracture, or a degenerative process. At times it can occur after an emotional injury or recovery from a long
illness.
What causes calcific periarthritis?
Calcific periarthritis is thought to be caused by the damage of a calcific accumulation into an adjacent soft tissue space or bursa along with the starting of an acute inflammatory reaction.
How do you treat calcific periarthritis?
As the clinical route of acute calcific periarthritis is self-limiting and typically sold out over the course of one month, the disease is effectively treated
via non-surgical treatment content including rest, icing, and non-steroidal anti-inflammatory medicines.