Phrenic Nerve
Introduction
The phrenic nerve plays a key part in breathing or respiration. It creates your diaphragm to contract and expand, providing your lungs capacity to inhale and exhale air. Nerve damage can create a paralyzed diaphragm. You may feel short of breath and carry problems sleeping. An irritated phrenic nerve can create persistent hiccups.
The phrenic nerve controls your diaphragm (the large dome-shaped muscle connecting your abdominal and chest cavities). It’s required to breathe. Your nerve gives signals that produce your diaphragm to contract (become thicker and flatter). This movement supplies your lungs room to develop and take in air (inhalation). After this, reduce firing of your phrenic nerve relaxes your diaphragm, and your lungs compress, moving out air (exhalation) and enhancing smaller.
Origin and course
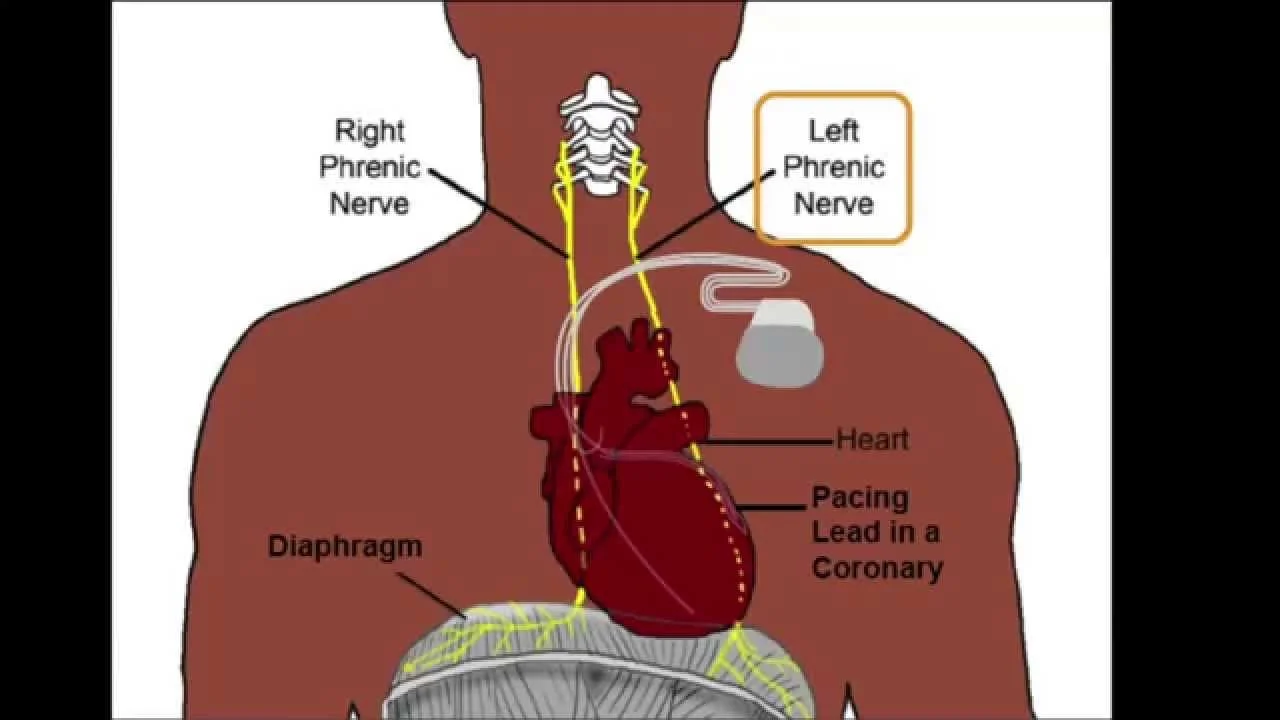
The diaphragm is innervated by the phrenic nerve, a bilateral cross-nerve that arises from cervical nerves in the neck and descends down the thorax.
It plays a crucial role in breathing by providing motor innervation to the diaphragm. The phrenic nerve’s anatomy varies, with left and right counterparts having different courses and relations.
It also resources sensory innervation to the central part of the diaphragm and attached fascial coverings.
The phrenic nerve is a deep branch of the cervical plexus that rise mostly from the C4 spinal nerve but also takes contributions from the C3 and C5 spinal nerves. This fact could be recalled by the mnemonic: C3, 4, 5, keep the diaphragm alive.
The phrenic nerve arises in the neck, at the upper lateral border of the scalenus anterior muscle, and declines across its anterior surface, deep to the prevertebral skin of the deep cervical fascia. The nerve connects to muscles, jugular veins, and arteries posteriorly.
From this point on, the route of the left and right phrenic nerves has several differences. However, on both sides, the nerves run after the subclavian vein enters the thoracic cavity via the superior opening.
The subclavian vein enters the thoracic cavity via the superior opening. The pericardiacophrenic arteries also guide both phrenic nerves across their course in the thorax.
Anatomy
The C3 to C5 cervical (neck) nerve source of your spinal cord is where your phrenic nerve attaches. The nerve:
- Starts at the C3 vertebral level, the part that coordinates with your jaw and helps you twist and rotate your neck.
- connects to the C4 and C5 levels of your neck vertebrae, which are below the C3 vertebra.
- A person who has a spinal cord injury between C3 and C5 may become paralyzed and unable to breathe on their own.
- Travels through your neck and chest (thorax) and past your heart and lungs to pass your diaphragm.
Anatomical Course
The phrenic nerve flow from cervical spinal roots C3, C4, and C5. This could be recalled apply the rhyme “C3, 4 and 5 have the diaphragm alive”. Spinal root C4 provides the main donation, with lesser purpose from C3 and C5 and some transmit fibers from the cervical plexus.
The nerve proceeds at the lateral border of the anterior scalene muscle. The cervical fascia’s prevertebral skin is subsequently reached by passing inferiorly over the anterior skin of the anterior scalene. The nerve travels posteriorly to the subclavian vein on both sides. From here, the natural phrenic nerve divide between the left and right:
Right Phrenic Nerve
- Passes anteriorly over the lateral portion of the right subclavian artery.
- Enters the thorax via the superior thoracic space.
- Descends anteriorly across the right lung root.
- The route along the pericardium of the right atrium of the heart.
- Pick the diaphragm at the inferior vena cava opening.
- Innervates the inferior skin of the diaphragm.
Left Phrenic Nerve
- Passes anteriorly over the medial portion of the left subclavian artery.
- Enters the thorax via the superior thoracic space.
- Descends anterior to the left lung origin.
- Crosses the aortic arch and avoids the vagus nerve.
- The route along the pericardium of the left ventricle.
- Pick and innervates the inferior skin of the diaphragm.
Location
Nerve fibers from the third, fourth, and fifth spinal nerves occur from the spinal cord in the neck. They come together to form the phrenic nerve in the neck, with the fourth cervical nerve principally given.
The newly formed nerve travels a long distance through the chest to transfer to the diaphragm. It runs through the mediastinum in the chest, which connects the lungs and houses the heart, blood vessels, esophagus, and other nerves.
The nerves take a somewhat different route when they pass through the posterior mediastinum (the space between the lungs) as they enter the chest:
- Near the left ventricle, the left phrenic nerve travels largely anterior to the pericardium, or lining of the heart.
- The right phrenic nerve goes just laterally to the right atrium and right ventricle of the heart after descending along the inner section of the lung.
- It then passes through the vena cava hiatus on its process to the diaphragm. The phrenic nerves then introduce into the left dome and right dome of the diaphragm, respectively.
The phrenic nerves pass through the diaphragm next reaching it. They access the muscle and innervate it from the lower skin.
Fortunately, damage affecting the spinal cord in the lower neck or chest area does not infect breathing. This is due to the phrenic nerve leaving the higher spinal cord in the neck.
Structure
The cervical spinal cord’s ventral horn is where the phrenic motor nucleus, which houses the phrenic nerve, is located. It declines obliquely with the internal jugular vein across the anterior scalene, deep to the prevertebral surface of deep cervical fascia and the transverse cervical and suprascapular arteries. On the left, the phrenic nerve crosses anterior to the first segment of the subclavian artery. On the right, it reclines on the anterior scalene muscle and crosses anterior to the second portion of the subclavian artery. On both sides, the phrenic nerve normally runs posterior to the subclavian vein as it enters the thorax where it runs anterior to the origin of the lung and connects the fibrous pericardium and mediastinal parietal pleura.
The right phrenic nerve crosses the source of the right lung anteriorly, then crosses the brachiocephalic artery posterior to the subclavian vein, before exiting the thorax by flowing via the T8 level of the diaphragm’s vena cava hiatus aperture. The right atrium is where the right phrenic nerve crosses. The left phrenic nerve carries the diaphragm independently and runs over the pericardium of the left ventricle. The pericardiacophrenic arteries and veins progress with their respective phrenic nerves.
The phrenic nerve could be marked by a line between these two points:
- 1st aim could be specified as 3.5 cm at the level of the thyroid cartilage from the midsagittal plane.
- 2nd aim is at the medial end of the clavicle.
Supply
The phrenic nerve is the single motor supply to each hemidiaphragm. It also gives sensory supply to:
- diaphragm.
- mediastinal pleura.
- pericardium.
- the central portion of the diaphragmatic pleura and peritoneum.
Blood supply
arterial supply: pericardiophrenic artery (divide of the internal thoracic artery).
Function
The phrenic nerve is a mixed nerve, that delivers motor, sensory and sympathetic fibers. The left and right phrenic nerves stimulate their own ipsilateral hemidiaphragm, which is the only nerve that gives motor activity to the diaphragm. Thus, the phrenic nerve stimulates the movements of the diaphragm and relaxes an essential part of breathing.
The phrenic nerve also provides sensory innervation to the central part of the diaphragm, as decently as the pericardium, mediastinal pleura, diaphragmatic pleura, and diaphragmatic peritoneum.
Clinical Significance
In a patient with left phrenic nerve palsy during fluoroscopy, forceful inhalation with the mouth closed causes the paralyzed left diaphragm to lift while the healthy right side descends.
Pain arising from structures supplied by the phrenic nerve is frequently “mention” to other somatic regions served by spinal nerves C3-C5. For example, a subphrenic sore below the right diaphragm muscle does a patient to feel pain in the right shoulder.
The distress of the phrenic nerve (or the tissues it supplies) directs to the hiccup reflex. A hiccup is caused by the diaphragm contracting spasmodically and pulling air up against the larynx’s closed band.
The phrenic nerve should be identified during thoracic surgery and preserved. A clinician may gently trick the phrenic nerve to elicit a dartle (diaphragmatic startle) response in order to validate its identity. The right phrenic nerve should be crushed by the vena cava clamp during liver transplantation. Severing the phrenic nerve, or a phrenectomy, do paralyze that half of the diaphragm. Bilateral diaphragmatic paralysis or BDP can also be created by spinal cord injury,
Multiple sclerosis, polyneuropathy, myopathy, and amyotrophy, as decently as motor neuron disease, infections, pneumonia, sarcoidosis, heart surgery, lung transplantation, and mediastinal tumors. Diaphragm paralysis is best proven by sonography. Breathing would be made more difficult but do continue provided the other nerve is injured.
The phrenic nerve act from the neck (C3-C5) and innervates the diaphragm, which is highly lower. Hence, patients suffering spinal cord injuries below the neck are still capable to breathe effectively, even with any paralysis of the lower limbs.
Depending on which nerves are destroyed when the brachial plexus is damaged, the arm, forearm, and hand may enhance paralyzed. The phrenic nerve has been clinically used to neurotic the musculocutaneous nerve and the median nerve in order to relieve occur palsy. The innervation to the injured nerve could be partially or completely repaired with this treatment with a high success rate (84.6%).
Additionally, with no effect on the phrenic nerve’s respiratory function, this treatment has led to the restoration of brachial plexus nerve function. The indication where pulmonary vital capacity is reduced has typically been a result of the use of the right phrenic as the donor for the neurotization whereas the use of the left phrenic nerve has not been significantly related to reduced pulmonary vital capacity.
Summary
The phrenic nerves play an important part in breathing. These nerves are at risk of injury and can create serious problems when damaged.
Paralysis of the diaphragm is created by damage to both phrenic nerves. This can occur during certain types of surgery or trauma. Some types of infectious and neuromuscular diseases can further affect the phrenic nerves. harm phrenic nerves could be treated with ventilation, diaphragm pacemakers, or surgery.
FAQs
Where does the phrenic nerve originate?
The phrenic nerve originates at the C3 through C5 nerve roots, which leave the spinal canal at the neck root and decline caudally, parallel to the pericardial sac to give the motor innervation to the diaphragm.
What is the phrenic nerve C3 C4 C5?
The phrenic nerve proceeds in the neck. It is formed from C3, C4, and C5 nerve fibers and declines along the anterior surface of the scalenus anterior muscle before entering the thorax to supply motor and sensory capture to the diaphragm. Its anatomic location in the neck leaves the nerve at risk of traumatic injury.
Where is the function of the phrenic nerve?
Your phrenic nerve plays a critical part in your respiratory system to assist breathing. It is the only nerve in your neurological system that sends signals to your diaphragm to enable movement. It sends signals that do your diaphragm to dilate and contract. These movements approve your lungs to inhale and exhale air.
What are the branches of the phrenic nerve?
The anterior, lateral, and posterior branches of the left and right phrenic nerves are located in the abdominal cavity. These are certainly peripherally in a radial pattern.
Why is it called the phrenic nerve?
The phrenic nerves manage the diaphragm, our big muscle of respiration (breathing). From the Greek, phrenic plane both diaphragm and mind. The ancient Greeks take that the diaphragm was the seat of our emotions.
Which nerve controls breathing?
The phrenic nerve is among the most significant nerves in the body due to its part in respiration. The phrenic nerve gives the primary motor takes to the diaphragm, the big respiratory muscle.
What is the phrenic nerve test?
The phrenic nerve stimulation test uses electric or magnetic stimulation to the neck to examine the phrenic nerve’s reaction. It was also approved by the phrenic nerve conduction research. A phrenic nerve that does not respond to stimulation can define the cause of paralysis of the diaphragm.
What nerve causes hiccups?
A cause of long-term hiccups is harm to or discomfort of, the vagus nerves or phrenic nerves. These nerves give the diaphragm muscle.
Are there two phrenic nerves?
The phrenic nerve is a mixed nerve, that delivers motor, sensory and sympathetic fibers. The left and right phrenic nerves stimulate their communication with the ipsilateral hemidiaphragm, and it is the sole nerve that distributes motor activity to the diaphragm.
Which phrenic nerve is longer?
Due to the asymmetric heart position and the lower position of the left hemidiaphragm, the left phrenic nerve is longer, drops less vertically, and is misleading and more superficial than the right phrenic nerve. The phrenic nerves provide whole motor activity to the diaphragm.



4 Comments