Physiology Clotting Mechanism
The clotting mechanism, also known as hemostasis, is a vital physiological process that prevents excessive blood loss following vascular injury. It involves a complex interplay of cellular and molecular components to form a hemostatic plug, which subsequently matures into a stable blood clot. Key players in this process include platelets, coagulation factors, and the endothelium.
When a blood vessel is damaged, platelets rapidly adhere to the exposed extracellular matrix, forming a primary hemostatic plug. This adhesion is mediated by von Willebrand factor and glycoprotein receptors on the platelet surface. Subsequently, activated platelets release various factors, such as ADP and thromboxane A2, which promote further platelet activation and aggregation.
What is Blood Clotting?
Coagulation, or blood clotting, is essential in reducing the quantity of bleeding that happens when a blood vessel is injured. The proteins in your plasma work with the platelets to form a clot over the wound, which stops the bleeding.
The body protects itself against blood loss through the clotting process. Vascular systems, platelets, coagulation factors, prostaglandins, enzymes, and proteins are among the substances that aid in the clotting process. Together, these elements form clots and stop blood loss.
What are the Symptoms of Blood Clotting?
While identifying your risk factors is crucial, it’s also vital to be aware of the symptoms of blood clots, which can vary depending on the location of the clot:
Heart – Breathlessness, sweating, nausea, dizziness, chest pain, pain in other upper body areas, and a heavy or painful feeling in the chest
Brain – a sharp headache that comes quickly, dizziness, difficulty speaking, weakness in the arms, legs, or face
Arm or Leg – Pain, edema, soreness, and warmth, either suddenly or gradually
Lung – severe chest pain, a racing pulse, dyspnea, sweating, fever, and a bloody cough
Abdomen – severe diarrhoea, nausea, and upset stomach
What risk factors for developing Blood Blotting?
- Obesity
- Pregnancy
- Immobility
- Smoking
- Oral contraceptives
- Certain cancers
- Trauma
- Certain surgeries
- Age (above 60)
- A family history of blood clots
- Chronic inflammatory diseases
- Diabetes
- High blood pressure
- High cholesterol
- Prior central line placement
Treatment of Blood Blotting:
Blood clots are treated differently depending on their location and your health. If you suspect a blood clot due to your symptoms, see a doctor immediately.
A number of scientific advances have improved blood clot treatment and prevention. Among the most modern treatments are:
Anticoagulants: Anticoagulants are medications that prevent the formation of blood clots.
Thrombolytics – medication that breaks apart blood clots
Catheter-directed thrombolysis – a surgical procedure in which a long tube called a catheter is inserted and directed towards the blood clot to release medication that breaks up the clot.
Thrombectomy – surgical clot removal
Should it transpire that you have a venous clot, your physician may suggest that you speak with a hematologist, a physician who specializes in treating blood disorders. A cardiologist, neurologist, and maybe a hematologist may be involved in a patient’s care if they have an arterial disease and are at risk of getting an artery clot.
Some patients can receive state-of-the-art therapies by taking part in clinical research. If you’ve been given a diagnosis, you should talk to your physician about whether or not you should take part in a clinical trial.
Are Blood Clots Preventable?
Blood clots are one of the most preventable types of blood diseases. There are several ways to lower your risk of blood clots, one of them is to try to lower your risk factors whenever possible. See your physician if you think behavioral or genetic factors might put you at risk. Make sure your doctor knows about all the drugs you use and any blood clotting disorders in your family history.
Physiology of Clotting Mechanism:
The body protects itself against blood loss through the clotting process. Vascular systems, platelets, coagulation factors, prostaglandins, enzymes, and proteins are among the substances that aid in the clotting process. Together, these elements form clots and halt blood loss.
Given the importance of blood to the human body, blood loss might be lethal. Blood is created during hematopoiesis and is then utilized to supply oxygen to tissues and cells. The body protects itself against blood loss through the clotting process. Vascular systems, platelets, coagulation factors, prostaglandins, enzymes, and proteins are among the substances that aid in the clotting process. Together, these elements form clots and halt blood loss. Vasoconstriction, adhesion, activation, and aggregation are the tactics employed by the contributing components to stop the leaky blood flow temporarily and replace the cork. The active form of fibrinogen, fibrin, stabilizes this fragile platelet block shortly after.
Cellular level:
Numerous proteins, enzymes, ions, endothelial cells, and platelets are among the biological components involved in the clotting process.
Organ system involved:
The blood clotting process involves the circulatory system, which includes blood vessels and the blood cell lineage.
Mechhanism of clotting:
The clotting process consists of two stages:
Primary hemostasis: Primary hemostasis is the development of a weak platelet plug.
Secondary hemostasis: The delicate platelet plug within a clot is stabilized by the fibrin network.
Primary hemostasis:
Primary hemostasis, or the formation of a weak platelet plug, is the result of four processes: vasoconstriction, platelet adhesion, platelet activation, and platelet aggregation.
The initial reaction to vascular damage is vasoconstriction. The first sign of blood vessel spasm is vascular injury. This vasospasm eventually causes an increase in vasoconstriction. The primary mediator of vasoconstriction is a strong vasoconstrictor known as endothelin-1, which is generated by damaged endothelium. Damaged endothelium exhibits sub-endothelial collagen, von Willebrand factor, ATP, and inflammatory mediators. Von Willebrand factor is produced by erythrocyte and is subsequently maintained in platelet a-granules. The von Willebrand factor is also produced by the Weibel-Palade bodies of the endothelium. Subendothelial collagen, ATP, inflammatory mediators, and von Willebrand factor exposure combine to facilitate platelet adhesion, the second step of primary hemostasis.
Platelet adhesion is the mechanism by which platelets attach to the exposed subendothelial von Willebrand factor. Following vascular damage, platelets migrate along arterial walls and adhere to exposed von Willebrand factor and subendothelial collagen. The platelet membrane’s phospholipid bilayer has a large number of G protein receptors. Specifically, the relationship between the two is established by von Willebrand’s factor in the endothelium binding to the G protein Ib-IX receptor on platelets. Various factors may activate the bound platelet during the third stage of primary hemostasis.
Following their attachment to the exposed von Willebrand factor, which is the site of the damaged artery, platelets undergo two specific processes that together makeup platelet activation. Second, platelets secrete cytoplasmic granules.
Ultimately, primary hemostasis allows a frail platelet plug to form, providing temporary bleeding control until secondary hemostasis occurs, which involves further stabilization of fibrinogen to fibrin via thrombin.
Secondary hemostasis:
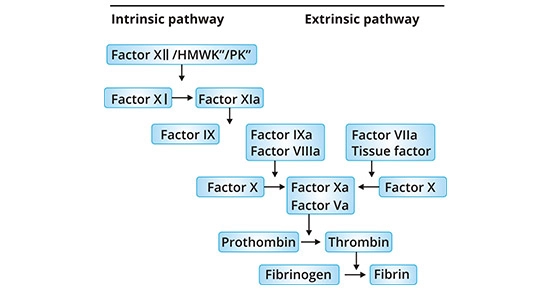
A sequence of clotting factors acting together stabilizes the weak platelet plug in secondary hemostasis. This requires the execution of three procedures: initiating the clotting factor activation, converting prothrombin to thrombin, and converting fibrinogen to fibrin. The first step in completing these jobs is to activate the clotting factor. This leads to the convergence of the intrinsic and extrinsic paths at factor X activation, where they execute their respective activities via the shared pathway. Please be advised that calcium ions are necessary for the entire secondary hemostasis process.
The extrinsic pathway includes the tissue factor and factor VII. When the tissue factor binds to FVII and activates it to become factor VIIa, a tissue factor-FVIIa complex is created. This molecule then activates Factor X. Note that Factor IX of the intrinsic pathway can be activated by the tissue factor-FVIIa complex, which is also referred to as the alternate route. After the tissue factor-FVIIa complex has changed Factor X into Factor Xa, the cascade continues in the same manner.
The intrinsic pathway consists of factor I, factor IX, factor VIII, and Hageman factor. To initiate the process, factor XII interacts with exposed subendothelial collagen and changes into factor XIIa. Subsequently, factor XIIa stimulates factor XI, and factor XIa stimulates factor IX, culminating in factor IXa. When factor VIII is engaged and factor IXa is present, factor X is activated. The cascade follows the common path when factor X is activated by the factor IXa-factor VIIIa combination.
The conventional path begins with Factor Xa activation. Factor Xa forms a prothrombinase complex on phospholipid surfaces, where it combines with Factor Va and calcium to activate prothrombin into thrombin. A serine protease degrades prothrombin and then activates thrombin. Factor XIIIa now initiates due to thrombin. When fibrin and factor XIIIa crosslink, a stabilized clot is formed.
Pathophysiology of clotting:
The process of a blood clot forming in a blood vessel is called thrombosis. The Virchow triad is a crucial idea that illustrates the initial pathological anomalies that might cause the clotting process to progress to thrombosis. The endothelial damage, hypercoagulability of the blood, and stasis or turbulent blood flow make up the trio.
Thrombosis can be caused by turbulent or uneven blood flow. Normal blood flow is smooth. Turbulent blood flow damages endothelial cells, which facilitates the formation of a thrombus. A weak vascular rupture is an illustration of irregular blood flow. Another characteristic of abnormal blood flow is venous stasis, which can lead to endothelial damage and thrombosis during bed rest following surgery, long-distance driving or flying, or immobility caused by obesity.
Endothelial injury results in platelet activation and thrombus formation. This might be due to irritation of the vascular endothelial surface. An inflammatory chronic disease that leads to endothelium damage is excessive cholesterol.
A person who has hypercoagulability, a blood condition, is more prone to thrombosis. Genetic clotting disorders like a Factor V Leiden mutation or acquired clotting illnesses like disseminated intravascular coagulation might be the cause of this.
Disorder of primary hemostasis:
- Von Willebrand Factor disease
- Bernard-Soulier disease
- Glanzmann thrombasthenia
- Medication-induced
Disorder of secondary hemostasis:
- Factor V Leiden
- Vitamin K deficiency
- Hemophilia
- Anti-phospholipid antibody syndrome
- Disseminated intravascular coagulation
- Liver disease
- Medication-induced
Defects of small vessels:
- Trauma
- Aneurysm rupture
- Vasculitides
Clinical significance of Clotting:
In addition to the pathophysiology, it’s critical to remember the following while managing a patient with clotting mechanism abnormalities:
Patients with:
Small amounts of bleeding in the skin or mucous membranes are frequently the first signs of primary hemostasis issues. Purpura and peticiae are two examples of this.
Secondary hemostasis problems are often the result of bleeding into soft tissue or joints.
Direct defects in small blood vessels often appear as palpable purpura and ecchymosis. These might collect and grow into a hematoma.
Summary
Coagulation, or blood clotting, is essential in reducing the quantity of bleeding that happens when a blood vessel is injured. The proteins in your plasma work with the platelets to form a clot over the wound, which stops the bleeding.
The body protects itself against blood loss through the clotting process. Vascular systems, platelets, coagulation factors, prostaglandins, enzymes, and proteins are among the substances that aid in the clotting process. Together, these elements form clots and halt blood loss.
FAQ
What is the physiology of clotting time?
Clotting times usually vary from four to ten times. This test determines the length of blood vessel constriction and platelet plug formation. The only ways to halt bleeding are blood vessel constriction and platelet activity because no clot is allowed to form.
What is the clotting mechanism called?
Blood thickens from a liquid condition to something nearly like a gel as a result of the coagulation process. The body controls when and how much bleeding occurs through the broader process of hemostasis, which also includes coagulation.
What are the 6 steps of blood clotting?
Platelets and damaged vessel walls release clotting factors.
An inert blood protein is transformed into a pro-thrombin activator by clotting factors.
The prothrombin activator transforms prothrombin into thrombin.
Fibrinogen is transformed into fibrin by thrombin.
RBCs and platelets get caught in the fibrin network, creating a blood clot.
What are the first four clotting factors?
The common route factors X, II, I, and I are the Stuart-Prower factor, proaccelerin, prothrombin, fibrinogen, and XIII, in that order.
How much clotting is there?
There are twelve clotting factors. They are just circulatory plasma proteins, nothing more. Every element involved in blood clotting is essential to the coagulation process.