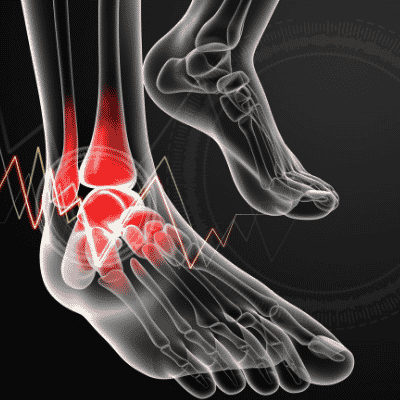
Distal Tibiofibular Syndesmosis
What is a Distal Tibiofibular Syndesmosis?
The distal tibiofibular syndesmosis refers to the fibrous joint connecting the tibia and fibula in the lower leg, specifically at the distal ends of these bones near the ankle. This syndesmosis is essential for maintaining the stability and integrity of the ankle joint during weight-bearing activities and is crucial for transmitting forces between the leg and the foot.
Injuries to the distal tibiofibular syndesmosis, often termed syndesmotic injuries, can result from various traumatic events, such as ankle sprains, sports-related injuries, or accidents. These injuries can range from mild sprains to severe disruptions, including syndesmotic instability or even frank diastasis between the tibia and fibula. Proper diagnosis and management of these injuries are critical to prevent long-term complications, such as chronic ankle instability, post-traumatic arthritis, and functional impairments.
Understanding the anatomy, mechanisms of injury, clinical evaluation, and appropriate treatment options are fundamental in effectively managing distal tibiofibular syndesmosis injuries and facilitating optimal recovery and long-term function for affected individuals.
Abstract:
A syndesmosis is a fibrous joint formed by strong ligaments or membranes connecting two adjacent bones. The distal tibiofibular syndesmosis, a syndesmotic joint made up of two bones and four ligaments, is likewise included in this concept. A syndesmosis is a complicated fibrous joint that allows for a small amount of movement and is joined by ligaments and a strong membrane between two bones.
Introduction
An essential part of the ankle joint that stabilizes the ankle and permits appropriate weight-bearing and movement is the distal tibiofibular syndesmosis. The tibia and fibula bones of the lower leg are joined by a fibrous joint called the syndesmosis. It is crucial for ankle stability and is situated above the ankle joint.
Articular surfaces:
An exact syndesmosis makes up the inferior tibiofibular joint, which is a fibrous joint. The reciprocally concave fibular notch on the distal end of the tibia and the triangular convex surface on the medial part of the distal end of the fibula is the articular surfaces of this joint.
Ligaments and joint capsule:
The inferior tibiofibular joint lacks an articular capsule and a synovial membrane since it is a fibrous joint. Rather, the talocrural joint’s synovial membrane enters this joint by projecting around 4 millimeters superiorly.

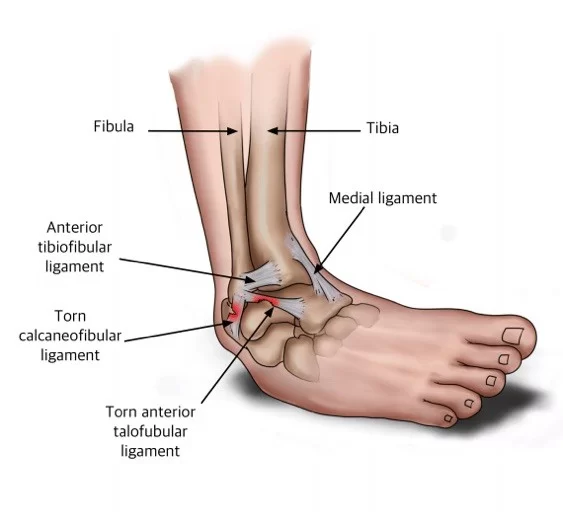
Three ligaments make up the distal tibiofibular syndesmosis:
- The transverse tibiofibular ligament (TTFL),
- The posterior inferior tibiofibular ligament (PITFL), and
- The anterior inferior tibiofibular ligament (AITFL).
The stability of the joint during dorsiflexion—the movement of lifting the foot upward toward the shin—is attributed to the AITFL, the ligament that sustains damage the most frequently from syndesmotic lesions. The TTFL offers horizontal stability, while the PITFL maintains stability during plantarflexion or the downward motion of the foot away from the torso.
The anterior, posterior, and transverse tibiofibular ligaments, as well as the interosseous ligament, hold the articular surfaces of the distal tibiofibular joint together.
- The interosseous tibiofibular ligament, which is continuous with the leg’s interosseous membrane, joins the facing surfaces of the bones. It is the main stabilizer of this joint and provides a tight connection between the bones.
- The anterior and posterior surfaces of the tibia and fibula are separated by the anterior and posterior tibiofibular ligaments, respectively. Both run laterally and inferiorly, with the posterior ligament having a larger and thicker course than the anterior. During foot movements, these ligaments cover the trochlear surface of the talus in turn; the anterior ligament covers the talus during dorsiflexion and the posterior ligament covers it during plantar flexion.
- The posterior tibiofibular ligament is situated deep to the inferior transverse ligament. Many scholars believe it to be the posterior tibiofibular ligament’s deep segment. The yellow ligamentous fibers that make up this structure have a higher density of elastic fibers than the white ligaments found in the majority of the body’s joints. Compared to other ligaments in this joint, this ligament has significantly greater stretchability.
Innervation:
The inferior tibiofibular joint is innervated by branches of the deep fibular and susurral nerves.
Blood supply:
The lateral malleolar branches of the anterior and posterior tibial arteries, as well as the perforating branch of the fibular artery, deliver blood to the inferior tibiofibular joint.
Available Motions:
- 2° outward rotation of the fibula with respect to the tibia
- The ankle mortise widens by just approximately 1mm when the ankle joint transitions from end-range plantar flexion to end-range dorsiflexion.
Movements:
The inferior tibiofibular joint permits distinct superior-inferior gliding of the bones and stretching of the interspace between them, despite being strongly anchored by a robust set of ligaments. These motions are intended to allow for talocrural joint mobility.
The fibula externally rotates during dorsiflexion of the foot, which causes the distance between the tibia and fibula at the inferior tibiofibular joint to significantly broaden. This movement also involves the translation of the fibula superiorly, and a superior gliding action succeeds it in the inferior and superior tibiofibular joints. On the other hand, plantarflexion of the foot causes the fibula to glide inferiorly at both tibiofibular joints and the distance between the tibia and fibula at the inferior tibiofibular joint to narrow.
Pain in the tibiofibular joint that occurs with stress is referred to as the capsule pattern. At the maximal dorsiflexion of the foot, the joint is closely packed, while in plantar flexion, it is loosely packed. The anteroposterior glide of the fibula against the tibia is the auxiliary movement within this joint.
Causes and Epidemiology
Athletes who play American football and downhill skiing frequently sustain syndesmotic ankle sprains. Football injuries are typically the consequence of an athlete forcing their foot to rotate externally while they are prone—that is, at the bottom of the pile. An additional cause of the injuries could be an impact on the lateral knee while the foot is planted and dorsiflexed, which would cause an eversion or external rotation moment at the talocrural joint.
The boot is designed to prevent dorsi- or plantar-flexion movement during downhill ski racing, which can lead to an excessive allowance of talocrural external rotation and damage to the interosseous membrane and anterior or posterior tibiofibular ligament.1–11% of all injuries are syndesmosis-related, according to research. According to research by Boytim et al., the incidence among professional American football players is substantially greater, reaching up to 29%.
What Are the Distal Tibiofibular Syndesmosis-Related Injuries?
There are two types of distal tibiofibular syndesmosis: acute and chronic. Traumatic incidents like fractures or sprains of the ankle frequently result in acute damage. Over time, chronic injuries may occur. These are a few typical injuries:
- Syndesmotic Ankle Sprain: This is the most frequent injury to the syndesmosis and is caused by a tearing or straining of the ligaments that attach to the lower leg’s tibia and fibula.
- High Ankle Sprain: This syndesmotic ankle sprain happens when there is a sprain, stretch, or tear in the ligaments connecting the tibia and fibula.
- Syndesmotic Rupture: This type of injury results in a complete rupture of the ligaments connecting the tibia and fibula bones, which can cause significant pain and instability in the ankle joint.
- Syndesmotic Diastasis: This injury type causes a separation or widening of the space between the tibia and fibula bones, which can cause significant pain and instability.
- Chronic Instability: This injury type results in chronic pain and instability in the ankle joint due to weakened or stretched syndesmosis ligaments over time.
What Indicates Distal Tibiofibular Syndesmosis Injury Symptoms?
Depending on how severe the damage is, the symptoms of distal tibiofibular syndesmosis injuries can vary, but some typical symptoms include:
- Pain: When the distal tibiofibular syndesmosis is injured, pain is frequently experienced. The pain can be strong and severe, and it is often felt outside the ankle, close to the lower leg bone.
- Swelling: One of the most typical symptoms of syndesmosis injuries is swelling around the ankle joint. Significant edema may make it difficult to move your ankles.
- Bruising: If the injury is the consequence of a stressful incident, such as a fall or an athletic event, there may also be bruising surrounding the ankle joint.
- Difficulty walking: Walking or bearing weight on the affected leg may be problematic in the event of a distal tibiofibular syndesmosis injury. This may be particularly true in cases of serious injuries.
- Instability: One of the most common symptoms of syndesmosis injuries is instability in the ankle joint, particularly if the ligaments that connect the tibia and fibula are ripped or strained. It is challenging to walk and carry out other tasks because of this.
- Reduced Range of Motion: Distal tibiofibular syndesmosis injuries can result in a reduction in the ankle joint’s range of motion, making it more difficult to move the ankle freely.
Compared to a lateral ankle sprain, the Syndesmotic will appear to have much less edema, as well as a loss of full plantar flexion and incapacity to bear weight. Because the interosseous membrane was injured, ecchymosis may develop several days after the injury. One frequently notices difficulties or incapacity to toe walk. Past medical history includes frequent sprains, protracted healing times, chronic discomfort, and the development of heterotopic ossification inside the interosseous membrane. When the foot is in an external rotation with high dorsiflexion, it is the most prevalent MOI.
Differential Diagnosis
During clinical diagnosis, it is crucial to rule out other pathologies with a similar mechanism of injury (MOI) due to the concealed nature of the high ankle sprain. Priority should be given to ruling out fractures of the tibia, fibula, and/or talus. Second, because the mechanisms of injury for the two ailments are fairly similar, the clinician should address concerns about a lateral ankle sprain.
“A history of an external rotation component can usually be used to distinguish syndesmotic ankle sprains from inversion ankle sprains,” according to Norwig. A severe contusion, infection, malignancy, dystrophic calcification, compartment syndrome, significant joint laxity, and severe ankle sprain are further potential diseases. Prior to starting treatment for a syndesmotic ankle sprain, these disorders should be preferred to be checked out.
Outcome measures
- The Disability Index for the Foot and Ankle (FADI) and
- The Lower Extremity Functional Scale (LEFS).
View the clinical presentation for examination Hx and MOI.

- Analysis of the gait and observation: Look for anomalies
- Palpate the medial and lateral malleoli for the presence of a fracture. In order to rule out Maissoneuve’s fracture, palpation of the fibula must be done from distal to proximal, including the proximal tibiofibular joint.
- Distal Pulses: Verify that pedal pulses are present.
- Girth Measurements: Feel for tenderness proximally over the anterior tibiofibular ligament and proximal along the interosseous membrane.
- Significant ankle swelling: estimate the girth in Figure 8.
Special Examination
1] Perform the Kleiger’s Test (dorsiflexion external rotation stress test).
- Ascertains whether the distal tibiofibular syndesmosis or the deltoid ligament has been severely damaged.
- Application of an external rotational force to the injured foot and ankle is done while the knee is flexed by 90 degrees and the ankle is in a neutral position.
- Test result (+): Anterolateral ankle pain. The talus moving away from the medial malleolus is a sign of injury to the deltoid ligament.
- 0.75 is the optimal interceptor kappa.
2] Squeeze Test:

- This is carried out by squeezing the tibia and fibula together above the injury.
- It separates the tibia and fibula and detects a fibular fracture or syndesmosis sprain.
- (+) test: If the condition is a syndesmosis sprain, the pain will be replicated along the distal tibiofibular junction, and if it is a fibular fracture, along the fibular shaft.
- Interrater = 0.5 (moderate).
3.] Cotton Test:

- It is used to determine whether syndesmosis instability is present when there is diastasis.
- It involves rotating the plantar heel straight from side to side while using one hand to support the distal leg and the other to hold it.
- Any lateral translation would suggest syndesmotic instability in the (+) test.
4.] Fibular Traslation Test:
- 77% Sensitivity, 88% Specificity, Beumer et al. (2011)
For injuries connected to distal tibiofibular syndesmosis, what is the diagnosis?
Your healthcare provider will probably do a physical examination and request imaging testing in order to evaluate an injury to the distal tibiofibular syndesmosis. A few common methods of diagnosis are as follows:
- Physical Examination: Your doctor will probably check your lower leg and ankle joint for discomfort, swelling, bruises, and instability. To evaluate a patient’s range of motion, they could also ask them to move their ankle in different directions.
- X-ray: Ankle joint X-rays are helpful to detect fractures or other bone injuries. An X-ray is also helpful to see if there is a wider gap between the tibia and fibula bones, which is a common indication of a syndesmosis injury.
- MRI: Images of the ligaments, tendons, and soft tissues surrounding the ankle joint can be obtained in great detail using magnetic resonance imaging (MRI). Determining the extent of an injury caused by syndesmosis can be aided by an MRI.
- Computed tomography (CT) scan is a useful diagnostic tool for identifying fractures and other bone injuries because it produces precise images of the bones in the ankle joint.
- Stress Test: To determine whether the syndesmosis is stable, your healthcare professional may subject your ankle joint to a stress test. If there is excessive movement or instability in your ankle, your provider may apply pressure to the joint or ask you to move it in different directions during a stress test.
Health Care Administration
Obtaining imaging as soon as feasible is recommended to rule out any anticipated fractures and help restore normal anatomy. Imaging is still the gold standard for diagnosis. The region of tibiotalar contact that is available during weight bearing decreases by 42% for every millimeter that the fibula moves laterally. It makes perfect sense how a misdiagnosed injury this “minor” could result in a lifetime of persistent sprains. As the imaging gold standard for ligamentous injuries, plain films are the bare minimum advice.
However, because of the intricacy of the tissues and structures, a CT scan is advised for bone detail. MRIs, on the other hand, provide an accurate view of the ligamentous damage. Arthroscopy is the only method that can match their accuracy. In order to differentiate an injury from a normal joint gap or overlap, bilateral imaging is performed. If there is no diastasis, syndesmotic ankle sprains are regarded as stable and are solved symptomatically. As tolerated, these individuals are instructed to bear weight.
Patients who have a sprain with latent diastasis, in which the reduction of the tibiofibular joint is watched on a CT or MRI scan, may not require surgery. Immobilization in a non-weight-bearing cast or walking boot for four to six weeks is a common treatment for patients with these results.
In patients without a fibular fracture who have a high syndesmotic ankle sprain and show syndesmosis diastasis, surgery is necessary. The fastest possible surgical stabilization is necessary. Results of surgical repair that involve both close treatment of the ligaments with open or percutaneous insertion of a transverse syndesmosis screw and open repair of torn ligaments are demonstrating positive.
How Are Injuries Associated with Distal Tibiofibular Syndesmosis Treated?
Depending on the extent of the injury, there are many treatment options for distal tibiofibular syndesmosis injuries. Treatment choices often consist of:
- Rest and Ice: To help with swelling and discomfort reduction, rest the ankle and apply ice to the afflicted area.
- Immobilization: If the damage is serious, immobilizing the ankle joint with a cast or brace is required.
- Medication: Acetaminophen and Ibuprofen are two examples of over-the-counter pain relievers that are helpful in treating pain and inflammation.
- Physical therapy: It suggests strengthening the ankle joint, increasing the range of motion, and lowering the chance of further injuries.
- Surgery: To reconstruct or normalize the injured ligaments in the ankle joint, surgery is required in extreme circumstances.
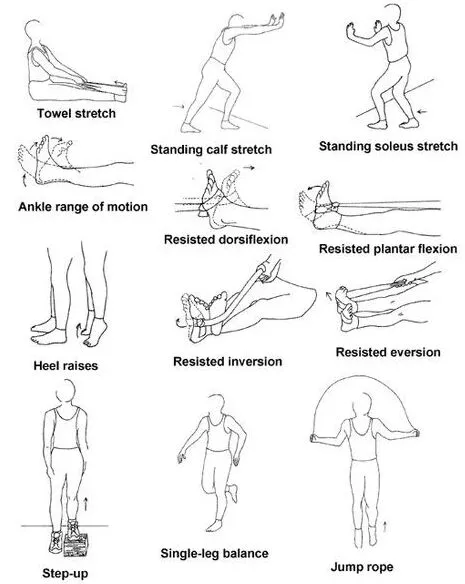
Handling Physical Therapy

1.) Step and Calf Stretch
2.) Exercises to Strengthen Your Calf
3.) The Lunge Calf Exercise
Aims:
- ROM, reducing discomfort and swelling, and shielding ligaments from more damage are the objectives for the first two weeks.
- Week 3 and beyond: Restore proper range of motion, fortify supporting muscles and ligaments, engage in training to increase balance and endurance
- Preventing more injury is the most crucial long-term objective!
Education of Patients:
- Follow the weight-bearing procedure suggested by the surgeon or physical therapist;
- Refrain from strenuous physical activity until full weight bearing and dynamic balance have returned to normal.
- Fall risk
Assistive Devices:
- Gait training with crutches or a boot/brace
- Crutches: Necessary until a pain-free, regular gait returns to normal;
- For unstable injuries, use a stirrup brace or walking boot.
Modalities:
- RICE (rest, ice, compression, and elevation) for the first 15 minutes, three times a day (Despite a commonly recognized treatment, Bleakley et al. claimed that there is insufficient data to support the use of RICE.
- It demonstrates that non-steroidal anti-inflammatory medications and comfrey ointment enhance the short-term healing process after an acute ankle sprain.

Therapeutic Exercise/ Neuromuscular Re-education:
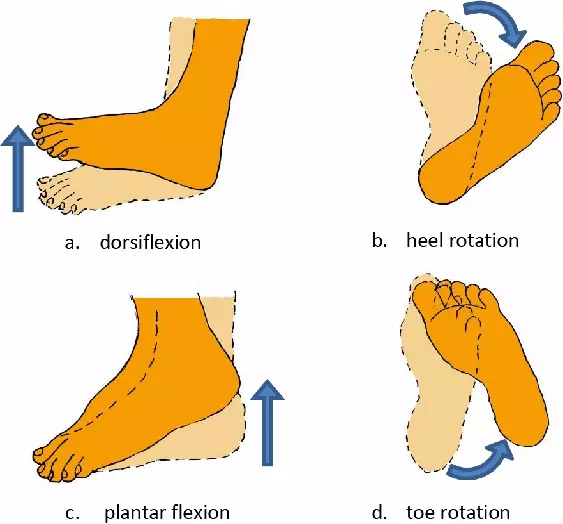
- AROM flexion, ankle alphabet, dorsiflexion/plantarflexion, and inversion/eversion with a theraband are all covered in the first two weeks.
- Weeks 3-4: Standing Stretch, seated dorsiflexion stretch with theraband, double heel raise progressing to single heel raise, and dorsiflexion stretching on a step stool
- To encourage a regular gait pattern, gradually increase your weight and practice walking on a treadmill.
- Ankle proprioception, postural reflexes, and balance during neuromuscular reeducation Example: Equilibrium position on one leg, training with a disk or balance pad, aquatic therapy
- Advance to running, cycling, agility, leaping, and exercises tailored to your sport.
- Avoid hyper-dorsiflexion (which puts stress on the mortise joint), loaded external rotation, and subtalar eversion in your training regimen.
Hand Therapy:
- Passive stretching and talocrural and subtalar joint accessory movement may be helpful in the manual therapy of stiffness.
- After extended mobilization, one 30-second A-P talocrural joint mob enhanced ankle dorsiflexion range of motion (ROM) instantly, according to researchers.
- Collins et al. reported that subjects showed immediate ROM gains when Mulligan’s movement with mobilization was applied in the sub-acute sprains and in patients with recurrent sprains.
- Green et al. reported that those who used RICE with manual therapy were more likely to reach this normal ROM within the first two weeks of the ankle sprain than those who received RICE alone.
What Is the Distal Tibiofibular Syndesmosis Prevention?
The following advice can help prevent these kinds of injuries:
- Wear suitable footwear.
- Develop the muscles surrounding the ankle joint.
- Be sure to warm up and stretch before beginning any strenuous activity.
- Steer clear of dangerous sports like basketball and skiing.
Summary
Walking difficulties, soreness, and swelling are possible symptoms of injuries to the distal tibiofibular syndesmosis, which may need medical care. The injury is pointed out with the aid of physical examinations and imaging studies. Depending on the degree of the damage, treatment options may include immobilization, medication, physical therapy, surgery, and rest. Many people can fully recover from these injuries and resume their regular activities with the right care and rehabilitation.
FAQs
What is the purpose of the syndesmosis between the tibiofibular bones?
The main purpose of the tibiofibular syndesmosis’s distal ligaments is to stop the fibula from moving out of its groove in the tibia, either laterally, anteriorly, or posteriorly.
Which are the four syndesmosis ligaments in the ankle joint?
The anterior inferior tibiofibular ligament (AITFL), posterior inferior tibiofibular ligament (PITFL), tibiofibular interosseous ligament (TFIL), and transverse tibiofibular ligament (TTFL) are the four ligaments that make up the syndesmotic ligament complex for the soft tissue.
How does one describe the distal tibiofibular joint?
A syndesmosis is a complicated fibrous joint that allows for a small amount of movement and joins the ligaments and a robust membrane between two bones. A syndesmotic joint is the inferior tibiofibular joint or distal tibiofibular syndesmosis.
References
- Here are some common methods of diagnosis: The author Vasković (2023, July 20). joint tibiofibular. Tibiofibular joints. Kenhub. https://www.kenhub.com/en/library/anatomy
- Nigam, A. July 5, 2023. Distal Tibiofibular Syndesmosis: An explanation. Distal tibiofibular syndesmosis can be found at https://www.icliniq.com/articles/orthopedic-health
- Ankle Sprains Syndesmotic. (n.d.). Syndesmotic Ankle Sprain Physiopedia. https://www.physio-pedia.com/
- On September 23, 2010, Hermans, J. J., Beumer, A., De Jong, T. A. W., and Kleinrensink, G. J. An adult distal tibiofibular syndesmosis anatomy: a multimodality-based graphic study. Wiley Journal of Anatomy, doi:10.1111/j.1469-7580.2010.01302.x
- Tibiofibular Distal Syndesmosis (n.d.). Distal Tibiofibular Syndesmosis is clarified in Physiopedia at https://www.physio-pedia.com.Syndesmosis i.e. #:~:text=A%20i