Posterior Cruciate Ligament (PCL) Injury
The posterior cruciate ligament (PCL) is placed right behind the anterior cruciate ligament (ACL) inside the knee. It is one of the ligaments that connects the femur (thighbone) to the tibia (shinbone). The posterior cruciate ligament prevents the tibia from rotating around the thigh bone.
A huge amount of force is required to injure the posterior cruciate ligament. A bent knee striking a dashboard in a car accident or a football player falling on a bent knee are two typical causes of damage. A severe twisting or contact injury during sports can also cause PCL damage.
The posterior cruciate ligament (PCL) joins your upper and lower legs. Even though your PCL is stronger and larger than your ACL, it may still be damaged. A PCL injury can cause discomfort, swelling, and other symptoms. Non-surgical and surgical treatments are available.
What is The posterior Cruciate Ligament?
The posterior cruciate ligament (PCL) is one of the four primary ligaments in the knee joint. It’s a thick tissue band that runs from the rear of your thighbone (femur) to the front of your shinbone (tibia).
The PCL’s major function is to keep your shinbone from shifting too far back concerning your thighbone. It also aids with knee rotation control and stability when bending and straightening your leg.
Anatomy of the posterior Cruciate Ligament
The posterior cruciate ligament (PCL) is the strongest and biggest intra-articular ligament in the human knee, and it serves as the major posterior stabilizer. It is made up of two functional bundles: the larger anterolateral (ALB) and the smaller posteromedial (PMB). The ALB’s femoral connection is roughly double the size of its tibial attachment.
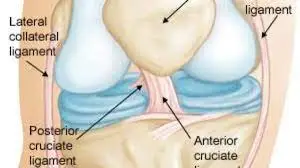
Origin
The PCL arises from the groove on the anterolateral portion of the medial femoral condyle.
Insertion
The PCL is inserted about 1 cm distal to the joint line along the posterior part of the tibial axis.
Blood supply
The posterior capsule is perforated by the middle geniculate artery, which runs parallel to the superior margin of the synovial septum. It connects to the synovium around the PCL, generating a plexus of vessels supplying the PCL. A branch of the inferior geniculate artery may potentially provide a supply.
Nerve supply
The posterior articular branches of the tibial and obturator nerves connect to the posterior capsule. To reach the PCL, these branches penetrate through the posterior capsule.
Function
The PCL is one of the primary knee joint stabilizers, especially resisting excessive posterior translation of the tibia relative to the femur. The PCL also serves as a secondary knee stabilizer, limiting excessive rotation between 90° and 120° of knee flexion.
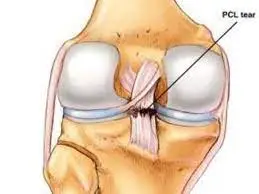
What is The Posterior Cruciate Ligament Injury?
- A posterior cruciate ligament (PCL) injury is a sprain or rupture of the PCL, one of your knee’s four main ligaments. This strong band of tissue goes from the rear of your thighbone (femur) to the front of your shinbone (tibia), regulating knee rotation and stability during bending and straightening.
- Injury to the posterior cruciate ligament is less prevalent than other types of knee ligament injuries. They are frequently more subtle and difficult to assess than other ligament lesions in the knee.
- A posterior cruciate ligament injury is frequently associated with damage to other components in the knee, including cartilage, other ligaments, and bone.
- Many posterior cruciate ligament injuries are only partial rips that can heal on their own. People who have merely torn their posterior cruciate ligaments may be able to return to sports without encountering issues with knee stability.
Causes of the Posterior Cruciate Ligament Injury
PCL injuries are less frequent than ACL tears, accounting for around 20% of knee ligament injuries.
They occurs mostly due to:
- Hyperextension of the knee: this can occur when landing violently with a bent knee, such as after a fall, or jump, or in sports such as skiing or football.
- A direct blow to the front of the knee: This might occur as a result of a vehicle accident, sports collision, or banging your knee on something hard.
- Severe Knee Damage: A dislocation or several ligament rips are examples of severe knee damage.
- Over Twisting: Landing on the front of the shinbone, as when a dancer returns from a leap. A simple misstep leads to a fall on a bent knee.
Symptoms of the Posterior Cruciate Ligament Injury
People who have had a PCL injury may have a variety of symptoms, including:
- Pain: Pain in the back of your knee that generally gradually gets worse over time.
- Swelling and stiffness: There is noticeable swelling around the knee joint, as well as stiffness that limits your range of motion.
- Instability: The sensation that your knee may “give way” or buckle, particularly while going down stairs or on uneven surfaces.
- Difficulty bending or straightening the knee: When attempting to bend or completely straighten your leg, you may encounter discomfort or a limited range of motion.
- To the touch, the back of the knee may be warm. This is due to the injury causing bleeding within the knee joint.
- Tenderness in the area of the knee joint. The knee, especially the rear of the knee, may be sore or sensitive to touch.
- Tingling or numbness in the knees. People with more severe PCL injuries may have tingling or numbness around the knee joint.
Diagnosis of the Posterior Cruciate Ligament Injury
A patient interview, physical exam, and medical imaging are typically used by a physician or other health practitioner to identify a posterior cruciate ligament (PCL) injury.
A person should be ready to answer inquiries regarding his or her medical history as well as specifics regarding the injury, such as:
- What caused the injury?
- When did the injury happen?
- Has the knee ever been injured?
- What is the exact location of the pain?
- Was a “popping” sound heard at the moment of the stated injury?
- Is your knee weak or unstable, as if it will give way?
Knee instability can indicate a recent, severe PCL injury or an undiscovered PCL tear from months or even years before.
In addition to a patient interview, the doctor will do a series of physical examinations to confirm a PCL tear diagnosis.
Physical Examination
- During a physical examination, the doctor will look for symptoms of trauma, such as bruising, swelling, and lacerations around the knee.
- Specific physical examinations, such as the posterior drawer test and posterior sag test, may be performed by the clinician.
Posterior drawer test
- The person is tested while lying on his or her back.
- The examiner will instruct the subject to bend their hip to 45° with their foot flat) and their knee to 90°.
- To stabilize the leg, he or she will lean softly on the person’s foot.
- Wrapping both hands over the joint line of the knee, the examiner will attempt to slide the tibia (shin bone) backward.
- This movement may be repeated multiple times to confirm the diagnosis.
The tibia will move backward because a damaged PCL has less resistance than an intact ligament.
Posterior sag sign examination
- This exam is carried out with the person being examined lying on his or her back.
- The doctor will bend the injured knee and hip to 90° angles, with the foot in the air, and grip the heel for support.
A PCL rupture is likely if there is a significant posterior sag in the affected knee (because of gravity).
Medical Imaging
The doctor may request an x-ray or other medical imaging in addition to a physical exam.
X-rays and magnetic resonance imaging (MRI) scans are two more processes that may assist your doctor to confirm your diagnosis. However, these pictures may seem normal, especially if the damage happened more than three months before the testing.
X-rays. Even though X-rays will not reveal any injuries to your posterior cruciate ligament, they can indicate whether the ligament tore off a piece of bone when it was wounded. This is known as an avulsion fracture. Your doctor may also conduct stress views to determine how far back the shin bone can move.
MRI: Magnetic Resonance Imaging(MRI)scans produce more accurate pictures of soft tissues, such as the posterior cruciate ligament, than X-rays. This type of diagnostic imaging provides a close-up image of the soft tissue that surrounds the knee joint.
Treatment of the Posterior Cruciate Ligament Injury
Non-Surgical Treatment
If you simply hurt your posterior cruciate ligament, your ailment may recover without surgery. Nonsurgical therapy methods may be suggested by your doctor:
- RICE. When you’re initially hurt, the RICE regimen (rest, ice, mild compression, and elevation) might help you heal faster.
- Immobilization. Your doctor may advise you to wear a specific brace to prevent the tibia bone from drooping backward (gravity pulls the bone backward when you lie down). You may be given crutches to prevent you from placing weight on your leg to further preserve your knee.
- Physical therapy: You will begin a cautious rehabilitation program after the edema has subsided. Specific exercises can help you regain knee function and improve the leg muscles that support it. A significant aspect of a good recovery is strengthening the muscles at the front of your thigh (quadriceps).
Surgical Treatment
- Patients with isolated PCL tears may also benefit from rebuilding if they have prolonged instability or discomfort that does not improve with non-operative therapy.
- A posterior cruciate ligament reconstruction surgery is normally conducted with an arthroscope and minor incisions; however, some surgeons will still make an extra incision on the side of the knee. Traditional open surgery is more invasive than arthroscopic surgery.
- Less invasive procedures have the advantage of causing less pain during surgery and allowing for faster recovery times. Advanced approaches enable patients to continue a broader variety of activities following rehabilitation.
- If you have several injuries, your doctor may advise you to have surgery. Surgery is usually required if you have dislocated your knee and damaged numerous ligaments, including the posterior cruciate ligament.
Exercises for the Posterior Cruciate Ligament Injury
Exercises for basic mobility that can be utilized as a part of a rehab program for posterior cruciate ligament damage.
Stretching Exercises
Heel slide with knee flexion

- Lie on your back and bend your knee, making sure your foot is in touch with the floor. Rep 10 to 20 times more.
- There may be some discomfort, but no pain.
- This may be developed to enhance the range of motion if necessary by pulling on the leg further than it normally extends with a towel or equivalent.
Stretching the calves

- Stretching your calf while standing:
- Place your hands on the wall at shoulder height and shoulder width apart as you face the wall.
- With your front knee slightly bent and your heel flat on the ground, take one step back.
- Press your hips on the wall as you bend forward until your back and calves start to stretch gently.
- After 30 seconds of holding, swap legs and do it again.
Hamstring stretch with straight legs

- The goal here is to give the healing tissue some elasticity rather than to improve flexibility. This stretch may also be done while sitting.
- Lean into the stretch by placing your foot on a table or similar surface and maintaining your leg straight and your chest up.
- Take the stretch as far as it is comfortable and relax into it. Strive to extend from the hips rather than the shoulders.
- A mild stretch in the back of the leg should be felt, but it should not be uncomfortable.
- Once or twice a day, do three sets of 10 seconds.
Strengthening Exercise (Early Stages)
Quad set with straight legs

- With your legs out in front of you and your back straight, take a seat straight on a chair or the floor.
- Tip your toes up in the direction of the ceiling.
- Push your knee into the floor or chair seat by using your quadriceps muscles, but do not raise your leg. The front of your thigh should start to tighten up.
- Hold for five to ten seconds, then let go and repeat ten to fifteen times.
Hamstring Isometric Contraction

- Spread your legs wide apart and place your feet flat on the ground while lying on your stomach.
- Press your heels into the floor without raising your legs to activate your hamstrings.
- Hold for five to ten seconds, then let go and repeat ten to fifteen times.
Strengthening Exercise (Late Stages)
Calf lift

- Just elevate and lower yourself on your toes while maintaining a straight gait.
- Try to do three sets of ten to twenty reps per day.
- Later in the rehabilitation process, single-leg calf rises and single-leg calf raises without leaning against a wall or holding onto anything are two ways to advance this activity.
Hamstrings Curls

- This bodyweight exercise involves holding onto a stable object and bending one knee at a time towards your buttocks while keeping your leg straight.
- It challenges balance and coordination while offering a functional movement pattern. These can be performed without any weight at first against a wall, then with a rehabilitation band, and finally with a weight.
- In one fluid motion, curl up against resistance and down again. Try for three sets of ten to twenty reps.
- The amount of recuperation time needed in between sessions may grow as strength and resistance rise.

Squats in quarters
- Stand back up after lowering yourself to about a fourth of its height. Try for three sets of ten to twenty reps.
- To advance this, lower yourself to halfway (Phase 3 of rehabilitation) and then do full squats (to horizontal) in the phases tailored to your sport. Just add weight to make it more intense.
- When doing squats, make sure your abdominal muscles remain tight.

Lunge
- Positioning one leg ahead of the other. To lean forward and stand again, bend your front leg.
- Try for three sets of ten to twenty reps. You may add weight to increase the intensity.
- Make sure you maintain your tummy muscles taut while doing this exercise.

Heel drop
- Bend one leg so the other’s heel nearly touches the floor while standing on a step or anything similar that is up to six inches tall, then take a step back to the beginning position.
- Continue until your muscles are tired.
Prevention
Total prevention of PCL injuries might be challenging. That being said, there are a few things you can do to lower your risk:
Stretching before exercise will help to maintain the health of your knee joints. When you’re running or walking, use the right form. Playing sports requires you to be attentive and cautious.
Summary
If the damage to your PCL is not too severe, you could recover quickly. If the ligament suffered significant damage, however, you may not be able to rehabilitate your knee and it may get weaker.
After recovering from PCL surgery, patients often experience increased stability and mobility. To safeguard your joints, keep in mind that you might still need to wear a knee brace when engaging in vigorous activity.
FAQs
What are the signs and symptoms of a cruciate ligament injury?
A PCL injury causes the following symptoms:
Knee swelling and discomfort in the popliteal fossa (region behind the knee), Instability of the knee joint, and Knee joint discomfort.
How long does a posterior cruciate ligament damage take to heal?
Athletes should consult with their doctor to determine when they may return to their sport. As long as there are no further consequences from the injury, most athletes may return to their sport within eight weeks.
How do you repair a posterior cruciate ligament injury?
If you have a PCL injury, you may need to walk on crutches until the swelling and discomfort subside.
A brace to provide support and stability to your knee.
Physical therapy can aid in the improvement of joint mobility and leg strength.
Reconstruction of the PCL and perhaps other tissues in the knee.
Can you bend your knee if you have a torn PCL?
A person may have difficulties bending the knee, resulting in a limp or difficulty climbing or descending stairs. Weight-bearing is difficult. Standing or walking on an injured knee can be difficult or uncomfortable, especially for lengthy periods.
References
- Posterior cruciate ligament injuries – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/posterior-cruciate-ligament-injuries/
- Professional, C. C. M. (n.d.-c). Posterior cruciate ligament (PCL) injury. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21793-pcl-posterior-cruciate-ligament-tears
- Posterior cruciate ligament. (n.d.). Physiopedia. https://www.physio-pedia.com/Posterior_Cruciate_Ligament
- Walden, M. (2023, October 26). Torn PCL rehabilitation exercises. Sportsinjuryclinic.net. https://www.sportsinjuryclinic.net/sport-injuries/knee-pain/acute-knee-injuries/rehabilitation-pcl-injuries
- Khadavi, M. M. M. M., MD, & Khadavi, M. M. M. M., MD. (n.d.). Posterior cruciate ligament (PCL) injuries. Sports-health. https://www.sports-health.com/sports-injuries/knee-injuries/posterior-cruciate-ligament-pcl-injuries






One Comment