Pott’s fracture (Ankle malleoli Fracture) And Physiotherapy Management
- Ankle malleoli Fracture fracture, also known as Pott’s syndrome and Dupuytren fracture, is an archaic term loosely applied to a variety of bimalleolar ankle fractures.
- The injury is caused by a combined abduction external rotation from an eversion force.
- This action strains the sturdy medial (deltoid) ligament of the ankle, often tearing off the medial malleolus due to its strong attachment.
- The talus then moves laterally, shearing off the lateral malleolus or, more commonly, breaking the fibula superior to the tibiofibular syndesmosis.
- Care should also be taken to avoid missing the less common causes of ankle pain, namely; small fractures around the ankle and foot (e.g. Pott’s fracture).
Anatomy related to Potts fracture
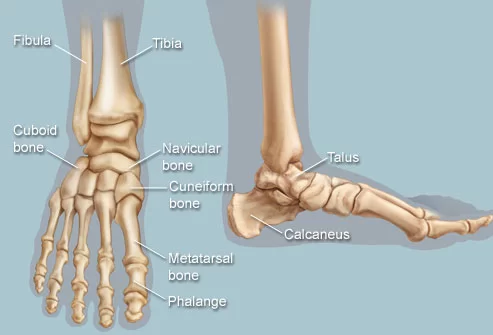
- The ankle contains three joints. The talocrural joint or ankle joint is a hinge joint formed between the inferior surface of the tibia and the superior surface of the talus.
- The medial and lateral malleoli provide additional articulations and stability to the ankle joint.
- The inferior tibiofibular joint is formed by the articulation of the distal parts of the fibula and tibia. The inferior tibiofibular joint is supported by the tibiofibular ligaments or syndesmosis.
- The subtalar joint between the talus and calcaneus is divided into an anterior and posterior articulation separated by the sinus tarsi.
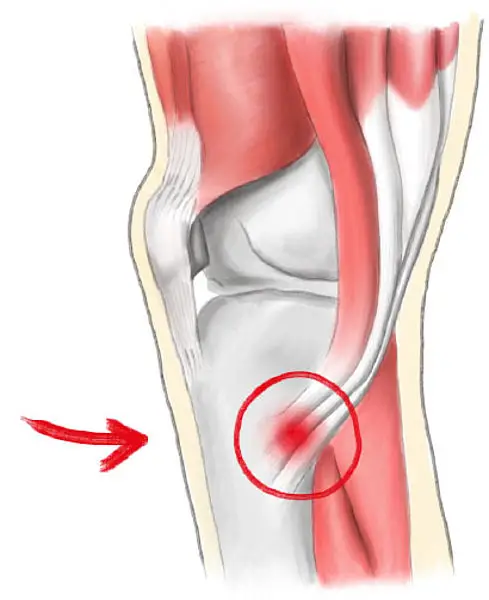
- The lateral ligament consists of three parts: the anterior talofibular ligament which passes as a flat band from the tip of the fibula anteriorly to the lateral talar neck; the calcaneofibular ligament, which is a cordlike structure directed somewhat posteriorly; and the posterior talofibular ligament, which runs posteriorly from the fibula to the talus.
Mechanism of injury of Potts fracture
- A Pott’s fracture is a fracture affecting one or both of the malleoli. During activities such as landing from a jump (volleyball, basketball) or when rolling an ankle, a certain amount of stress is placed on the tibia and fibula, and ankle joint.
- When this stress is traumatic, and beyond what the bone can withstand, a break in the medial, lateral, or posterior malleolus may occur.
- Also, activities involving a sudden change of direction, such as football and rugby, can cause fractures around the malleoli. When this happens, this condition is known as a Pott’s fracture.
- A Pott’s fracture often occurs in combination with other injuries such as an inversion injury, a dislocation of the ankle, or other fractures of the foot, ankle, or lower leg.
- Pott’s fractures can vary in location, severity, and type including displaced fractures, un-displaced fractures, bi-malleolar fractures, or compound fractures.
- It is difficult to distinguish clinically between a fracture and a moderate-to-severe ligament sprain.
- Both conditions may result from inversion injuries, with severe pain and varying degrees of swelling and disability.
Clinical Presentation of Potts fracture
- Patients with a Pott’s fracture typically experience a sudden sharp and intense pain around the ankle or lower leg immediately at the time of injury.
- The pain is situated at the front, back, the inner or outer part of the ankle or lower leg. The patient may have heard a “crack” as well. Due to the pain, the patient limps to protect from the injury.
- In severe cases, weight-bearing may be impossible. Patients with Pott’s fracture usually experience swelling, bruising, and pain on firmly touching the affected region of bone.
- Pain may also increase during certain movements of the foot or ankle or when attempting to stand or walk.
- When it is a displaced fracture, an obvious deformity may be noticeable. Also, disability such as flat foot is common in Pott’s fractures case.
- And the reason for this is because of a person with Pott’s fractures. This is because in many instances of a Pott’s fracture the foot goes into right angles at a valgus position, and the muscles which support the arch of the foot are put on the stretch, therefore the person with Pott’s fracture walks in this faulty position and a flat foot develops.
Classification of Pott’s Fracture:
Pott’s fracture is according to the number of malleoli involved, the mechanism of injury, joint stability, or the level of the fracture. 3 main classifications are:
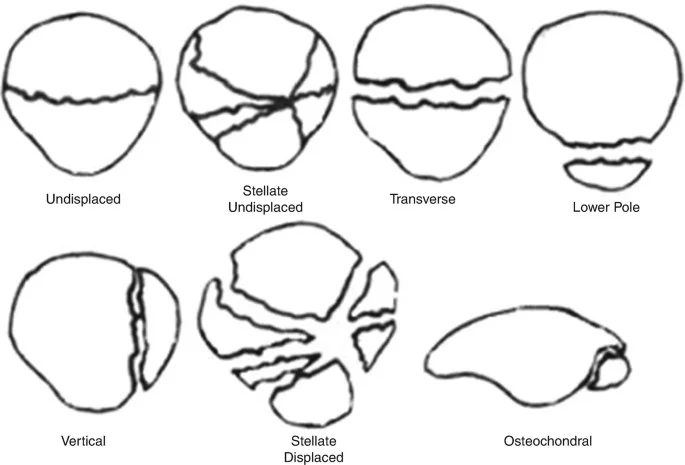
(1) Henderson’s Classification
This is the easy classification depending on the number of malleoli fractured when seen on skiagram.
- Type 1- Unimalleolar
- Type 2- Bimalleolar
- Type 3- Trimalleolar
This does not show with fracture pattern, mechanism of injury, or associated ligamentous injuries.
(2) Danis Weber’s Classification
It depends upon the level of the fracture of the fibula.
- Type 1- Fracture below the level of syndesmosis of the fibula.
- Type 2- Fracture at the level of syndesmosis of the fibula.
- Type 3- Fracture above the level of syndesmosis of the fibula.
(3) Lauge-Hansen’s Classification
It is based on experimental observations, radiographic and clinical examinations. It also depends upon the mechanism of injury such as the position of the foot during the time of injury and the direction of the deforming force later.
It has the following types:
1) Supination-Adduction:
Below the level of the syndesmosis, the lateral malleolus has a transverse avulsion fracture or a torn lateral collateral ligament. A vertical fracture of the medial malleolus will occur if the stress is applied indefinitely.
2) Supination-External Rotation
It causes
disruption of anterior tibio-fibular ligament,
spiral oblique fracture of distal fibula,
disruption of posterior tibiofibular ligament
fracture of posterior and medial malleolus or rupture of the deltoid ligament.
3) Pronation-Abduction
it leads to:
transverse fracture of the medial malleolus
rupture of the deltoid ligament
rupture of all syndesmotic ligaments
avulsion fracture of syndesmotic ligament insertions
a short, horizontal fracture of the fibula above the level of syndesmosis.
4) Pronation-External Rotation
it leads to:
transverse fracture of medial malleolus
disruption of the deltoid ligament
disruption of the anterior tibiofibular ligament
short oblique fracture of fibula above the level of the Ankle joint
continues force leads to rupture of posterior tibio-fibular ligament
postero-lateral part of tibia avulsion fracture
5) Pronation-Dorsiflexion
It causes:
fracture of the medial malleolus
fracture of anterior margin of tibia
supramalleolar fracture of fibula
transverse fracture of posterior tibial surface.
(4) AO’S Classification
This classification is a variation of the Danis Weber classification. 3 main types of fracture have been described according to the level of the fibular fracture.
Each of these types are further divided into 3 subgroups.
Type A. – Fibular fracture below syndesmosis
- A1-isolated
- A2-with fracture of medial malleolus
- A3-with a postero medial fragment
Type B. Fibular fracture at level of syndesmosis
- B1-isolated
- B2-with medial lesion
- B3-fracture of posterolateral tibia with medial lesion
Type C. Fibular fracture above syndesmosis
- C1-diaphyseal fracture fibula-simple
- C2-diaphyseal fracture fibula-complex
- C3-proximal fracture fibula
Diagnosis of Potts fracture
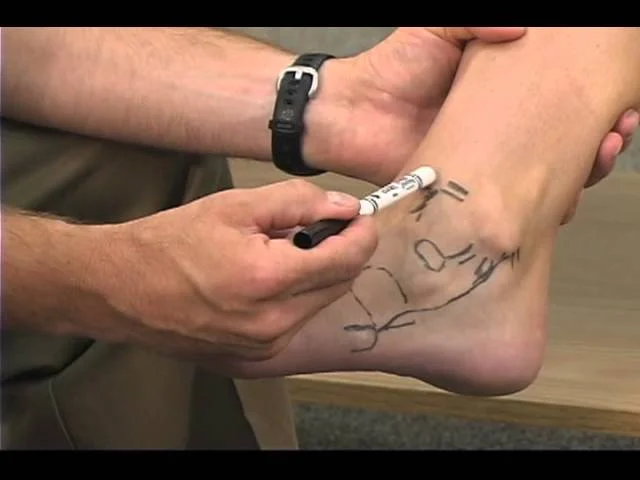
- In the diagnosis of Pott’s fracture, there is a need for a careful history of the patient and an increase in the diameter of the leg at the malleoli level suggests a fibular fracture (Keen’s sign of Pott’s fracture). Diagnosis of a Pott’s Fracture can be confirmed on x-ray.
- Once diagnosed it is often standard protocol to classify the fracture using either Lauge-Hansen’s classification based on the rotational mechanism of injury or the Danis-Weber Classification system that takes into consideration the position of the distal fibular fracture in relation to the syndesmosis of the ankle joint.
Management of Potts fracture
- One of the most important components of rehabilitation following Pott’s fracture is that the patient rests sufficiently from any activity that increases pain.
- Activities that place large amounts of stress on the ankle should also be avoided, particularly excessive weight-bearing activities such as running, jumping, standing, or walking.
- Displaced Pott’s fractures where the anatomical relationship of the bones of the ankle has been disrupted need to be a surgical fixation. Post-operatively, protective boot, brace, plaster cast, and/or crutches are used for a number of weeks.
- For fractures that are not displaced, treatment may involve a plaster cast immobilization and the use of crutches, followed by the use of a protective boot or brace for a number of weeks.
Physiotherapy management of Potts fracture
During immobilization
- Limb elevation
- Strong repeated movements for the toes, knee, and hip.
- Diapulse may be applied over the POP cast for relieving pain.
- Non–weight-bearing crutch walking can be initiated on the second or third day of immobilization.
During mobilization
During the immobilization period, Ankle joint stiffness is the most common symptom, so mobilization of the Ankle is the best option to improve the range of motion of the Ankle joint.
- Thermotherapy: If there is no oedema, thermotherapy is advisable. It increases capillary permeability, promoting the reabsorption of extravasated fluid and dissolution of organized haematoma, helping early healing.
- Early passive mobilization: Early initiation of relaxed passive range of motion exercises is important.
- The patient should be made well conversant to practice them often. This can be done best by the patient sitting in a chair with the back supported.
- The distal portion of the affected leg rests just over the knee on the sound thigh.
- The ankle and foot, which are free to move, are grasped by the patient using both hands.
- Full-range relaxed passive movements of the ankle and foot can be improved effectively with repetitive efforts with the use of HP or warm water immersions.
- Relaxed passive movement in the maximum possible range, especially circumduction, causing minor discomfort but not pain is ideal, to begin with.
- The passive movement should not be so forcible as to overstretch the fibrils that are gaining longitudinal attachment within the healing breach; nor should they be so gentle as to fail to disengage those fibrils that are gaining abnormal transverse adherence.
- Deep friction massage is also useful in preventing adhesions.

- Early muscle strengthening: Exercises to strengthen all the muscles should also be started as early as possible.
- The technique may be the same as described for early mobilization, except that the movements are active in this exercise.
- It can be made self-resistive also if there is no pain. The movements should be taken to the maximum range, with isometric holding at the end of the range.
- As the exercises are self-resistive, the degree of resistance can be controlled to the level of pain and discomfort
- While strengthening the muscles the patient should be told to concentrate more on the muscles of the anterior and lateral compartments of the leg which are usually weaker as compared to those of the posterior compartment.
- Exercising the toe flexors and intrinsic muscles should not be neglected, to maintain the tone and strength of the foot arches. In fact, active slow circumduction with toes tightly clenched is a simple and more effective exercise.
- Stretching exercises: It is important to stretch the posterior calf muscles. This needs prolonged gradual relaxation of the calf.
- It can be done by keeping the forefoot on a block or a book and pushing the heel down with the knee straight in standing, or with the knee bent to 90 degrees in sitting; putting downward pressure over the knee with a block or a book placed under the forefoot.
- In standing, the bodyweight presses the heel down and stretches the gastrosoleus (Calf muscles).
- Re-education in weight-bearing: Proper placement of the injured limb, gradual weight-bearing, and the normal pattern of gait is to be progressed in stages. Weight-bearing is started after 12 weeks.
- Speedy movements: Gradual initiation and progress to more vigorous exercises like toe walking, heel walking, spot jogging, and single-leg hopping.
Fractures treated by open reduction and internal fixation
- The period of cast immobilization after surgery is usually less, about 3–4 weeks. Therefore, mobilization can be started early. Gentle relaxed passive movements, as well as self-assisted procedures followed by thermotherapy, should be started.
- The rest of the physiotherapeutic regime is the same as described for the conservative approach.
- However, SWD or US is contraindicated due to the metallic implants used for internal fixation.
Related History
Physician Percivall Pott have an injury in 1765 and describe his clinical findings in a medical journal which are published in 1769.
Dupuytren fracture term named for Guillaume Dupuytren. Percivall Pott did not mention the disruption of the tibiofibular ligament, whereas Guillaume Dupuytren describe it.
you should read these:
FAQs
What is a Pott’s fracture?
A fracture that affects one or both malleoli is known as a Pott’s fracture. The tibia, fibula, and ankle joint are subjected to some stress during sports like landing from a jump (volleyball, basketball), or while rolling an ankle.
Where is Pott’s fracture?
A break in the lateral or medial malleolus, one of the bony protrusions on the sides of the ankle, is what distinguishes a Pott’s fracture from other types of ankle fractures. These two bones can occasionally fracture simultaneously, generally as a result of a severe ankle sprain.
What are the complications of Pott’s fracture?
A Pott’s fracture can result in long-term problems include persistent discomfort, instability of the ankle joint, and an elevated risk of ankle arthritis if it is ignored or incorrectly treated.
What are the symptoms of Pott’s fracture?
Pott’s fracture symptoms are
Ankle pain that strikes suddenly and severely.
It won’t be possible for you to bear weight on your leg.
At the site of the fracture, there will be soreness.
There will be a lot of swelling and bruising.
What is a first-degree Pott’s fracture?
“Pott’s fractures” is frequently used to refer to fractures affecting the ankle joint:
One malleolus is broken in first-degree Pott’s fractures, while two are broken in second-degree Pott’s fractures, bimalleolar fracture of two malleoli.
What causes a Pott’s fracture?
An eversion force mixed with an external rotation generated by abduction is what results in the damage. Due to its strong connection, the medial malleolus is frequently torn off by this motion, which stresses the ankle’s strong medial (deltoid) ligament.