Patellar Fracture
Introduction
- A fracture in the patella, the little, flat bone that shields your knee joint, is called a patella fracture. It is typically brought on by a direct injury, such as a blow to the knee, a fall, or a collision, such as hitting the dashboard in an automobile accident.
- A significant injury that might affect your ability to bend or straighten your knee is a patella fracture. While there are simple cases of patella fractures, this little bone can also split into several fragments.
- A fracture in the patella, also known as the kneecap, is a break in the tiny bone located at the front of the knee. The patella serves as a protection for your knee joint, so if you fall on it or bang it up against the dashboard in an automobile accident, it might break. A catastrophic injury that can make it difficult or impossible to walk or straighten your knee is a patellar fracture.
- Wearing a cast or splint until the bone heals might be the treatment for certain mild patellar fractures.
- Nonetheless, the majority of patellar fractures result in the bone fragments shifting during the injury.
- Surgery is required for these more complex fractures to stabilize and repair the knee. Enable the function to return.
What occurs if the patella cracks or fractures?
- A direct blow to the knee is typically the cause of a patella fracture. The force used might cause it to split into two parts, develop a hairline crack, or break into several little bits.
- Your knee’s extensor mechanism may stop working correctly if you have a patella fracture. Your patella is where your quadriceps and patellar tendon join, and this allows you to flex and extend your knee.
- Your knee joint is cushioned by the cartilage covering your patella. This kind of fracture may cause damage to the cartilage, which may result in post-traumatic arthritis.
Anatomy
- The patella, the biggest sesamoid bone in the human body, is located in front of the knee joint within the quadriceps tendon.
- The bone is made up of many quickly combining ossification centers that form between the ages of three and six.
- The patella is a triangle bone that is thick, and flat and points downward at its tip. The base of the bone is proximally located, and it has medial and lateral borders.
- The patella is a compact, thin lamina that covers a thick trabecular bone. If located on the superior surface, the quadriceps muscle attachment extends distally onto the anterior surface.
- The attachments of the vastus lateralis and medialis are represented by the rough markings located at the lateral and medial margins of the patella.
- The patellar ligament attachment is represented by those at the apex.
- The patellar ligament, which attaches to the tibial tuberosity on the front side of the tibia, originates near the apex of the patella.
- Several vascular apertures located in the central third of the patella enable arteries to enter and nourish the bone.
- The anterior projection of the lateral femoral condyle and the horizontal fibers of the vastus medialis support the patella.
- Stability is further aided by the strain in the medial patellar retinaculum.
Surfaces
- The subcutaneous anterior surface is characterized by many rough, longitudinal striae, tiny holes for the flow of nutrition vessels, and convexity in all directions.
- The tendon of the quadriceps femoris, which extends beyond the superficial fibers of the ligamentum patellae, covers this area in its current state. A bursa separates it from the integument.
- Up to 4 to 5 mm of articular cartilage covers the posterior surface. This facilitates the force’s dissipation.
- It appears above a smooth, oval, articular region that is separated into two facets by a vertical ridge.
- The facets represent the medial and lateral portions of the femur, while the ridge corresponds to the groove on the patellar surface.
- The lateral facet is the deeper and larger of the two faces of the same surface. Anatomically, the medial facet varies significantly. Along the medial facet’s extreme medial boundary is where the third odd facet is located.
Borders and Muscle Attachments
- Thick, rough, and sloping forward, downward, and to the side, the base or superior border provides attachment to the part of the Quadriceps femoris that originates from the Rectus femoris and Vastus intermedius.
- The narrower medial and lateral borders merge below, where they connect to the parts of the quadriceps femoris that originate from the medialis and lateralis of the Vastus.
Apex
- The ligamentum patellae is attached to the pointed apex.
- The apex is located just in front of the knee joint line when one is standing comfortably.
- structure
- The patella is made up of a thin, compact lamina covering fairly uniformly thick cancellous tissue.
- The cancelli are positioned parallel to the front surface, just underneath it. They extend forth from the articular surface to the other portions of the bone.
Ossification
- The patella is ossified from a single center that may not become visible until the sixth year, but it often does so in the second or third year. Rarely, two centers that are next to each other form the bone. This process of osseous gradation ends around puberty.
Functions of the patella
- Mostly serves as the quadriceps muscle’s anatomic pulley. Increasing the extensor mechanism’s lever arm makes knee flexion more efficient and thereby raises quadriceps strength by 33–50%.
- In the past, the patella was thought to function as a frictionless pulley in which the quadriceps tendon’s force and the patellar tendon’s force were equal.
- Recent research, however, indicates that the patella functions more like a balancing beam, varying the force, direction, and length of its two arms—the patella tendon and the quadriceps tendon—at different degrees of flexion.
- The patellofemoral contact region on the patella surface shifts from distal to proximal with increasing flexion.
- This shift in the contact region causes the lever arm and mechanical benefit that the patella offers the quadriceps.
- It functions as a “spacer” in between the femoral condyles and the quadriceps tendon, protecting the tendon from compression and friction while minimizing stress concentration by distributing pressures uniformly to the underlying bone
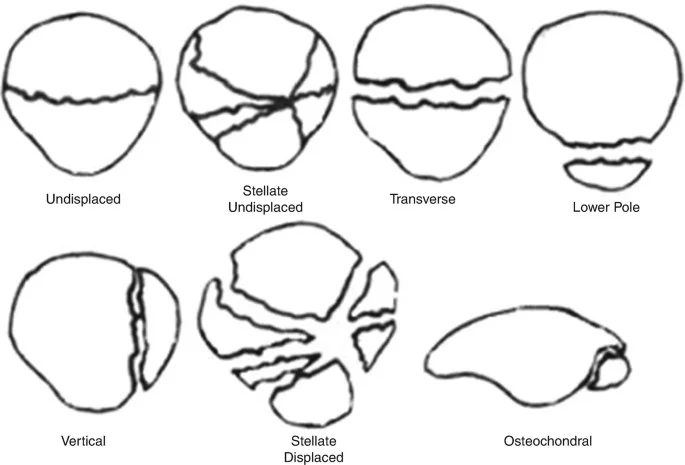
Types of Patellar Fractures
- Stable fracture: The fractures of this kind are nondisplaced. The bone fragments could stay close to one another or could be a millimeter or two apart. When there is a stable fracture, the bones often mend without moving.
- Displaced fracture: The shattered ends of the bone are not aligned correctly and are separated in a displaced fracture. Another possibility is damage to the typically smooth joint surface. Surgery is frequently necessary for this kind of fracture to fuse the broken bone back together
- Comminuted fracture: The bone breaks into three or more fragments in this kind of fracture. A comminuted fracture can be stable or unstable, depending on the particular pattern of the fracture.
- Open fracture: An open fracture occurs when a wound extends down to the bone or when the bone breaks in a way that protrudes through the skin. An open fracture may take longer to heal and frequently results in harm to the soft tissues around it.
- Open fractures are more dangerous because there is a greater chance of infection in both the bone and the wound when the skin is broken. Treatment must begin very early to prevent infection
- Osteochondral Fracture: The layer of cartilage at the base of the patella, where it joins the other bones in the knee joint, may also sustain a displaced fracture. To stop bones from rubbing against one another when moving, cartilage, a smooth substance, lines the ends of the bones in joints. An osteochondral fracture is an injury to this cartilage and the underlying bone. This kind of injury is usually a closed fracture.
- Osteoarthritis: A degenerative disease of the joint marked by cartilage degradation, is more likely to occur in cases of all types of patella fractures because they can cause cartilage damage.
- People who have osteochondral fractures are more likely to develop osteoarthritis of the knee since these fractures invariably impact the knee’s cartilage.
Causes of Patellar Fracture
- An injury to the knee is frequently linked to patella fractures. Typical reasons include:
- landing squarely on one’s knee, particularly on a hard surface like concrete
- Sports where a ball, bat, or stick might strike a player in the knee directly
- Where the knee strikes the dashboard in a car accident
- injuries from gunshots
- The tendon tugging on the kneecap and breaking it apart is caused by abrupt contractions (pulling) of the quadriceps muscle.
Symptoms of Patellar Fracture
- pain around the kneecap
- bruising
- Even with very mild kneecap fractures, swelling can occur.
- the inability to extend the leg straight or to bend the knee
- incapacity to walk, stand, or bear weight
- knee deformity, particularly in cases of serious fractures
- bone that protrudes from the knee’s skin when a patellar fracture is open
Diagnosis
- Correctly determine the type of fracture that has occurred and diagnose a fractured patella.
- A broken patella can cause discomfort and make walking difficult or impossible, depending on how severe the break is.
- In cases when a knee injury results in excruciating pain or if the bone pokes through the skin, medical professionals advise visiting an emergency center right away.
- In the doctor’s office, knee injuries that are less serious or painful can be identified.
- Examine the patient physically to rule out fractures and evaluate symptoms and indicators such as pain, edema, and deformity.
- The doctor frequently requires more information on the severity of a fracture, such as if a bone fragment has detached from the patella, and may take comprehensive pictures of the knee.
Physical Exam
- In addition to determining the degree of deformity and edema, find out what kind and how much pain you’re feeling.
- As soon as the bone pokes through the skin, an open fracture is evident. Surgery is always necessary for open fractures.
- If you have a knee injury and you can see bone, you should seek emergency room care right away.
- When a patient has a closed fracture—one in which the broken bone is still under the skin—the doctor will inquire about the nature of the injury, the level of pain, and the precise location of the discomfort.
- To assess whether any additional tendons, ligaments, or bones are affected, the doctor can ask you to flex or extend your leg as much as you can.
- In an examination, the physician also inquires about your family history and health. It is helpful to our experts to know about any prior knee injuries or other medical disorders as this aids in their diagnosis and treatment recommendations.
- X-ray: A patella fracture’s site can be determined using X-ray scans. They also assist your physician in determining if the break only affects the surface or penetrates through the bone.
- CT Scan: A CT scan is a series of X-rays that are used to produce two- or three-dimensional images of the knee, which allows medical professionals to inspect a patella fracture from a variety of perspectives.
- If an X-ray shows that there is more than one patellar fracture or if bone fragments have come away from the patella and are now in other areas of the knee, your doctor could advise a CT scan.
- New radiology procedures are employed by professionals to guarantee the lowest radiation exposure possible during CT scans.
- An MRI: An MRI may be advised by medical professionals if a patient has a serious patella fracture and bone fragments have damaged ligaments, tendons, or nerves.
- A magnetic resonance imaging (MRI) scan can detect whether a bone fragment is pushing on a nearby nerve or whether there are strained or torn ligaments or tendons in the soft tissue around the knee.
- In cases when soft tissue is injured, physicians could advise surgery right away.
- Bone Scan: If your pain and swelling point to a fractured patella and more imaging is required, your doctor can advise a bone scan if an MRI is not an option due to an implanted pacemaker or other metal device. This is uncommon, though.
- A technician will first inject a tiny quantity of dye into a vein in your arm. This dye, known as a tracer, passes through the circulation and gathers in the areas where your tissues and cells are actively repairing themselves.
- Following an hour or two for the tracer to pass through the bloodstream, a radiologist uses a specialized camera to take pictures of the tracer while they scan your body. If it gathers more in some areas than others, there can be an injury present.
Treatment of Patellar Fracture
Initial Treatment
- Your knee will swell up and you might not be able to straighten your leg if you break your patella. The discomfort and lack of function of your leg will likely prevent you from being able to walk.
- Typically, you will be seen in urgent care or the emergency room (ER), where an x-ray of your knee will be taken.
- The radiologists will use the X-rays to assist them diagnose whether your patella is broken. An MRI or other imaging test may be necessary if you have torn tendons, such as the patella tendon or the quadriceps tendon, as they may not show up clearly on an x-ray.
- Compared to X-rays, which display bone lesions, MRIs are far better at showing soft tissue damage. It might not be necessary to perform this in the ER, planned for a later time.
- In most cases, you can be treated with a straight leg brace and sent home as long as the skin around your patella is normal (no wounds, no internal skin pressure).
- Make an appointment within the following several days to a week with your physician or an orthopedic surgeon. If the fracture was an open or complicated fracture, the bone will have broken through the skin, and you will probably need immediate hospital admission and surgery.
General Treatment
- Whether or not the bone fragments are in contact and whether or not your leg can be straightened are the main determinants of treatment.
- Your thigh muscles are no longer attached to your lower leg, so if the components are torn apart, you probably won’t be able to straighten your knee.
- If that’s the case, reconstructing the broken bone parts will probably require surgery. Your ability to extend your leg will return as a result, which will facilitate walking.
- Occasionally, the patella may break, but the bones remain together and do not separate. Your knee can still be straightened if that occurs since the strong soft tissues around and surrounding your kneecap are still intact.
- You might not require surgery, but they’ll probably be wearing a brace and facing limitations on their ability to bend and bear weight.
- A kneecap can be operated on in a variety of ways. Restricting the bones is the primary objective.
- This allows you to straighten your knee out once again by re-connecting your tibia to your thigh muscles. A patella can be fixed using sutures, wires, plates, or a combination of these.
Non- Surgical Treatment
- Surgery might not be necessary if the bone fragments are not misaligned or dislocated. To assist in restricting your leg from moving and keep your knee straight, your doctor could put on a splint or cast.
- This will maintain the appropriate alignment of the fractured bone ends while they recover.
- You might be able to wear a cast or brace while bearing weight on your leg, depending on the details of your particular fracture.
- However, weight-bearing is prohibited for six to eight weeks following certain fractures. You and your doctor will discuss any limitations on weight-bearing.
- a splint or cast to stabilize the leg while the fracture heals
- preventing or minimizing childbearing
- Painkillers (non-opioid painkillers should be used in the initial days following a serious kneecap fracture, as opposed to opioids)
- Walking assistance and physical treatment to help you regain your strength and independence
Surgical Treatment
- If the bone fragments are dislocated, surgery will probably be required. If the fractures are not close together, the patellar bones may not heal or may mend slowly.
- Strong thigh muscles that link to the top of the patella can pull shattered fragments out of position as they recover.
- Your doctor could advise delaying surgery until any abrasions (scrapes) have healed if the skin surrounding your fracture has not ruptured.
- However, there is a higher danger of infection if the bones are visible through the skin, thus surgery is usually done as soon as feasible.
- The surfaces of the bone and the wounds from the damage are carefully cleaned out during surgery. Usually, the same procedure will be used to fix the broken bone.
Surgical Procedures
- The kind of fracture you have will frequently determine the sort of operation that is done. Your doctor will go over your operation and any possible issues with you before the surgery.
- The most common methods for securing these two-part fractures are screws, pins, wires, and tension bands in the “figure-of-eight” arrangement. The two halves are pressed together by the figure-of-eight band.
- The fractures closest to the patella’s core respond well to this treatment. The kneecap’s terminal fracture fragments are too tiny for this operation.
- The tension band may overcompress—that is, force together excessively—fragmented breaks.
- Securing the bones with tiny screws or tiny nails is an additional method of treating a transverse fracture.
- The patella may fracture into many tiny fragments on the top or, more frequently, the bottom.
- This kind of fracture happens when the kneecap is crushed when the individual falls on it after initially being torn apart from the injury. Your doctor will remove the bone pieces since they are too tiny to be put back in place.
- Subsequently, they will reattach the detached patellar tendon to the residual patellar bone.
- In cases when the kneecap is fractured at the center and the fragments are not aligned, your physician may want to employ a wire and screw repair technique.
- Resection of minor non-reconstructable sections of the kneecap may also be beneficial.
Physiotherapy Treatment
- To reduce discomfort and inflammation: After applying a crepe bandage from the far end toward the body, spend fifteen to twenty minutes cryotherapy from the far end toward the close end.
- Finish with a deep friction massage that lasts five minutes and uses a rotating friction method to help with edema.
- Towards improving the range of motion: Start the recovery process with gentle workouts that are designed to keep joints mobile and avoid stiffness.
- Aim for 90 degrees of knee flexion after first focusing on the range of 30 to 60 degrees. Work on developing knee flexion gradually.
- Active assistance in knee flexion and extension is allowed during these workouts, as long as the knee is constantly protected from loads in the valgus and varus directions.
- Utilize the quadriceps and hamstrings using the Muscle Energy Technique, modifying according to the patient’s tolerance and following the guidelines of Reciprocal Inhibition.
- To aid in the restoration of patellar mobility, include exercises for patellar mobilization in the program. Add passive-graded mobilization strategies as well.
- To improve your muscle strength: Start with simple ankle exercises that are isotonic. Exercise your quadriceps isometrically. Include workouts using the isometric hamstrings.
- To recover strength and muscle mass in the quadriceps, perform isometric movements from a variety of angles.
- Make the Vastus medialis oblique stronger. Include a variety of gluteal exercises to assist the patient in getting up from a sitting posture.
- while keeping your hip extensor muscles strong. Incorporate the clamshell exercise to improve lateral rotation and abduction.
- Make the switch to a more difficult open
- Among the chain exercises are leg lifts while in a supine posture, knee extensions while sitting, hip abductions and adductions in a supine position, hip flexions and extensions in a prone position, and hamstring curls performed in a prone position.
- Training your gait For the first four weeks, continue walking without bearing any weight. Transition to lightweight bearing between weeks five and six.
- After the sixth week, progressively increase the strain on the afflicted leg by introducing partial weight bearing.
- Complete weight bearing should be resumed twelve weeks following surgery: The goal of the Focus on Gait Retraining phase is to improve the patient’s gait mechanics. It motivates the patient to gradually improve their gait while maintaining a high std of walking.
- Among the chain exercises are leg lifts while in a supine posture, knee extensions while sitting, hip abductions and adductions in a supine position, hip flexions and extensions in a prone position, and hamstring curls performed in a prone position.
- Training your gait For the first four weeks, continue walking without bearing any weight. Transition to lightweight bearing between weeks five and six.
- After the sixth week, progressively increase the strain on the afflicted leg by introducing partial weight bearing.
- First 14 weeks: the Advanced Training and Functional Activities phase begins, bringing increasingly challenging activities including walking on different surfaces, mastering stair climbing, and effectively navigating through numerous barriers.
- Improving proprioception with instruction: When the patient has healed to the point that they can bear weight comfortably, these elements are incorporated into the post-fracture rehabilitation regimen.
- Exercises for balance go from basic activities like standing on one leg and keeping your eyes open to more difficult ones. These might include things like standing on one leg while closing one’s eyes, or throwing and catching a ball while keeping your balance on the limb that is affected.
- Use lower limb-specific Proprioceptive Neuromuscular Facilitation procedures to increase strength. Drills for coordination incorporate such like Sideways backward-facing lunges to improve general balance.
- Joint position sense exercises that need the affected joint to be actively moved. through its range of motion, to mimic particular postures devoid of visual signals.
- These exercises are essential for improving proprioceptive abilities, which enable the body to accurately sense the position of joints.
Recovery
- Phase 1: In-Patient Rehabilitation (0-1 Weeks): Inform the patient about the benefits of physiotherapy recovery.
- Exercises to increase joint strength training and range of motion were initiated, along with the use of an air mattress to avoid bed sores and to preserve strength and mobility.
- Describe physiotherapy and the dos and don’ts for this particular ailment. to avoid developing new issues or problems.
- To reduce the possibility of pressure sores, great care was taken to make sure the ankles were positioned appropriately and that early movement was promoted.
- Additionally, it was advised to follow an isometric training plan for the quadriceps, hamstrings, and glutes to assist preserve the strength of the lower limb muscles.
- Phase 2: Out-Patient Rehabilitation (2-4 Weeks): The goals of the second phase, which lasted for two to four weeks, were to maintain the gains from the first phase while further increasing the range of motion.
- The therapy plan started with active-assisted range-of-motion exercises for the ankle and knee to accomplish this. It was then progressed to active range-of-motion exercises.
- Along with the beginning of bedside sitting, vigorous quadriceps exercises were also used at this time.
- The patient’s regimen also included strength-building activities, such as isometric workouts for the back and abdominal muscles and pelvic bridging training.
- Phase 3: (5-8 Weeks): The main goals at this point were to enhance the patient’s general health and restore their capacity to do everyday tasks. T
- he exercises from the initial and subsequent stages were preserved and carried out.
- The third step involved moving from partial weight-bearing to full weight-bearing and then progressing to balance and proprioceptive training to obtain ambulation.
Complications of Patellar Fractures
- Posttraumatic Arthritis: One kind of arthritis that appears after an accident is called posttraumatic arthritis.
- Even in cases when your bones mend properly, over time discomfort and stiffness may result from damage to the articular cartilage that covers your bones.
- A tiny proportion of people who have patellar fractures go on to develop severe arthritis. Much more prevalent is chondromalacia patella, a disease characterized by mild to severe arthritis.
- Muscle Weakness: Following a fracture, certain individuals may experience lifelong weakness in the quadriceps muscle located in the front of the leg.
- It is also typical to have some loss of knee range of motion, including flexion (bending) and extension (straightening). Usually, this loss of mobility is not immobilizing.
- Chronic Pain: Patellar fractures can result in persistent discomfort in the anterior region of the knee.
- Although the exact etiology of this discomfort is unknown, posttraumatic arthritis, stiffness, and muscular weakening are probably factors.
- Some patients discover that wearing a knee brace or support makes them more comfortable.
Summary
- Whether surgery or non-surgical therapy was used for you
- The length of time required for recovery
- In three to six months, the majority of patients will be able to resume their regular activities. It could take longer for people with serious fractures to resume their normal activities.
- To preserve your knee and avert more issues, your doctor could advise making certain lifestyle adjustments.
- This might entail staying away from exercises that require frequent deep knee bends or squats.
- Additionally, you should refrain from walking on steep inclines and using ladders or steps.
FAQ
Is a fractured patella serious?
A catastrophic injury that can make it difficult or impossible to walk or straighten your knee is a patellar fracture
Can a fractured patella be repaired?
To fix a broken kneecap, two surgical procedures can be used: Procedures for open reduction-internal fixation (ORIF): The surgeon makes an incision in the skin and uses metal wires, pins, or screws to reassemble the damaged bones. Broken bone fragments that are too small to be repaired are taken out.
How should a broken patella be treated?
To assist in restricting your leg from moving and keep your knee straight, your doctor could put on a splint or cast. This will maintain the appropriate alignment of the fractured bone ends while they recover. Depending on the particular fracture you have, if you have a brace or cast on your leg, you might be able to carry weight on it.
How long does it take to recover from patellar repair?
Physical therapy, immobilization, and anti-inflammatory drugs all aid with this. Recuperation from a torn patellar tendon typically takes six months. An exercise regimen designed to increase joint strength and mobility will be provided to you.
How excruciating is a fractured patella?
A broken patella can cause discomfort and make walking difficult or impossible, depending on how severe the break is





One Comment