Pes Anserine Bursitis and Physiotherapy Management
What is a Pes Anserine Bursitis?
- Pes Anserine bursitis, also known as intertendinous bursa, is an inflammatory condition of the bursa of the conjoined insertion of the sartorius, gracilis, and semitendinosus.
- We can locate this at the proximal medial aspect of the Knee, two inches below the medial knee joint line between the pes anserine tendons.
Anatomy
- The Pes Anserine bursa is a fluid-filled vesicle. It secretes synovial fluid in order to reduce friction between tissues, and also works as a cushion for bones, tendons, and muscles.
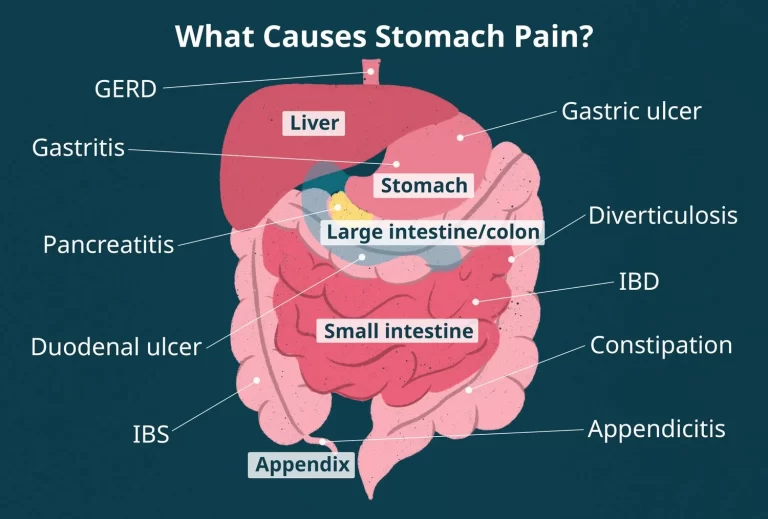
- The inflammation of the bursa does not appear suddenly but rather progresses over a period of time. Bursitis can also occur in the shoulder, knee, hip, elbow, and big toe.
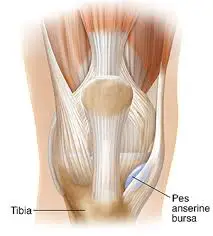
- The Pes Anserine, also called the ‘Goose Foot’ is the insertion of the sartorius, gracilis, and semitendinosus muscles, which are conjoined proximally on the medial side of the Tibia.
- The three tendons of the Pes Anserine are located superficial to the medial collateral ligament (MCL) of the knee. The sartorius and gracilis muscles are adductors of the leg (i.e. they pull the leg towards the median axis of the body).
- The semitendinosus muscle is part of the hamstring muscle group located at the back of your upper leg. Together, these three muscles are primarily flexors of the knee and internal rotators.
Causes of Pes Anserine Bursitis
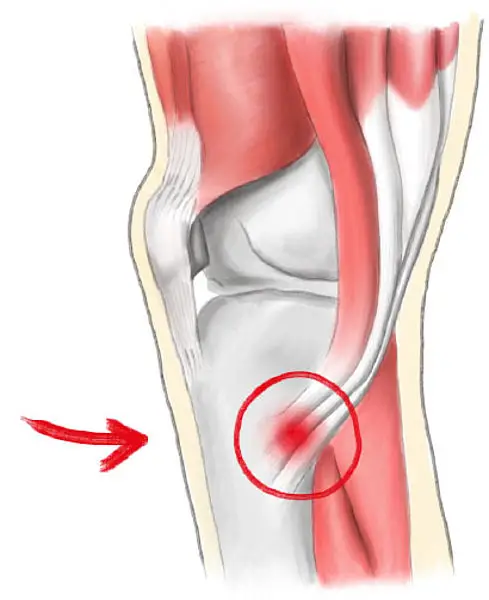
- Pes Anserine bursitis often occurs when the related muscles are repeatedly used, by doing movements such as flexion and adduction. This causes friction and also increases pressure on the bursa.
- The bursitis can also be due to a trauma, such as a direct hit in the Pes Anserine region. A contusion to this area results in an increased release of synovial fluid in the lining of the bursa.
- The bursa then becomes inflamed and tendered or painful and underlying Osteoarthritis of the knee.
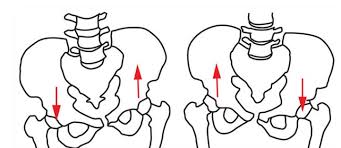
- Reports suggest that anserine bursitis is more common in overweight middle-aged females. We can explain this by the fact that women have a wider pelvis, resulting in angulation of the knee in the frontal plane, which leads to more pressure in the area of insertion of the pes anserinus by genu valgum.
- We can say that an inflamed bursa is not a primary pathology, but rather a consequence of an earlier complication.
Symptoms of Pes Anserine Bursitis
- Pes Anserine bursitis causes pain on the inside of the knee (mostly during running or taking stairs). The patient may experience spontaneous anteromedial knee pain on climbing or descending stairs and tenderness at the PA.
- Also, the region around the bursa will be swollen or tender to the touch.
- Other clinical presentations may include:
- Decreased muscle strength
- Gait deviations
- Decreased function
- Decreased ROM
- Postural dysfunction/impaired lower extremity biomechanics
- Aggravating factors include activities that require movements like flexion and endorotation, as well as exorotation and adduction. Pivoting, kicking, squatting, or quick movements from side to side, such as in the sports mentioned above, may also cause further.
Epidemiology
There is significant overlap with other knee disorders, making the precise prevalence of this condition in the general population uncertain. However, pes anserine pain was common in around one-third of 1% of participants in a big research including over 10,000 people. In one study, it was shown that over 90% of patients with concurrent osteoarthritis also had pes anserine discomfort, however, bursitis was not always present.
Furthermore, obese ladies with osteoarthritis in their knees have been found to have a higher incidence of anserine bursitis. According to the theory, women were more likely to experience it because of their broader pelvises, greater knee angulation, and more pressure on the anserine insertion site.
Differential Diagnosis
- Septic bursitis
- Osteomyelitis
- Gout
- Medial meniscus tear
- L3-L4 radiculopathy
- Medial collateral ligament tear
- Suprapatellar bursitis
- Proximal tibia stress fracture
- Prepatellar bursitis
- Semimembranosus bursitis
- Knee cysts
- Meniscal cysts
- Intra-articular synovial cysts
Diagnosis
- Lateral X-ray views of the patient’s knee are very useful for ruling out a stress fracture, arthritis, or even Osteochondritis Dissecans. An MRI is needed to clarify damage caused to other regions of the medial side of the knee.
- An MRI could prevent unnecessary arthroscopy. MRI findings should be compared with those of a physical examination.
- Sinography (radiography of a sinus following the injection of a radiopaque medium) is the best method for establishing the diagnosis when other imaging modalities, including MRI and CT, are not feasible.
- A Lidocaine/Corticosteroid injection in the area of the bursa will help determine the contribution of this pathology to the patient’s overall knee pain.
Examination
- The pes anserine bursa can be palpated at a point slightly distal to the tibial tubercle and about 3-4 cm medial to it.
- Examine hamstring length with the patient in the supine position. Bend the patient’s hip 90° and then extend the knee as far as possible. How far the knee can be extended will indicate hamstring length and tightness. If the patient’s knee can be straightened completely than the hamstrings are not tight.
- With the sports-related variant of pes anserine bursitis, symptoms may be reproduced by means of resisted internal rotation and resisted flexion of the knee. With the chronic variant in older adults, flexion or extension of the knee usually does not elicit pain.
Treatment of Pes Anserine Bursitis
- The initial treatment of pes anserinus bursitis should include relative rest of the affected knee and non-steroidal anti-inflammatory drugs (NSAID).
- Additional modalities, including local injection of a corticoid such as methylprednisolone, are indicated is some cases. Intrabursal injection of local anesthetics, corticosteroids, or both constitutes a second line of treatment.
- Surgical treatment is indicated in cases with failure to conservative treatments. Simple incision and drainage of the distended bursa can improve symptoms in some reported cases.
- The bursa may be removed if chronic infection cannot be cleared up with antibiotics. After surgery, if the bursa is removed, follow the same steps of rehabilitation and recovery outlined under physical therapy management.
- If the bursitis becomes infected and standard antibiotic treatments are ineffective, A surgical decompression of the bursa may be a solution in this case.
Physiotherapy Treatment

- SHORT WAVE DIATHERMY: short wave diathermy is a deep heating modality that uses heat to provide pain relief, improves the blood supply to targeted muscles, and removal waste products.
- TENS: transcutaneous electrical nerve stimulation is an electrical modality that provides pain relief by providing pain modulation.TENS closes the gate mechanism at the anterior grey horn in the spinal cord. also stimulates the endogenous opioid system which prevents the release of substance p at the anterior grey horn.
- ULTRASOUND: ultrasound is a therapeutic modality that generates ultrasound causes deep heat, provides micro-massage to soft tissue, increases flexibility, promotes healing of tissue as well improves localized blood supply to the area. and ultimately pain relief.
- Physiotherapy is the mainstay in the treatment of the Pes Anserine syndrome. To temper the pain caused by bursitis, the most important thing of all is rest.
- Avoid stairs, climbing, or other irritating activities to quiet down the bursa and the related pain. Nonsteroidal anti-inflammatory drugs (NSAID) can be taken to alleviate the pain.
- Restrict movement and alternately apply ice during the inflammatory phase.
- An ice massage of 15 minutes every 4-7 hours will reduce the inflammation.
- An elastic bandage can be wrapped around the knee to reduce any swelling or to prevent swelling from occurring. Be careful not to increase friction. Teach the patient muscle-conditioning exercises.
- These may include leg stretching exercises such as hamstring stretch, standing calf stretch, standing quadriceps stretch, hip adductor stretch, heel slide, quadriceps isometrics, hamstrings isometrics.
- Progression of these exercises may involve closed-kinetic chain exercises such as single-knee dips, squats, and leg presses. Resisted leg-pulls using elastic tubing are also included.
- The closed-kinetic chain exercises are also a recommended method to prevent the development of collateral knee instability, which occurs to be a risk factor of Pes Anserine bursitis.
- Some patients receive an injection which consists of a solution of anesthetic and steroid. Afterward, a physiotherapist will give a hamstring stretching program and a concurrent closed-chain quadriceps strengthening program that has to repeated several times a day. This will result in less pain at about 6-8 weeks.

- Kinesiotaping is more effective than naproxen or physical therapy in the reduction of pain and swelling.
Complications
Pes anserine bursitis complications are uncommon and mostly arise from non-adherence to therapy. These may include increased discomfort and inflammation, followed by a weakening of the tendons and muscles around the knee joint.
How to Prevent Pes Anserinus Bursitis?
Ask your doctor for at-home workout recommendations to lower your risk of pes anserinus bursitis. In many situations, these exercises can help avoid a recurrence by strengthening and stretching the muscles in your legs, knees, and belly.
Reducing weight might alleviate strain on the pes anserine bursa if you are overweight. Consult your healthcare physician prior to implementing any dietary modifications.
Prognosis
After receiving treatment for pes anserinus bursitis, the majority of people may return to work right away, particularly if they work in an office and are sedentary. Nonetheless, you might have to take a few weeks off if your profession requires a lot of physical activity. Find out from your doctor when it’s safe for you to go back to work or school.
Patient Education
Patient education focuses on helping athletes avoid reinjury and on the right procedures for getting back into the game. These include training with correct technique, strengthening your quadriceps and hamstrings, using the right shoes for the activity level and intensity, keeping a healthy weight, and gradually resuming competitive training and activity.
Conclusion
Knee pain can significantly impair your quality of life and be crippling. Fortunately, there is an effective treatment for pes anserine bursitis, especially if it is identified early. A customized treatment plan can be devised by your healthcare professional to alleviate the pain and facilitate your return to a regular lifestyle.
FAQ
How do you treat pes anserine bursitis?
Limit mobility and use ice on alternate days when the inflammation is at its worst. Every four to seven hours, give yourself a 15-minute cold massage to help with inflammation. The knee can be bandaged with an elastic bandage to either minimize edema or stop it from happening. Take care to avoid creating more friction.
Will pes anserine bursitis go away on its own?
If the underlying reason is left untreated and you keep up your workout regimen, pes anserine bursitis/tendinopathy usually does not get better on its own. See your closest sports medicine specialist if you believe you may have pes anserine tendinopathy. You can start the first course of therapy in the interim.
What happens if pes anserine bursitis is left untreated?
Untreated bursitis can worsen mobility, produce additional pain and inflammation, and eventually lead to weakening in the tendons and muscles of the legs. Your legs may start to give out during everyday activity as your quadriceps become weaker.
What are the exercises for pes anserine bursitis?
By squeezing the back of your knee all the way down to the floor, you may tighten the thigh muscles of the affected leg. Maintain a straight knee. Lift the leg that is affected up until your heel is roughly 30 centimeters off the ground, maintaining your leg straight and your thigh muscles taut. After holding for around six seconds, gently descend.
Is it OK to walk with pes anserine bursitis?
Since inflammation is typically the cause of pes bursitis, effective treatment options include rest, ice, anti-inflammatory drugs, and physical therapy exercises. Rest with Stay away of strenuous activity and extended walks, particularly on rough terrain.
How long does pes anserine take to heal?
With appropriate care, pes anserinus bursitis can recover in six to eight weeks. Certain individuals may be more susceptible to the illness, particularly those who are sports or have osteoarthritis.
Why is pes anserine bursitis so common?
Usually, overuse or persistent friction and strain on the bursa cause bursitis to develop. Athletes frequently get pes anserine bursitis, especially runners. Individuals who have osteoarthritis in their knees are likewise vulnerable.




4 Comments