Pulled Calf Muscle
What is a Pulled Calf Muscle?
A Pulled Calf Muscle, scientifically referred to as a calf muscle strain, transpires when the muscles residing in the calf region, namely the soleus and gastrocnemius muscles, undergo excessive stretching beyond their normal limits.
The lower leg plays a pivotal role in biomechanics, particularly during locomotion that demands explosive power and endurance. The calf complex emerges as a fundamental cornerstone in activities involving movement and weight-bearing. Injuries in this region reverberate across a spectrum of sports and athletic communities. Calf Muscle Strain Injuries (CMSIs), frequently observed in sports necessitating high-speed running, elevated running loads, sudden accelerations, decelerations, and fatiguing scenarios, wield a substantial impact.
Calf strains, a prevalent muscular injury, bear the risk of re-injury and protracted recovery if not duly managed. These strains often manifest in the medial head of the gastrocnemius or proximity to the musculotendinous junction. The gastrocnemius, spanning across the knee and ankle joints, stands more vulnerable to injury due to its complex structure. Injury triggers encompass abrupt bursts of acceleration and abrupt eccentric overstretching of the muscle. Addressing these issues with appropriate measures becomes paramount to ensure optimal recovery and performance continuity.
Clinically Relevant Anatomy
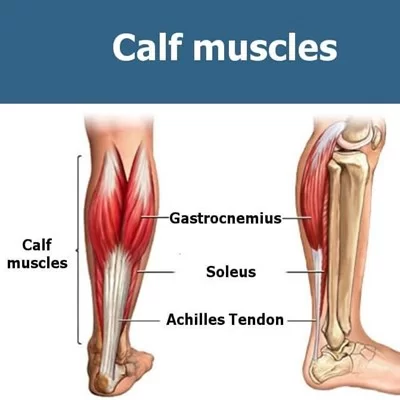
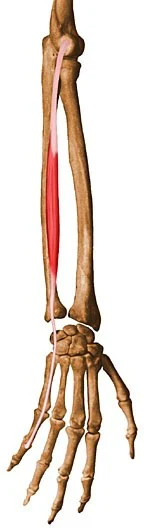
Within the calf muscle group, there are two primary components: the robust gastrocnemius and the equally vital soleus muscles. These two muscles converge towards the heel, forming a cohesive muscular structure. The gastrocnemius and soleus, with their distinct sections, collectively create substantial muscular mass.
Supplementing this muscular duo is a smaller yet significant muscle known as the plantaris. This unassuming muscle courses its way between the gastrocnemius and soleus, spanning the entirety of the lower leg. Together, these three muscles collaborate to form what is referred to as the triceps surae. However, it’s worth noting that not everyone possesses a plantaris muscle. Remarkably, approximately 100% of individuals exhibit the presence of solely the two larger muscles, underscoring the anatomical diversity within this muscle grouping.
It is composed of 3 muscles:
Gastrocnemius Muscle
Working in conjunction with the soleus muscle, the gastrocnemius plays a pivotal role in enabling plantar flexion at the ankle joint and flexion at the hinge-like knee joint. This orchestrated movement facilitates the distribution of force during the gait cycle. Despite its ability to span two joints, the gastrocnemius muscle faces limitations in exerting maximal force simultaneously on both joints. Notably, when the knee is flexed, the muscle’s potential for generating power at the ankle joint diminishes.
- Origin: The two heads are originated from the medial and lateral condyles of the femur.
- Insertion: Converging onto the Achilles tendon.
- Nerve: Tibial nerve (S1 – S2), with cutaneous supply primarily from L4, L5, and S2.
- Actions: Primary functions include plantar flexion of the foot and flexion of the knee.
- Antagonist: Counteracted by the Tibialis anterior muscle.
Soleus Muscle
Positioned beneath the gastrocnemius in the superficial posterior compartment of the lower leg, the soleus muscle assumes the responsibility of ankle joint plantar flexion and lends support to the tibia against the calcaneus, curtailing excessive forward sway.
- Origin: Arising from the fibula and the medial border of the tibia (soleal line).
- Insertion: Anchoring to the Tendo calcaneus.
- Nerve: Innervated by the Tibial nerve (L5 – S2).
- Actions: Primarily engaged in plantar flexion.
- Antagonist: Opposed by the Tibialis anterior muscle.
Plantaris Muscle
Found in the superficial compartment of the calf, the plantaris muscle is a relatively minor participant in functional terms. It coordinates with the gastrocnemius muscle to flex the knee and contributes as a plantar flexor of the ankle joint.
- Origin: Originating from the lateral supracondylar ridge of the femur, situated above the lateral head of the gastrocnemius muscle.
- Insertion: Embedding into the Tendo calcaneus, in the medial aspect, beneath the gastrocnemius muscle-tendon.
- Nerve: Innervated by the tibial nerve, stemming from the anterior rami of S1-S2.
- Actions: Dual functions encompass foot plantar flexion and knee flexion.
- Antagonist: Opposing force from the Tibialis anterior muscle.
Each of these muscles contributes its unique attributes to the complex orchestration of movement, reflecting the intricate interplay within the lower leg’s biomechanical dynamics.
Who gets pulled calf muscles?
A pulled calf muscle can affect anyone, yet it tends to be more prevalent among individuals engaged in activities characterized by frequent stop-and-go motions coupled with sudden bursts of speed. Athletes involved in sprinting, football, soccer, and tennis are particularly susceptible to experiencing strained calf muscles. Over time, this injury has been colloquially referred to as “tennis leg,” though its occurrence is not confined to tennis players alone.
What are the Causes of pulled calf muscles?
Calf muscle strains typically manifest when an individual suddenly moves or overextends their calf muscles, often after prolonged periods of standing. Swift changes in direction, sudden jumps, or abrupt halts during physical activity can trigger these strains. This injury is particularly prevalent when the toes are forcefully drawn upward toward the body, while the ankle pulls the calf muscles downward with excessive speed.
An acute calf muscle strain occurs when the muscle undergoes rapid and unexpected tearing. Such muscle tears can arise from either injuries or trauma, leading to:
- Inadequate Warm-up: Failing to adequately warm up before engaging in physical activity.
- Lack of Flexibility: Insufficient flexibility within the muscles.
- Poor Conditioning: Inadequate physical conditioning of the calf muscles.
- Overexertion and Fatigue: Excessive physical strain and fatigue.
- Calf Muscle Weakness: Underlying weakness in the calf muscles.
- Calf muscle tightness: Tight muscles increase the risk of injury.
Instances of Acute Calf Muscle Strain: Slip, sudden jumping, rapid running, lifting or throwing heavy objects, performing awkward lifts.
Chronic Calf Muscle Strain: Activities like rowing, tennis, golf, or baseball, combined with poor posture. Prolonged periods of holding the back or neck in an uncomfortable position, such as after a desk job.
Overuse Syndrome: Engaging in repetitive movements, whether at work or during activities like sports, can contribute to overuse strain.
Importance of Stretching and Warm-up: Contrary to not stretching or warming up before exercise, gradually stretching before activity can reduce the stress exerted on muscles.
Flexibility Matters: Insufficient flexibility results in tighter calf muscles and fibers, rendering them more susceptible to strains. Enhancing flexibility becomes crucial in minimizing strain risk.
Risk factors for pulled calf muscles include
- Age: Individuals above the age of 40 might exhibit a heightened susceptibility to experiencing strains during physical activities.
- Gender: Notably, men tend to be more predisposed to calf muscle injuries.
- Inadequate Conditioning: Prioritizing warming up and stretching before engaging in physical activities, as well as proactively conditioning muscles before the onset of a sports season, is of paramount importance.
- Muscle Characteristics: Those with taut or abbreviated calf muscles inherently carry an elevated risk of encountering calf strains.
Symptoms of Pulled Calf Muscle
Distinguishing between different types of muscle strains within the intricate calf complex is imperative for crafting precise prognoses, formulating effective treatment plans, and preempting the recurrence of injuries.
Among calf strains, the medial head of the gastrocnemius is the most frequent site of occurrence. A sudden sharp pain envelops the calf, often accompanied by an audible or tactile “pop” in the posterior calf’s medial region. Individuals may liken the sensation to a kick in the back of their leg. Substantial pain and swelling typically manifest within the subsequent 24 hours. This strain, often dubbed “tennis leg,” garnered its name from the classic scenario involving a midlife tennis player experiencing this abrupt injury while extending their knee.
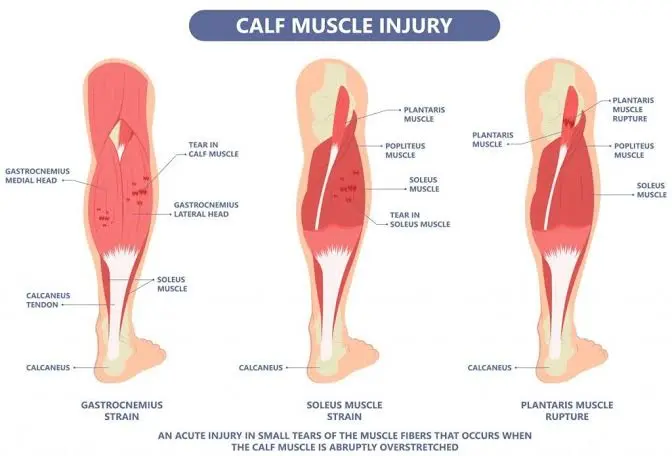
Gastrocnemius Strain
The gastrocnemius muscle is predisposed to strains due to its spanning of two joints (knee and ankle) and its abundance of type II fast-twitch muscle fibers. A tear in the medial head of the gastrocnemius muscle originates from an eccentric pressure applied to the muscle when the knee is outstretched & the ankle is dorsiflexed. Attempted contraction of the already stretched muscle leads to its tear.
Symptoms of a gastrocnemius strain encompass an abrupt sharp pain or a tearing sensation in the lower leg’s back, often localized at the medial belly of the gastrocnemius or the musculotendinous junction. Objective evaluation reveals tenderness upon palpation at the injury site, swelling, and possibly bruising within hours or days. Muscle stretching triggers pain, as does resistance during plantar flexion.
Soleus Strain
Soleus muscle strains occur with knee flexion. Proximal medial musculotendinous junction strains represent the most prevalent soleus injuries. Unlike the gastrocnemius, the soleus holds a lower risk for injury. Its span is limited to the ankle, comprising predominantly type I slow-twitch muscle fibers. Soleus strains often present with less dramatic clinical signs, exhibiting a more subacute course. Frequently occurring in middle-aged, less conditioned, or physically active individuals, the presentation mirrors that of gastrocnemius strain, albeit with slightly more distal and deeper pain sensation.
Subjective pain during calf muscle activation and Achilles tendon pressure application, around 4 cm above its insertion point on the heel bone or higher in the calf muscle, characterizes soleus strains. Aggravation of pain upon tendon stretching and walking on tiptoes may occur.
Plantaris Strains
Although the plantaris muscle traverses both the knee and ankle joints, it is often deemed vestigial and rarely implicated in calf strains. Plantaris rupture may transpire at the myotendinous junction, possibly accompanied by a hematoma or partial gastrocnemius or soleus tear. Clinical presentations of plantaris injuries mirror those of gastrocnemius and soleus strains.
The extent of the injury dictates whether individuals can continue exercising, albeit with some discomfort, or face more severe limitations, including an inability to walk due to intense pain. A nuanced grasp of these strains is vital for precise diagnosis and effective management within the diverse spectrum of calf muscle injuries.
Grading of a Pulled Calf muscle
Muscle strains are categorized into three grades, ranging from I to III, with grade III signifying the most severe level of injury. The appropriate course of treatment and rehabilitation strategies are tailored by the specific severity grade of the muscle strain, allowing for targeted and effective recovery approaches.
| Grade | Symptoms | Signs | Intermediate duration to return to routine |
|---|---|---|---|
| I | Sharp pain at the time of activity/after activity May have a sense of tightness May be capable to restart the movement, without pain/with mild ache Post-activity tightness and/or aching | Pain on unilateral calf raise/hop | 10 – 12 days |
| II | Strong pain at the moment of movement in the calf muscle Incapable to continue the movement Important pain with walking later May have swelling in the muscle Mild to moderate bruising may be present | Pain with active plantarflexion of the foot Pain & weakness with resisted plantarflexion Defeat of dorsiflexion Bilateral calf raise ache | 16 – 21 days |
| III | Intense & rapid pain in the calf, usually at the musculotendinous connection Incapable to resume the movement May present with significant bruising & swelling within hours of damage | Incapability to tighten the calf muscle May have a noticeable deficiency Thomson’s test positive | 6 months after surgery |
Differential Diagnosis
- Medial Tibial Stress Syndrome (Shin Splints)
- Achilles Tendinopathy
- Plantar Fasciopathy
- Muscle Strains and Joint Sprains Due to Limited Ankle Range of Motion (ROM)
- Additionally, other lower leg injuries that share comparable symptoms and treatment modalities with calf strains are explored below.
- Chronic Exertional Compartment Syndrome (CECS): CECS begins with mild pain during training sessions, often subsiding afterward. Progressively, pain emerges earlier, intensifying and prolonging, ultimately necessitating activity cessation. Symptoms encompass cramps, paraesthesia, numbness, and weakness in the lower leg. CECS arises from heightened intramuscular blood flow during exercise, leading to increased compartmental pressure, capillary compression, and ischemia development.
- Popliteal Artery Entrapment Syndrome (PAES): This syndrome involves an anomalous relationship between the popliteal artery and surrounding myofascial structures. Functional PAES results from muscle contraction, particularly active plantarflexion of the ankle, which compresses the artery between the muscle and underlying bone.
- Baker’s Cyst: An atypical accumulation of synovial fluid within the knee’s posterior aspect, creating a cyst. This cyst is linked to conditions affecting the knee joint, such as arthritis or meniscal injuries.
Diagnosis and tests
In certain cases, the necessity for imaging studies arises to ascertain the presence of partial or complete tears within the calf muscles. These examinations serve the dual purpose of eliminating other potential contributors to lower leg pain, including conditions like Achilles tendon ruptures or deep vein thrombosis (DVT).
Utilizing ultrasound, healthcare professionals can meticulously scrutinize the calf muscles for indications of tears or the accumulation of fluid within their vicinity.
Employing the capabilities of MRI scans, the assessment extends to identifying potential blood clot formations, detecting muscle tears, and unveiling the presence of internal bleeding. The integration of such advanced imaging techniques not only aids in accurate diagnosis but also guides the formulation of appropriate treatment strategies tailored to the specific nature of the injury.
Assessment
Subjective Assessment
History coupled with Associated Symptoms:
Mechanism of Injury:
- Analyzing the inciting trauma: pinpointing the size and magnitude of the force causing injury.
- Investigating recurrent trauma, especially those linked to faulty posture-related injuries.
Objective Assessment
Observation of the Foot and Ankle in Standing and Supine Positions:
Ankle Active Range of Motion (AROM):
Ankle Passive Range of Motion (PROM):
Repetition of symptoms on calf palpation:
Strength Testing Involving Resistance of the Foot and Ankle Complex:
Thompson Test: A pivotal maneuver to exclude the possibility of an Achilles tendon rupture.
Knee Active Range of Motion (AROM) and Resisted Testing:
Imaging:
- Ultrasound (US) emerges as the gold standard in diagnostic evaluation. It excels in assessing the muscular lesion’s degree and scope, while simultaneously excluding other potential pathologies such as ruptured Baker’s cyst and deep vein thrombosis.
Calf Muscle Tear and its Association with Sports:
Calf muscle tears frequently materialize in sports demanding rapid acceleration and agile changes in direction, a paradigmatic example being sports like running, volleyball, and tennis. The grading of muscle strains spans from I to III, reflecting their severity. Recovery duration correlates with the strain’s magnitude.
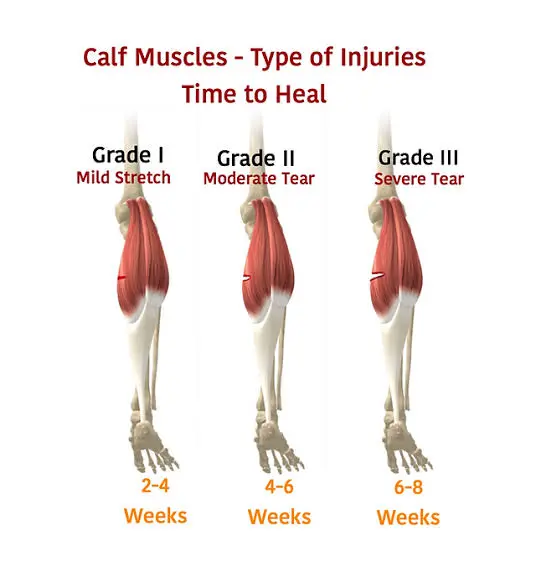
- Grade I: Mild Injury (First-degree): A common, relatively minor injury characterized by sharp pain during injury or activity. Minimal strength and range of motion loss, with muscle fiber disruption under 10%. Anticipated return to sport within 1 to 3 weeks.
- Grade II: Moderate Injury (Second-degree): Partial muscle tear necessitating cessation of activity. Notable strength and range of motion reduction accompanied by pronounced pain, swelling, and often bruising. Muscle fiber disruption ranges from 10 to 50%. Recovery typically spans 3 to 6 weeks for full activity resumption.
- Grade III: Severe Injury (Third-degree): Complete muscle rupture, often accompanied by a hematoma. Symptoms include pain, swelling, tenderness, and bruising. Recovery is individualized, potentially requiring months before a full return to activity is feasible.
- Rupture and Fluid Collection: Rupture is often associated with fluid accumulation between the soleus muscle and the medial head of the gastrocnemius. This occurrence can transpire with or without hemorrhage. The extent of the lesion is informed by fluid collection measurements. Partial or complete rupture classification hinges on the distance between the two muscles. Axial US scans prove most advantageous in distinguishing between these rupture types, offering a comprehensive visualization of the entire muscle belly within a single image.
Treatment for Pulled Calf Muscle
Calf strains rarely necessitate surgical intervention, except in cases of complete rupture.
Conservative Management
- Soft Tissue Injury Management
- Steroid Injections
- Physiotherapy
Swift removal of a hematoma, if present, is crucial to prevent complications like myositis ossificans.
In instances of more severe injury, the temporary utilization of a heel pad can aid in shortening the calf muscle, thereby alleviating tension during the healing process. Implementing heel pads in both shoes can maintain gait balance and mitigate imbalances.
Soft Tissue Injury Management
For immediate relief, the RICE Principle can be employed:
- Rest: While avoiding pain-inducing activities, it’s advisable not to abstain from all physical activity entirely.
- Ice: Ice serves as an effective method to alleviate pain and reduce swelling. Application of an ice pack (ensuring coverage with a light, absorbent towel to prevent frostbite) for 15-20 minutes every 2 to 3 hours during the initial 24 to 48 hours post-injury is recommended.
- Compression: Wrapping the injured area aids in swelling prevention. Employ an elastic medical bandage, ensuring snugness without excessive tightness to avoid interrupting blood flow. If the bandage causes the skin to turn blue, feel cold, numb, or tingly, loosening it is crucial. Prolonged symptoms warrant immediate medical attention.
- Elevation: Raising the leg above heart level, especially during nighttime, capitalizes on gravity to facilitate swelling reduction.
Physiotherapy
Physiotherapy Treatment Objectives:
- Alleviate Calf Muscle Pain
- Reduce Muscle Swelling
- Enhance Calf Muscle Strength
- Restore the Patient’s Confidence
- Reestablish Full Functional Activities
- Promote Complete Ligament and Joint Mobility
The primary approach to calf strain treatment revolves around rest and affording sufficient healing time, with surgery reserved for severe cases.
Conservative treatment encompasses gradual passive stretching, transitioning from isometric to concentric exercises. In advanced stages, the inclusion of massage and electrotherapy is plausible.
Initial Treatment Focus:
- Contain Bleeding
- Alleviate Pain
- Prevent Complications
Prompt initiation of soft tissue injury management protocols is vital, employing the PEACE and LOVE principles.
Various physiotherapy modalities can be adopted, including the application of tape or compressive wraps alongside leg elevation when feasible.
Careful control of NSAID use is crucial if significant bleeding occurred, as they possess anti-platelet effects that might exacerbate bleeding. Premature heat and massage applications should be avoided for the same reason.
Gentle, pain-free passive stretching exercises sustain plantar flexor range of motion. In later stages, once inflammation subsides, the combination of superficial heat and low-load static stretches enhances muscle flexibility.
Isotonic exercises for antagonistic muscles like the tibialis anterior and peroneal, as well as gentle exercises for the injured muscle, are recommended. Early days post-injury, controlled movements within pain thresholds stimulate healing.
Opting for shoes with low heels encourages improved heel-toe gait.
Transitioning from passive to active stretches, initially with a flexed knee (soleus) and then with a straightened knee (gastrocnemius), is indicated when calf muscles can be fully extended pain-free.
Methodical loading and strengthening exercises for the calf muscles are vital for a full recovery. Initiation of loading exercises sooner accelerates recovery.
Before complete reintegration into sports, a gradual return to sport-specific plyometric exercises is advisable.
Despite early and appropriate treatment, strains can sometimes lead to persistent pain. Successful treatment outcomes entail resolution of pain, restoration of full calf muscle extension, normalization of strength, regaining of normal knee and ankle range of motion, and vanishing of excessive tenderness.
Electrotherapy:
The initiation of physiotherapy rehabilitation can be undertaken 48 hours following the injury. During the initial days, incorporating electric modalities proves beneficial to mitigate swelling and alleviate pain.
Electric Modalities:
- Ultrasound: Ultrasound is harnessed to stimulate tissue healing, enhance blood circulation, improve mobility, and reduce swelling. Its therapeutic potential aids in expediting the recovery process.
- Cryotherapy: To counter inflammation and swelling, the application of cryotherapy in the form of ice packs or cold water baths is effective. Consistent cold application multiple times a day for 15-30 minute intervals is recommended to curtail these symptoms.
- Transcutaneous Electrical Nerve Stimulation (TENS): Transcutaneous electrical nerve stimulation (TENS) holds promise in diminishing pain and mitigating muscle spasms, offering an additional avenue for managing the aftermath of the injury.
Rehabilitation Exercises for a Pulled Calf Muscle:
Phase 1: First Week After Injury
- Application of ice, 3 times daily.
- Employ compression.
- Isometric exercise: Heel press.
Phase 2: Second and Third Weeks After Injury
- Ice application for 15-20 minutes post-exercise.
- Initiate active Range of Motion (ROM) exercises.
- Avoid activities causing pain.
- Range of motion exercises:
- Knee flexion exercise.
- Knee extension.
- Plantar flexion.
- Dorsiflexion.
- Gentle calf resisted exercise.
- Stretching exercises.
Phase 3: Three to Four Weeks After Injury
- Gentle strengthening exercises:
- Knee flexion.
- Knee extension.
- Plantar flexion.
- Dorsiflexion.
- Progress to pain-free calf stretching:
Stretching Exercises for Calf Muscle:
1. Towel Stretch:

- Sit on a firm surface, extending one leg.
- Curl a towel near the toes & the foot, then drag the towel towards the body while holding the knee straightforwardly.
- Maintain this position for 15 to 30 seconds before relaxing. Repeat 3 times.
2. Seated Heel Raises:

- Start with a sitting position with both feet on the floor.
- Raise your heels off the floor by pressing through the toes.
- Hold this position for ten seconds. Repeat 10 times.
3. Standing Calf Stretch:
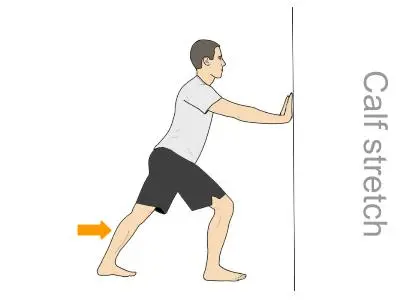
- Stand near a wall, one foot in front of the other, with a slightly bent front knee.
- Maintain your back knee straight, your heel on the floor, & tilt towards the barrier.
- Feel the stretch while the calf of the back of the leg.
- Hold for 15-20 seconds. Switch legs and alternate for a total of 3 repetitions.
Strengthening Exercises for Calf Muscles:

1. Single Leg Balance:
- Stand unsupported on one leg.
- Repeat three times.
2. Resistance Band Calf Exercise:

- Attach the band to the end of your foot.
- Push down into the bar, spreading your toes & regaling the calf.
- Hold for three seconds, then slowly release. Perform 10 to 15 repetitions. Switch legs and repeat.

3. Full Squat:
- Lower your hips below your knees.
- Perform 10 to 15 repetitions.
4. Wall Jump:

- Face a wall, placing masking tape a couple of feet above your head.
- Jump with your arms raised to touch the tape.
- Focus on a spring-like movement, landing softly.
- Progress to taking off & landing on one feet.
- Perform three sets of ten jumps.
Embracing these targeted rehabilitation exercises, segmented into distinct phases, empowers a gradual yet effective recovery journey for a pulled calf muscle. The progressive nature of these exercises aids in restoring strength, flexibility, and mobility while minimizing the risk of re-injury.
Outcome Measures
- LEFS: Lower Extremity Functional Scale
- VAS: Visual Analogue Scale
- NPRS: Numeric Pain Rating Scale
- Objective Muscle Strength Testing: For accurate and objective muscle strength assessment, employing a force platform proves invaluable, particularly for isometric evaluations of the gastrocnemius and soleus muscles. The assessment methodology should consider variations like seated or standing positions. This comprehensive evaluation facilitates the determination of Maximum Force and the rate of force development, with options at 150ms or 300ms intervals, augmenting the precision of strength measurement.
Prevention
- Incorporate Daily Stretching and Strengthening: Make it a routine to engage in daily stretching and strengthening exercises, tailored to your sporting, fitness, or occupational needs. Integrate these exercises seamlessly into your broader physical activities.
- Exercise Protocol for Strain Prevention: Adhering to a structured exercise protocol significantly diminishes the risk of muscle strains. Prioritize proactive measures to safeguard your muscles.
- Prioritize Fitness over Sports Participation: Shift your perspective – aim to attain a level of fitness that enables you to partake in sports, rather than using sports as a means to achieve fitness. This mindset promotes injury prevention.
- Work Fitness into Your Occupation: Regardless of your physically demanding profession, regular exercise serves as a countermeasure against injuries. It strengthens your resilience and enhances your capacity to perform your job effectively.
- Maintain a Balanced Diet and Exercise Regimen: Strike a balance with a well-rounded diet and exercise regimen to sustain a healthy weight. Excessive weight can exert pressure on muscles, heightening the vulnerability to muscle strains.
- Pre-Activity Warm-up Routine: Before engaging in any sports or physical activity, initiate a brisk 3 to 5-minute walk. This effectively primes your muscles, elevates your heart rate, and prepares your body to optimize the subsequent exercise’s intensity.
Conclusion
Calf muscle pain commonly arises from a strain, yet alternative conditions like deep vein thrombosis, Achilles tendinopathy, or rupture can manifest with similar symptoms. The duration of healing significantly varies, contingent on the strain’s severity and the personalized treatment response.
For grade I and II strains, a progressive exercise regimen within conservative management typically yields positive results. In instances of rupture, surgical intervention becomes imperative.
Incorporating strength and conditioning exercises plays a pivotal role in the revitalization of tissues and expedites the journey back to activity.
Remember, accurate diagnosis and a tailored approach are key in ensuring an optimal recovery path and successful return to function.
FAQ
Should I stretch a pulled calf muscle?
Your calf muscle requires time to heal before any additional pressure is involved in it. Never stretch when there is still pain and swelling in your calf. Once the pain and swelling diminish, instead of stretching, a secure choice would be, to begin with a gentle range of movement (ROM) movements of your foot, ankle, & knee.
What is the quickest method to heal a pulled calf muscle?
1-3 days: Protect, rest, ice, and elevate the limb.
3-14 days: Exercises, create up movement bypassing extreme pain/strain.
14 days: Onwards, improvement exercises, be negligibly defensive.
By 8 weeks you should have replaced all your everyday movements.
How do I know if I pulled a calf muscle?
Symptoms of a pulled calf muscle can contain No calf power, including existing incapable to balance/bear weight on the damaged leg. Snapping and popping sense in your calf. Impulsive pain in the back of your inferior leg, like somebody kicked your calf muscle.
Can a pulled calf muscle heal overnight?
A pulled calf muscle directs to a strain in the two muscles at the back of your leg, the gastrocnemius & soleus. It generally takes 3 days for it to initiate feeling satisfactorily, but complete healing may take weeks.
Is a pulled calf muscle serious?
Most individuals regain completely from pulled calf muscles without any enduring injury. Consult your family doctor when you can slowly begin to do light movements again. Relying on the harshness of your wound, it may be several weeks before you can return to complete movements.
Should I massage a pulled muscle?
Massaging a pulled muscle assists to improve blood circulation to the muscle, which in turn enables to relieve of swelling & break up any scar tissue/knots in the muscle, studies have even indicated that enhanced blood circulation assists to improve muscle temperature, resulting in enhanced muscle elasticity & flexibility.



2 Comments