Scapular Fracture
Overview
Scapular fractures are uncommon and are frequently brought on by direct trauma to the side or back of the scapula.
Less than 1% of all fractures are scapular fractures, which account for 3% to 5% of shoulder girdle fractures. Because scapular fractures require high energy/torque trauma to occur, 80% to 95% of all scapular fractures occur in conjunction with other injuries such as fractures of the shoulder, collarbone, and ribs, or during injury to the head, lungs, or spinal cord. These fractures may result in impingement, rotator cuff dysfunction, malunion, nonunion, scapulothoracic dyskinesis, or other long-term consequences like severe chronic pain and altered normal function of the shoulder girdle.
High-energy trauma, such as car crashes, falls, and other high-impact traumas, can result in scapular fractures. Over 70% of scapular fractures occur as a result of motor vehicle collisions; 52% of these injuries are related to drivers, and 18% are related to pedestrians who are struck by cars. There have also been reports of electric shock and seizures brought on by pressure on the scapula. Scapular fractures that occur alone are very uncommon.
The most common cause is high-energy trauma, which explains why scapular fractures are often linked to other acute injuries. All areas of the scapula may fracture from the direct force, but the glenoid and scapular necks may fracture from the indirect force caused by the humeral head impaction into the glenoid fossa.
When a patient has a scapular fracture, their upper limbs are adducted against their bodies and kept immobile. Shoulder range of motion is restricted, especially during abduction.
Morbidity and death reports are relatively high due to the high energy required to fracture the scapula and its correlation with other injuries. On the other hand, new information indicates that scapular fractures with lower injury severity scores (ISS) do not necessarily result in an increased risk of morbidity and death. Imaging is essential for diagnosing and categorizing scapular fractures, which informs clinical judgment.
In the past, scapular fractures were treated conservatively with closed care; however, evaluation by an orthopedic trauma surgeon is now standard practice because significant displacement is linked to poor long-term outcomes and more recent advancements in operative treatment have improved functional outcomes.
Relevant Anatomy
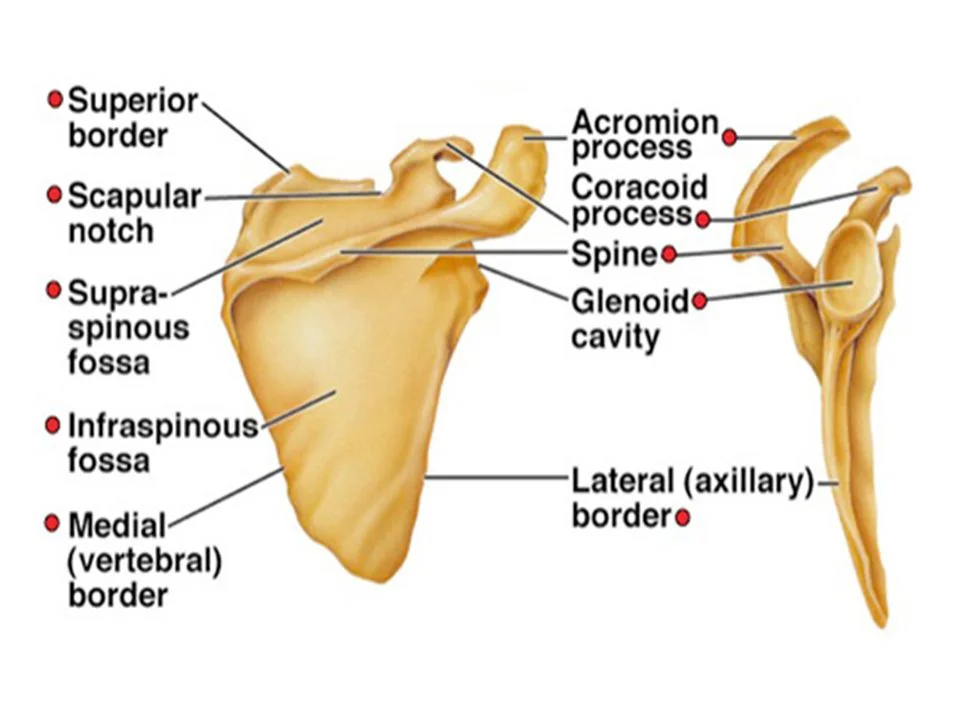
The scapula is a flat, large, triangular bone that joins the rib cage and spine to the arm bones. The humeral head, located at the top of your humerus bone, and the shoulder socket (glenoid of the scapula) make up the shoulder joint. Numerous muscles are connected to the scapula, which also moves along the chest wall to support the arm position. Vast blood vessels and nerves pass beneath the clavicle or collarbone and in front of the shoulder blade.
The acromion, which joins the clavicle or collar bone, the coracoid process, which connects to multiple muscles and ligaments, and the scapular body, which makes up the majority of the shoulder blade, are additional components of the bone.
Epidemiology
About 0.4–1% of all fractures are scapular fractures, which also make up 3% of shoulder fractures and 5% of shoulder girdle fractures, according to sources Males between the ages of 25 and 50 are more likely than females to sustain scapular fractures, which typically affect the glenoid or body.
Causes of Scapular Fracture
Up to 80–90% of scapular fractures happen as a result of high-energy trauma, which includes falls, car crashes, and other high-impact trauma. While humeral head impaction into the glenoid fossa frequently results in scapular neck and glenoid fractures, direct force can fracture any part of the scapula.
More than 70 percent of scapular fractures occur as a result of motor vehicle collisions; 52% of these injuries are related to drivers, and 18% are related to pedestrians who are struck by cars. There have also been reports of electric shock and seizures brought on by pressure on the scapula. Rarely do isolated scapular fractures occur.
- Car accidents
- Falls that cause immediate shoulder trauma
- Falls onto an elevated arm
- Blunt-force injuries from a baseball bat or hammer
- Drop in height
- Sports involving contact
- A direct strike to the shoulder
Symptoms of Scapular Fracture
- Localized discomfort while relaxing
- Severe discomfort when using the arm
- Sensitivity
- swelling in the area behind the shoulder
- severe scrapes and bruises surrounding the injured area
- Keeping the arm that was injured close to the body while the elbow and shoulder are internally rotated (90-90 degrees).
- unable to raise one’s arm
- the appearance of a deformed and flattened shoulder
- Breathing difficulties brought on by a related injury to the chest wall
- A damaged blood and nerve supply that causes numbness, tingling, or freezing in the arm
- After the shoulder’s movements, there is a popping sound and a spasm.
Classification of Scapular Fracture
A fracture to one or more scapular bones is possible:
- Scapular body (45% of patients): Three patterns of fracture occur in the scapula body: horizontal, oblique, and longitudinal.
- Scapular neck (25% of patients): The following describes three types of neck fractures: fracture of the neck inferior to the scapula spine, fracture of the surgical neck, and fracture of the anatomical neck.
- Glenoid (35 percent of cases)
- Acromion Process (8 percent of patients)
- Coracoid Process: 7 percent of patients
Types of Scapular Fracture
Intra-articular Scapular Fractures
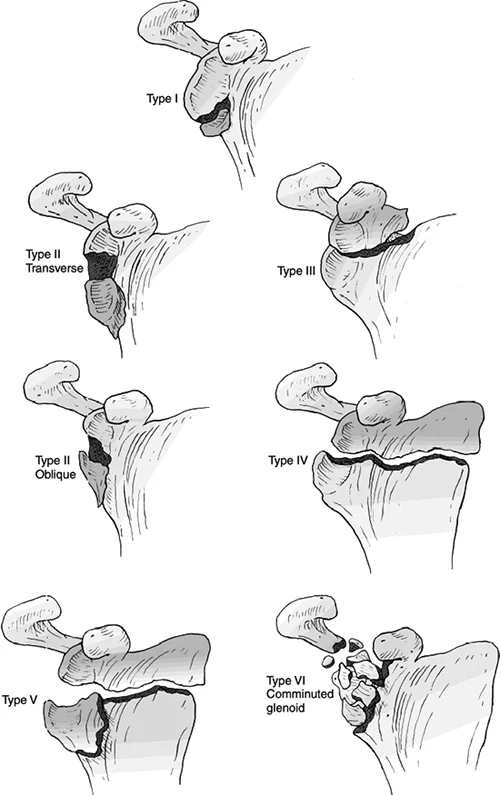
Ten to thirty percent of all scapular fractures are intraarticular fractures. Intraarticular glenoid fossa fractures were categorized by IDEBERG et al., and this classification scheme has been updated over time to define additional patterns of scapular fractures.
In high-energy car accidents, blunt trauma is the most frequent cause. While car and motorcycle crashes are the most common, scapular fractures can also occur in collisions involving bicycles, all-terrain vehicles, snowmobiles, and Jet Skis. Other common mechanisms include falling from a height or being struck by a moving vehicle while walking. The majority of open reduction and internal fixation (ORIF) procedures used to treat scapular fractures are for intraarticular glenoid fractures.
An extra mechanism linked to the intraarticular anterior glenoid fracture is an anterior shoulder dislocation. Following shoulder dislocation, which accounts for two-thirds of type 1 fractures, these IDEBERG type 1 glenoid fractures are the most common scapular fracture pattern.
Nonoperative treatment is the norm for nondisplaced intraarticular glenoid fractures. However, because the different myotendinous units providing to the scapula pull in multiple directions and cause distraction and rotational malalignment, displaced fractures require careful consideration for operative fixation.
However, the standards for surgical care are still debatable, and the surgeon’s preference as well as the patient’s comorbidities, age, hand dominance, general health, daily living activities, and degree of physical activity all play a role in whether or not ORIF is performed.
The most common objectives of ORIF for displaced intraarticular scapular fractures are to minimize joint incongruity and avoid cartilage damage, instabilities, severe discomfort, and decreased range of motion in the long run following the trauma. Surgery is indicated when there is at least 20% glenoid involvement and at least four millimeters of displacement at the articular surface; however, even in the absence of these conditions, surgery is still thought to be necessary to address instability.
Additional relative indications include open fractures, glenoid rim fractures with accompanying persistent glenohumeral instability, fractures prolonging to the medial border of the scapula with displacement, and anterior or posterior rim fractures involving more than 25% or 33% of the articular surface.
Extraarticular Scapular Fractures
Most scapular fractures are caused by extraarticular fractures involving the coracoid process, acromion process, neck, body, and spine. Nonarticular scapular fractures have traditionally been treated conservatively. ORIF for extraarticular scapular fracture has proven rare due to the belief that the shoulder girdle’s broad range of motion adequately allows for continuing activities of daily living even though scapular posttraumatic deformity.
More recently, some extraarticular fractures have called into question this belief, either on their own or in conjunction with other traumas. Although ORIF for displaced fractures has been promoted as a way to lessen persistent pain, weakness, and functional impairment, there is still debate regarding the corresponding indications of extraarticular scapular fractures.
Coracoid Process Fracture
2–13% of scapular fractures are caused by fractures of the coracoid process. The majority of the time, these fractures happen at the base with little displacement. Coracoid process fractures can occur as a result of either direct blunt trauma or indirect trauma of a dislocated shoulder, among other mechanisms.
On radiographs, a unilateral fracture of the coracoid process that occurs in conjunction with a unilateral anterior dislocation is frequently missed. Other traumatic causes include avulsion by myotendinous attachment, collapse by coracoclavicular connective tissue attachment throughout acromioclavicular joint separation, and axial loading associated with an ipsilateral clavicle fracture.
Based on their anatomical location, coracoid process fractures can be divided into five categories.
A different functioning method of classification based on the anatomic relationship between the fracture and the coracoclavicular ligament was described by Ogawa et al.
- Type I = distal tip
- Type II = midpoint
- Type III = base
- Type IV = superior body of scapula without intraarticular extension
- Type V = superior body of scapula with intraarticular extension
Type II fractures of the Ogawa coracoid process occur anterior to the coracoclavicular ligament, while type I fractures occur posterior to it. Ogawa, type I fractures are frequently occurring and prone to instability.
The most typical course of treatment for individual coracoid process fractures is conservative management. For fractures with intraarticular extension or displacement greater than 1 cm, surgical management is taken into consideration. Patients who have significant subsequent biomechanical requests, such as sportsmen and manual laborers, are additional candidates for surgical management.
If conservative treatment fails and the displaced bone fragment causes persistent irritation of the nearby soft tissues or if the fragment or fragments of the coracoid cause a barrier to the reduction of a shoulder dislocation, ORIF may also be considered.
Acromion Process Fracture
Roughly 8–16% of scapular fractures are caused by acromion process fractures. The most frequent cause is accidents involving motor vehicles. Acromion process fractures can also result from indirect trauma following shoulder dislocation or avulsion by the deltoid muscle, along with direct blunt trauma.
Fractures of the acromion process can be classified according to anatomic location concerning the acromioclavicular joint, acromial angle, or scapular spine.
A different functional approach based on the existence or lack of subacromial impingement was presented by Kuhn et al. Minimally displaced Type I fractures, significantly displaced Type II fractures without subacromial space narrowing, and significantly displaced Type III fractures with subacromial space narrowing Individuals who have Kuhn type III acromion fractures are more likely to experience rotator cuff injuries and reduced range of motion.
The most common treatment for nondisplaced acromion process fractures is conservative management, which has positive results. On the other hand, painful fracture non-union or raising fragment displacement are possible side effects of nonoperative management. Reduced range of motion, rotator cuff subacromial impingement, pain, and shoulder weakness are further long-term consequences.
Therefore, in the event of an open fracture in an acute setting, a fracture with a displacement of more than 1 cm, or a painful nonunion following conservative treatment, surgical intervention may be considered. However, there is still discussion about the best course of action, and there isn’t a single, generally accepted algorithm for treating acromion process fractures.
Scapular Neck, Body, and Spine Fracture
The most common type of scapular fracture is made up of extraarticular fractures of the neck, body, and spine. With 26–29% and 35–45% of scapular fractures occurring in the scapular neck, respectively, it is the second most common fracture site in the body. Less frequently, fractures in the spine contribute to 6–11% of scapular fractures. Although falling and being struck by a vehicle in motion are also frequent mechanisms, the cause of injury is usually violent and the consequence of a high-energies car accident.
The majority of extraarticular fractures receive conservative care. Even fractures involving substantial displacement can be successfully treated conservatively for isolated scapular body fractures. With nonoperative treatment, nondisplaced scapular neck and spine fractures have good long-term results.
Surgeons may opt for ORIF in specific cases, even though conservative management is still the cornerstone of care for the majority of displaced scapular neck and spine fractures. Since mal-union has been linked to the loss of normal shoulder biomechanics as a result of rotator cuff disorders, scapulothoracic muscular injury, muscular fibrosis, and altered muscular efficiency, the displaced scapular neck fracture has drawn the greatest attention.
Biomechanical examinations also indicate that displaced scapular neck fractures negatively impact the rigidity of the glenohumeral joint by modifying the length of the rotator cuff muscles through certain stages of movement. Patients who have significant displaced and misalignment of scapular neck fractures have also been reported to experience pain and weakness.
Radiographs or CT scans can be used to grade scapular neck displacement and rotation malalignment. For measuring the glenopolar angle and lateral border offset, the Grashey view is helpful. The glenopolar angle is an index of rotational misalignment of the glenoid about the anterior to posterior axis perpendicular to the horizontal plane of the scapula. A glenopolar angle of up to 20–22°, in isolation or conjunction with other shoulder girdle injuries, is used as an approximate recommendation for surgery to prevent long-term pain, weakness, and reduced capacity to carry out daily living tasks. The normal glenopolar angle is between 30 and 45°.
The glenopolar angle is created by drawing two lines that intersect at the highest point of the superior pole of the glenoid fossa and the inferior angle of the scapula. The first line passes through the superior and inferior points of the glenoid fossa.
The mediolateral displacement among the lateral margins of the superior and inferior scapular neck fragments that fracture defines the lateral border offset. A lateral border compensation of at least one to two centimeters is an additional relative indication of ORIF. Angulation and translation are additional measurements for scapular neck malalignment acquired on the radiographic Y view. An angular abnormality of at least 40–45° is an approximate recommendation for surgery. Angulation is a measure of rotating deformity obtained in a plane parallel to the mediolateral axis of the scapula.
By drawing two lines parallel to the inferior and superior neck fragment cortices, one can calculate the angle of attachment. The separation between the superior and inferior scapular neck fracture fragments, measured anteroposteriorly, is known as translation. The gap between the anterior cortex of the superior fragment and the anterior cortex of the inferior fragment is used to measure translation. A relative sign for surgery is a translation of at least 1 cm.
Diagnosis
Physical examination
The most frequent mechanism involves direct scapula trauma, either blunt or penetrating. The history and physical examination can provide the doctor with important details and aid in ruling out related injuries that may be fatal. This may not always be feasible in trauma circumstances, contingent on the patient’s psychological condition. It is important to conduct the physical examination of the upper extremities and shoulder in a way that permits a posterior forequarter examination.
When a patient is supine in bed with multiple injuries, this can be challenging. Asymmetry in the humeral head or shoulder displacement can be mild or severe. A comprehensive neurovascular assessment of the upper extremity should be carried out after palpation and visual inspection of the bony landmarks. In 5–13 percent of cases, brachial plexus injuries are linked to scapula fractures. Assessing motor abilities can be challenging due to the pain connected to these injuries. It is wise to perform a thorough examination of the skin to check for open fractures, as open scapula fractures necessitate prompt debridement and irrigation along with antibiotics.
Radiographs
Anterior-posterior, axillary, and lateral scapular (Y) views are appropriate radiographs to take in the event of acute scapular trauma. Acromioclavicular and glenohumeral joint injuries, as well as ipsilateral and scapular clavicle fractures, can all be diagnosed with this series of radiographs. Axillary views are especially advantageous for identifying intraarticular scapular fractures because they enable a clear view of the glenoid fossa or glenohumeral joint space. Obtaining extra axillary views improves diagnostic sensitivity for hard-to-see fractures such as coracoid process and acromion.
CT-Scan
In the event of acute trauma, standard 2D and 3D CT exams are often carried out. With CT, injuries to the bone, joint, muscle, or ligament at the shoulder girdle can be precisely characterized. It is especially useful in identifying radiographically occult injuries. Thus, CT is more accurate and reliable for the identification and arranging of scapular injuries than X-rays are; this is particularly accurate during the coracoid process, glenoid, and scapular neck fractures.
In the event of trauma, a dedicated shoulder CT scan is frequently unnecessary because modified 2D and 3D CT scans are typically obtained from the CT scan of the chest scan that was obtained upon admission. CT image modification also allows them to generate optimal 3D scapular images that match an ideal scapular Y, Anteroposterior radiographic views. Furthermore, by reducing artifacts brought about by patient positioning, body habitus, and imaging techniques, 3D CT images add value.
Differential diagnosis
The following differential diagnosis options are in the “Scapula Fracture” article.
- Pain in the abdomen in older people
- Injury of acromioclavicular
- Clavicle fracture
- Back pain
- A pneumothorax
- Dislocation of the Shoulders
Treatment of Scapular Fracture
Since more than ninety percent of scapular fractures are non-displaced, it is best to treat them non-surgically. Fractures with little to no displacement also tend to heal without complications.
Malunion may result from scapular body fractures with displacement, but because of the musculature of the scapular region, this may not even impair shoulder movement. However, if they are not properly realigned, displaced fractures in the glenoid or scapular processes do cause problems with shoulder mobility.
As a result, although the majority of scapular fractures heal without surgery, glenoid or neck fractures require the preservation of the shoulder joint range of motion.
Medical Treatment
Following surgery or an injury, pain is a normal part of the healing process. Following surgery or an injury, prescription drugs are frequently given for temporary pain relief.
A wide range of drugs, such as opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics, are available to help manage pain. To reduce the demand for opioids while simultaneously improving pain relief, doctors can suggest a mix of these drugs.
The patient and the medical team should be informed that opioids are narcotics and can become addictive, even though they help with pain relief following surgery or an injury. Opioid addiction and overdose have emerged as major global and national public health concerns. It’s crucial to take opioids exactly as prescribed by your doctor or surgeon. One should cease using opioids as soon as the patient’s pain starts to subside.
Non-Surgical Treatment
For the majority of scapula fractures, nonsurgical treatment using a shoulder immobilization sling is the most effective. While the bone mends, the sling keeps the shoulder in position. Since the fracture takes time to heal, immobilization with a sling is typically maintained for six to twelve weeks. Applying ice is advised to lessen swelling.
Surgical Treatment
Because of the unique muscular envelope of the scapula, scapular fractures heal well 90% of the time. However, in certain situations, scapular malunion can seriously affect the shoulder girdle activity, leading to chronic pain, aesthetic anomalies, impact disorder, and scapulothoracic dyskinesis.
Among the fractures that could require surgery are:
- Fractures of the glenoid articular with displaced
- Fracture with angulation of the scapula’s neck
- Fractures of the acromion process that result in contact between it and the arm bone (syndrome of impingement)
Postoperative Care:
- The operated shoulder is covered with a bandage, and the operated limb is supported by a sling.
- It is advised to apply ice to relieve pain and swelling.
- The wound needs to be kept clean and dry at all times.
- The patient must be given detailed instructions about activity and rehabilitation.
- The patient must adhere to the exercise regimen prescribed by the physiotherapist to improve shoulder strength and motion and avoid stiffness. Physical therapy is necessary for restoring shoulder function and strength.
- During the healing phase, the patient is advised to follow a healthy diet, abstain from alcohol and tobacco, and take their medications as directed.
Surgical risks and complications:
- Bleeding
- Infection
- Anesthetic reactions such as fever or nausea
- Blood clots or deep venous thrombosis
- Damage to nerves and blood vessels
- Shoulder stiffness
- Fat embolism
- Failure to heal properly
- Need for repeat surgery
Physiotherapy Management
It is important to begin physical therapy early and incorporate exercises aimed at increasing the shoulder joint range of motion. To prevent a frozen shoulder, it’s critical to begin these exercises as soon as possible. Shoulder loss of motion may result from prolonged inactivity of the shoulder joint. To reduce the chance of elbow and shoulder stiffness, it is recommended that you begin moving your shoulder during the first week following the injury. Exercises should be kept up until the full range of motion in the shoulders is restored. Moreover, it could take six months to a year.
As directed by the physical therapist, the first few weeks following an injury are used to begin initial exercises, as long as the exercises do not cause an increase in pain.
It is possible to begin exercising the unaffected joints during the first two days following the injury.
Stage 1 Activities (Weeks 0 to 3):
- Open and close your hands.
- Flexed and extend the wrist
- Flexion and extension of the elbow
- Forearm Rotation
Stage 2 Activities (Weeks 3 to 6):
- Pendular Exercises for the shoulder
- Shoulder flexion with active assistance
- Abduction of the shoulder with active assistance
- External rotation with active assistance
Stage 3 Exercises (After week 6):
- Shoulder flexion in an active forward motion
- Abduction of the shoulders actively
- Shoulder active external rotation
- Strengthening exercises with the upper extremities using weights and bands of resistance.
- Exercise for retraction of the shoulders, also known as a shoulder blade squeeze
- Push-ups against the wall
- Increasing rotator cuff strength: pull in and push out on a static rotator cuff
- Shoulder external rotation with a resistance band
Each exercise should be performed ten times, four to five times a day. It is recommended that the patient only move as far as their body will allow them to go, without using any deceptive movements to try to move further. The range of motion should not be forced; it will increase with time.
Complication
The accompanying injuries to nearby and distant osseous and soft-tissue structures are the most important complications linked to scapular fractures. There are an average of 3.9 additional injuries, most commonly affecting the ipsilateral shoulder girdle, upper extremity, lung, and chest wall.
In 15–55 percent of cases, there are pulmonary injuries such as hemopneumothorax or pulmonary contusion. In 10–40% of cases, there are cerebral contusions; in 5% of cases, there are central neurologic deficits. In 8% of cases, a splenectomy is necessary, and the death rate is 2%.
It is comparatively rare for complications to arise from the scapular fractures themselves. It is uncommon for nonunion. Depending on the specific type of fracture, malunion can manifest itself in several different ways. Malunion of a scapular body fracture typically is well tolerated, although painful scapulothoracic crepitus has been described.
Glenohumeral degenerative joint disease presenting with symptoms and instability can be caused by fractures of the glenoid cavity. Shoulder instability may arise from glenoid neck angulation fractures. Glenohumeral pain and dysfunction can result from glenoid neck fractures causing translational displacement, which can change the mechanics of the soft tissues surrounding the fracture.
Prognosis
It has been demonstrated that 86% of the time, conservatively treated non-operative fractures result in good to outstanding functional outcomes. Studies show that although just over one percent of fractures require surgery, patients who do so have very good functional outcomes.
Active and active-assisted full range of motion exercises usually take six weeks during rehabilitation; strength training starts three to four months after surgery or injury. For non-operative fractures, patients can frequently anticipate almost no functional deficits and good to excellent outcomes in the case of fractures needing surgical intervention.
FAQs
What happens if my scapular breaks?
A scapular fracture sufferer may also feel pain, as well as swelling and bruises in the upper back and shoulder. a feeling of grinding when moving the shoulder, if at all possible Being unable to lift the affected arm, and the need to hold the arm while keeping it and the shoulder still.
What is scapular fracture?
The bone behind your shoulder, between the shoulder and the spine, is called the scapula. In general, it is simple to feel. The most common cause of scapula fractures is direct trauma to the side or back.
Is a broken scapula serious?
Shoulder blade fractures should be assessed in the emergency room of a hospital because they are frequently linked to serious, possibly fatal injuries. Instantly immobilize the arm.
How long does a scapula take to heal?
It usually takes six to twelve weeks for this to heal. It’s critical to keep the shoulder moving to prevent stiffness once the fracture starts to heal. Try not to make it worse. For the first three weeks, wear the sling to give the soft tissues time to heal.
What causes a scapular fracture?
High-energy blunt trauma, like that sustained in a motorcycle or auto accident, or direct trauma involving a significant amount of force are the two main causes of scapular fractures. Of those who have broken shoulder blades, up to 80% also have associated injuries to the head, lungs, spinal cord, ribs, shoulder, and chest wall.
Can the scapula affect the shoulder?
The scapula is a vital bone for the function of the shoulder joint. Protraction, retraction, elevation, depression, upward rotation, and downward rotation are the six ways it can move the upper limbs, enabling full functional movement.
REFERENCES
- Berritto, D., Pinto, A., Russo, A., Urraro, F., Laporta, A., Belfiore, M. P., & Grassi, R. (2018, January 19). Scapular fractures: a common diagnostic pitfall. PubMed. https://doi.org/10.23750/abm.v89i1-s.7014
- Scapular Fracture. (n.d.). Physiopedia. https://www.physio-pedia.com/Scapular_Fracture
- Libby, C. (2023, July 17). Scapula Fracture. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK537312/
- Scapula Fracture (Shoulder Blade Fracture). (2021, August 8). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/scapula-fracture-shoulder-blade-fracture
- Scapula Fracture (Broken Shoulder Blade). (n.d.). Orthopaedic Trauma Association (OTA). https://ota.org/for-patients/find-info-body-part/6129#/+/0/score,date_na_dt/desc/