Semimebranous tendinitis and Physiotherapy Management
- Semimembranosus tendinopathy (SMT) is an uncommon cause of chronic knee pain. Owing to a lack of understanding of the condition, it may be under-diagnosed or inadequately treated.
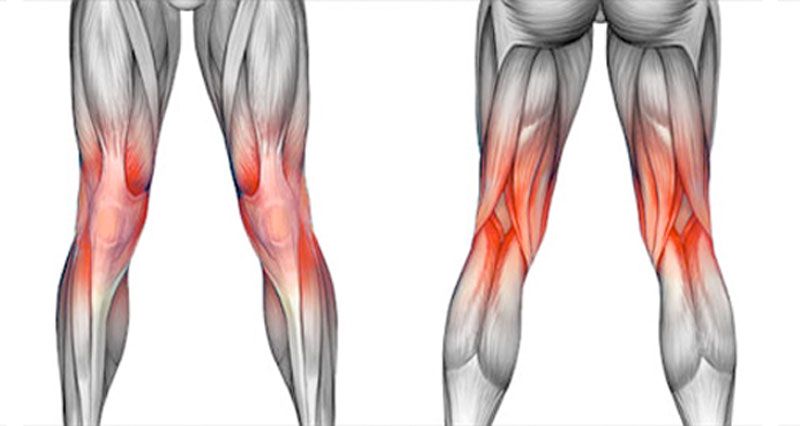
- The incidence of semimembranosus tendinopathy is unknown in the athletic population and is probably more common in older patients. The usual presentation for SMT is pain on the posteromedial side of the knee.
Anatomy related to semimebranous tendinitis
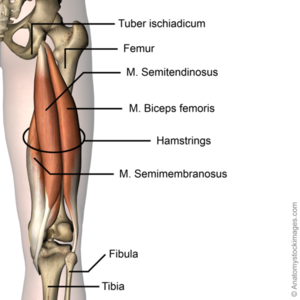
- The origin of the semimembranosus muscle is located at the lateral aspect of the ischial tuberosity, the muscle runs down the posteromedial aspect of the thigh and inserts at the posteromedial aspect of the knee.
- The muscle belly ends just above the knee joint and forms a thick rounded tendon distally, which passes medial to the medial head of the gastrocnemius but lateral to the smaller semitendinosus tendon.
- The most important function of the semimembranosus muscle is flexion and internal rotation of the knee joint. It also stabilizes the pelvis and causes extension of the hip joint.
- There is a U-shaped bursa that surrounds the distal SM tendon, separating the distal aspects of the tendon from the medial tibial plateau, MCL, and semitendinosus. Friction and repetitive eccentric tendon loading can lead to degenerative changes in the tendon and its insertions and irritation of the bursa.
Mechanism of injury
- The muscle belly ends just above the knee joint and forms a thick rounded tendon distally, which passes medial to the medial head of the gastrocnemius but lateral to the smaller semitendinosus tendon. Semimembranosus tendinopathy usually develops at the main (direct) head, at reflected insertions, or in the distal tendon.
- During repetitive knee flexion, the semimebranosus tendon is subjected to increased friction from the adjacent joint capsule, medial femoral condyle, medial tibial plateau, and semitendinosus tendon.Friction and repetitive eccentric tendon loading can lead to degenerative changes in the tendon and its insertions and irritation of the bursa.
- Common mechanisms of injury include: Stress placed on the tendon due to a sudden increase in intensity, frequency, or duration of training and the body trying to compensate for other injuries of the lower extremity (meniscus tear).
- Risk is increased by activities that involve repetitive and/or strenuous use of the knee and hip (distance running, triathlon, race walking, weightlifting, or climbing , running down hills. poor strength and flexibility, failure to warm-up properly before activity, flat feet and improper knee alignment (knock knees or bowlegged).
Etiology of
semimebranous tendinitis
- Typically caused by a primary phenomenon in endurance athletes or a secondary overuse compensatory condition from a primary knee abnormality. Other knee pathology often coexists, commonly Chondromalacia patallae and degenerative medial meniscal tears which may confuse the clinical picture and perhaps be involved in the cause.
- Elderly patients with osteoarthritis can develop semimembranosus tendinopathy in the anterior reflected tendon insertion secondary to adjacent osteophytes on the joint line. These patients also frequently suffer from concomitant pes anserine tendonitis.
- Total knee replacement components can also cause secondary semimembranosus tendinopathy. Some authors have noted a high predilection for females,but others have not. One might hypothesize that this is related to increased valgus stress and the Q angle present in women.
- Similarly, overpronation of the foot may cause increased valgus stress. Both conditions may increase friction between the medial femoral condyle and the SM tendon,but no studies have evaluated any of these variables as risk factors for semimembranosus tendinopathy.
Clinical presentation of
semimebranous tendinitis
- The presentation of semimembranosus tendinopathy can be variable but usually consists of an insidious, progressive ache in the posteromedial aspect of the knee. The pain may be severe in its acute form following a relatively sudden increase in endurance activity, such as cycling or running.
- Patients usually localize the pain at the posteromedial knee at the direct insertion, but pain may radiate proximally up the posteromedial thigh or distally to the medial calf. Symptoms increase with activities that involve significant hamstring activation- running, cycling, walking down stairs, or sudden deep knee flexion.
Diagnosis of
semimebranous tendinitis
- Tendinopathy is a syndrome of tendon pain and thickening—the diagnosis is based primarily on patient history and physical examination.Magnetic resonance imaging (MRI) and ultrasonography (US) are the methods of choice for the visualisation of the hamstring tendon complex.
- The advantage of MRI is better soft tissue contrast. It is more sensitive than US in detecting tendinopathy and peritendinous edema of the proximal hamstring tendons. The objective of imaging is to confirm the presence of hamstring tendon pathology and to assess the extent of the injury.A bone scan can also confirm diagnosis. It shows increased tracer uptake at the posteromedial aspect of the proximal tibia.
- On physical examination, there is tenderness on palpation of the semimembranosus tendon near its tibial insertion site (or sites) or slightly more proximally. Resisted flexion of the knee at 90° can make the semimembranosus tendon more prominent for easier palpation. Passive internal tibial rotation of a knee flexed at 90° may localise the pain.
- Passive deep flexion of the knee may also exacerbate the pain as the affected tendon and/or insertion becomes impinged by adjacent structures. The hip, ankle, and foot morphology should be evaluated for biomechanical features that can predispose to semimembranosus tendon overuse.
Conservative management of
semimebranous tendinitis
- A common consensus on the best conservative management of semimembranosus tendinopathy is still lacking due to the low scientific evidence on the effectiveness of interventions being used.
- Conservatively, traditional treatment methods for semimembranosus tendinopathy are by the majority comparable to those of other tendinopathies which includes relative rest and ice for symptoms relief in the initial phase, reduction or pause of sports activity, nonsteroidal anti-inflammatory drugs (NSAIDs), soft tissue mobilization, physiotherapy, and continuous home exercise program focusing on progressive hamstring strengthening.
- The time to full recovery is normally between 1–3 months. Shockwave therapy is a safe and effective treatment for patients with chronic tendinopathy.
Physiotherapy management of
semimebranous tendinitis

- SHORT WAVE DIATHERMY: short wave diathermy is a deep heating modality that uses heat to provide pain relief, it improves the blood supply to targeted muscle, removal of waste products.
- TENS: transcutaneous electrical nerve stimulation is an electrical modality that provides pain relief by providing pain modulation.TENS closes the gate mechanism at the anterior grey horn in the spinal cord. also stimulates the endogenous opioid system which prevents the release of substance p at the anterior grey horn.
- Ultrasound therapy: UltraSound is therapeutic modalities that generate ultrasound causes deep heat, provide micro-massage to soft tissue, increase flexibility, promote healing of tissue as well as improve localized blood supply to the area. and ultimately pain relief.

- IFT: Interferential current therapy produces a low-frequency effect at targeted tissue, it inhibits transmission of pain impulses, stimulates the endogenous opioid system, increase blood supply, relieve edema, and removes the waste products.
- ISOMETRIC EXERCISE OF HAMSTRINGS HAMSTRINGS MUSCLE GROUP
- Isometric exercises in positions without tendon compression is proposed as an effective method of loading the muscle-tendon unit as well as reduce pain. It has been reported that isometric exercises have a pain inhibitory response. It is recommended that isometric exercises should be repeated several times per day. Symptom severity and irritability are used to determine the dosage. The dosage can be adjusted to shorter/less intense contractions or vice versa based on the symptoms.
- the position of the hip should be near neutral hip flexion-extension or in minimal hip flexion (20°- 30° for a straight leg pulldowns) A favorable sign for isometric hamstring loading is an immediate reduction in pain with hamstring loading tests after exercise.
- Isometric leg curl
- Bridge holds – hip in neutral
- Isometric straight leg pulldowns
- Trunk extensions
- Isometric long leg bridging on two, progressing to one leg holds
- ISOTONIC EXERCISE OF HAMSTRINGS MUSCLE GROUP
- restore hamstring strength
- to restore hamstring muscle bulk and capacity in a functional range of movement.
- Isotonic hamstring loading may be started when there is minimal or no pain during hamstring loading in early ranges of hip flexion. Although eccentric exercises are widely accepted as the treatment of choice for tendinopathies, there is not sufficient evidence for isolating the eccentric component.
- Therefore, Heavy Slow Resistance training (HSR) is advocated. Heavy Slow Resistance training includes eccentric and concentric elements. It has also been shown to compare favorably with isolated eccentric loading in tendinopathy rehabilitation.
- With HSR, the aim is to perform a slow fatiguing resisted isotonic exercise. Commence with 15 RM (the maximum load that can be lifted 15 times in a single set) and progress to 8 RM. Perform 3-4 sets every second/other days Hold contractions for 3 seconds for each phase of the exercise (concentric and eccentric).
- Minimize loaded hip flexion in the early stages. This is advised to protect the enthesis against too much compression. It is important to concentrate on single-leg work to address asymmetrical strength loss.
- Continue with stage 1 isometric exercises on the “off” days. This will help with symptom (pain) management, especially if there are still symptoms present.
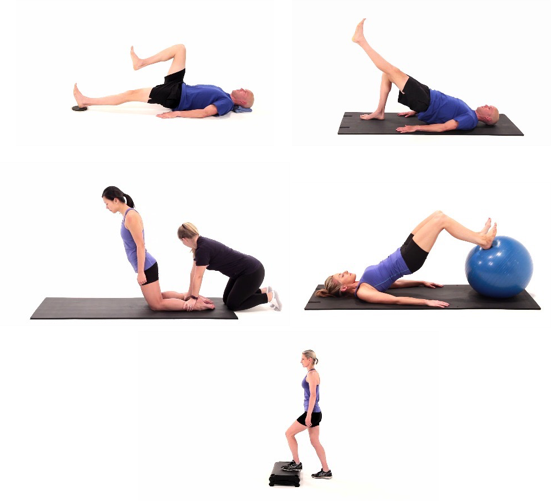
- APPROPRIATE EXERCISES FOR STAGE 2
- Single leg bridge
- prone hip extension
- prone leg curl
- Nordic hamstring exercise
- Bridging progressions
- Supine leg curler