Osgood Schlatter’s Disease and Physiotherapy Management
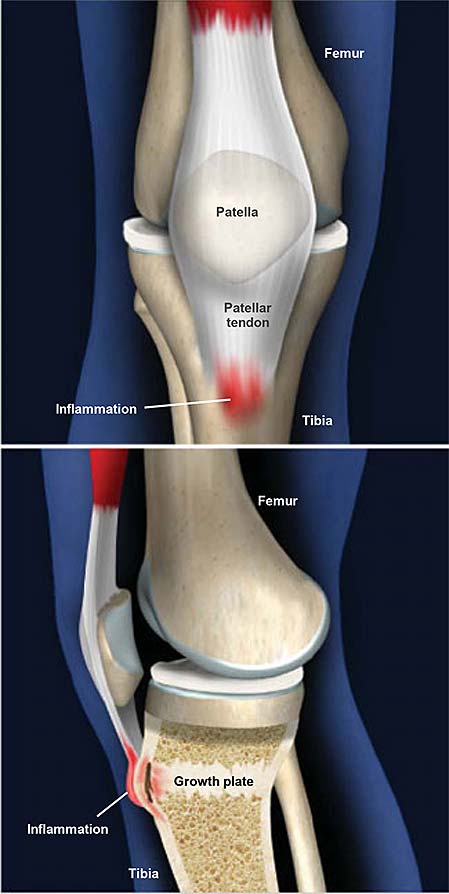
- Osgood Schlatter’s Disease is a tibial tuberosity apophysitis, which is the medical name for inflamed bone at the site of the tibial tuberosity growth plate, in children.
- Osgood Schlatter’s disease is an inflammation of the bone at the top of the tibia (shin bone), where the tendon from the patella (kneecap) attaches. It is an overuse knee injury rather than a traumatic injury.
- While Osgood Schlatter’s disease is relatively uncommon, it is a quite debilitating knee injury that occurs in young active children/adolescents
- Osgood-Schlatter’s disease is a traction apophysitis at the level of the tibial tubercle due to repetitive strain on the secondary ossification center of the tibial tuberosity.
- The repetitive strain is from the strong pull of the quadriceps muscle produced during sporting activities. The tibial tuberosity avulsion may occur in the ossification phase or the ossified phase of the secondary ossification center.
- Once the bone or cartilage is pulled away it continues to grow, ossify and enlarge. The intervening area may become fibrous, creating a separate persistent ossicle, or may show a complete bony union with some enlargement of the tibial tuberosity.
- It occurs more often in boys. These traction apophysitis are probably one of the most encountered overuse injuries in children and adolescents.
Anatomy related to Osgood Schlatter’s Disease
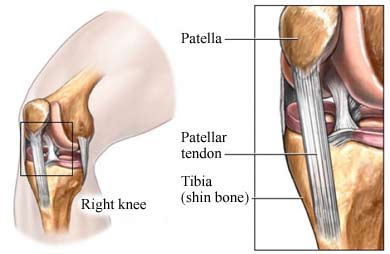
- The tibia tubercle (the tuberosity of the tibia) is a large oblong elevation on the proximal anterior aspect of the tibia, just distal to the anterior surfaces of the medial and lateral tibial condyles.
- It gives attachment to the patellar ligament or patellar tendon. The patellar tendon attaches to the tibial tuberosity inferior to the patella.
- Stress at this musculotendinous junction can cause pain and swelling. The pain felt by the patient is mostly unilateral, but often it is bilateral.
- The Osgood-Schlatter disease is localized at the tibial tubercle, distal and anterior to the knee.
Causes of Osgood Schlatter’s Disease
- Children and adolescents have growth zones in both the femur and the tibia and an apophysis (cartilage bone/cartilaginous material) at the tibial tuberosity.
- This cartilage (the flexible connective tissue that often can be found between two bones), like bones, muscles, and tendons, also has a growing capacity. But during the adolescent growth spurt, bones and cartilage grow much faster than muscles and tendons.
- The slower elongation of the musculotendinous extensor apparatus of the knee (m.quadriceps) inflicts very strong forces on the small site of the insertion of the patellar tendon to the tibial tuberosity. These forces can cause microemulsions of the tibial tuberosity.
- The cartilage of the tibial tuberosity (the anterior portion of the developing ossification center of the tibial tuberosity) can resist forces but not as bone and when the child or the adolescent does some physical activities the forces at the patellar tendon and tibial tuberosity increases, which causes pain, irritation and in some cases microemulsions or avulsions fractures of the tibial tuberosity.
- The increased stress of the musculotendinous junction of the patellar tendon and tibial tuberosity can cause the tendon to pull away from the bone a little bit.
- This small amount of tearing leads to increased pain and swelling below the knee cap. The condition is worsened with activities that subject the patellar tendon to high loads such as squatting or jumping. In some cases, ossification will occur at the area of trauma leading to a bony protuberance at the tibial tuberosity.
Clinical Features of Osgood Schlatter’s Disease
- Male with Osgood-Schlatter disease
- Pain is the leading symptom in this disease and it appears and aggravates during physical activities such as running, jumping, cycling, kneeling, walking up and down the stairs, and kicking a ball(knee extension).
- In sports like basketball, volleyball, soccer, tennis, the pain increases. The clinical picture consists of pain localized to the area of the tibial tubercle. In some cases, the tubercle may be swollen and hypertrophied and there is also tightness of the quadriceps muscle.
- Characteristics such as temperature or intra-articular swelling are not relevant (rarely the tuberosity can feel warm), but swelling, tenderness, and pain of the tibial tuberosity often appears.
- Painful palpation of the tibial tuberosity.
- Pain at the tibial tuberosity that worsens with physical activity or sport.
- Increased pain at the tibial tuberosity with squatting, stairs or jumping.
- In some cases increased bony protuberance at the tibial tuberosity.
Diagnosis of Osgood Schlatter’s Disease
- diagnosis can be made through a thorough history and examination. Tenderness to palpation over the tibial tuberosity that worsens with weight-bearing squat or jumping is fairly indicative of this disease.
- Physical examination reveals pain during palpation of the tibial tubercle.
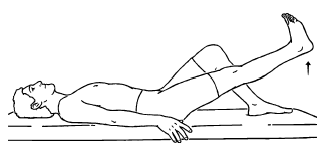
- Resisted extension of the knee from 90° flexed position will usually reproduce pain, but resisted straight leg raised test is usually painless.
- Ely’s test, which proves excessive tightness of the quadriceps femoris muscle, is positive in all cases.
- The diagnosis is based on typical clinical findings
- Radiographic examinations of both knees should always be performed, in both the anterior-posterior and lateral projections, to rule out the possibility of tumors, fractures, ruptures or infections.
- The lateral radiograph generally shows the characteristic picture of prominent tibial tubercle with irregularly ossific nucleus, or free bony fragment proximal to the tubercle. Imaging is also useful to exclude tuberosity epiphysiolysis or tumors.
- Sonographic examination can also be used. The ultrasound can be directed to demonstrate the appearance of the cartilage and bony surface, the patellar tendon, soft-tissue swelling anterior to the tibial tuberosity, and fragmentation of the tibial tuberosity
Conservative Treatment of Osgood Schlatter’s Disease
- Treatment should begin with rest, icing (RICE), activity modification, and sometimes non-steroidal anti-inflammatory drugs.
- Rest: Rest prevents the worsening of the initial injury. By placing the injured extremity to rest the first 3-7 days after the trauma, we can prevent further retraction of the ruptured muscle stumps (the formation of a large gap within the muscle), reduce the size of the hematoma, and subsequently, the size of the connective tissue scar.
- During the first few days after the injury, a short period of immobilization accelerates the formation of granulation tissue at the site of injury, but it should be noted that the duration of reduced activity (immobilization) ought to be limited only until the scar reaches sufficient strength to bear the muscle-contraction induced pulling forces without re-rupture.
- At this point, gradual mobilization should be started followed by a progressively intensified exercise program to optimize the healing by restoring the strength of the injured muscle, preventing muscle atrophy, the loss of strength, and the extensibility, all of which can follow prolonged immobilization.
- Ice or cold application: It is thought to lower intra-muscular temperature and decrease blood flow to the injured area. Regarding the use of cold on injured skeletal muscle, it has been shown that early use of cryotherapy is associated with a significantly smaller hematoma between the ruptured myofiber stumps, less inflammation, and tissue necrosis, and somewhat accelerated early regeneration.
- But according to the most recent data on the topic, icing of the injured skeletal muscle should continue for an extended period of time (6 hours) to obtain a substantial effect on limiting the hemorrhaging and tissue necrosis at the site of the injury.
- Compression: This may help decrease blood flow and accompanied by elevation will serve to decrease both blood flow and excess interstitial fluid accumulation.
- The goal is to prevent hematoma formation and interstitial edema, thus decreasing tissue ischemia. However, if the immobilization phase is prolonged, it will be detrimental to muscle regeneration.
- Cryotherapy, accompanied by compression, should be applied for 15–20 min at a time with 30–60 min between applications.
- During this time period, the quadriceps should be kept relatively immobile to allow for appropriate healing and prevent further injury.
- Elevation: The elevation of an injured extremity above the level of heart results in a decrease in hydrostatic pressure, and subsequently, reduces the accumulation of interstitial fluid, so there is less swelling at the place of injury. But it needs to be stressed that there is not a single randomized, clinical trial to validate the effectiveness of the RICE-principle in the treatment of soft tissue injury.
Surgical Treatment of Osgood Schlatter’s Disease
- Surgical procedures should be avoided until the child has grown up and the bone growth has been completed to avoid growth-plate arrest and the development of recurvatum and or valgus of the knee.
- Surgical treatment, we identified different surgical procedures such as drilling of the tibial tubercle, excision of the tibial tubercle (decreasing the size), a longitudinal incision in the patellar tendon, excision of the ununited ossicle and free cartilaginous pieces (tibial sequestrectomy), insertion of bone pegs and/or a combination of any of these procedures.
Physiotherapy Management of Osgood Schlatter’s Disease

- SHORT WAVE DIATHERMY(SWD): short wave diathermy is deep heating modality that uses heat to provide pain relief,it improves the blood supply to targeted muscles, and removal of waste products.

- TENS: trans cutaneous electrical nerve stimulation is electrical modality which provides pain relief by providing pain modulation .TENS closes gate mechanism at anterior grey horn in spinal cord. also stimulates endogenous opiod system which prevents the release of substance p at anterior grey horn.

- Exercise Therapy :
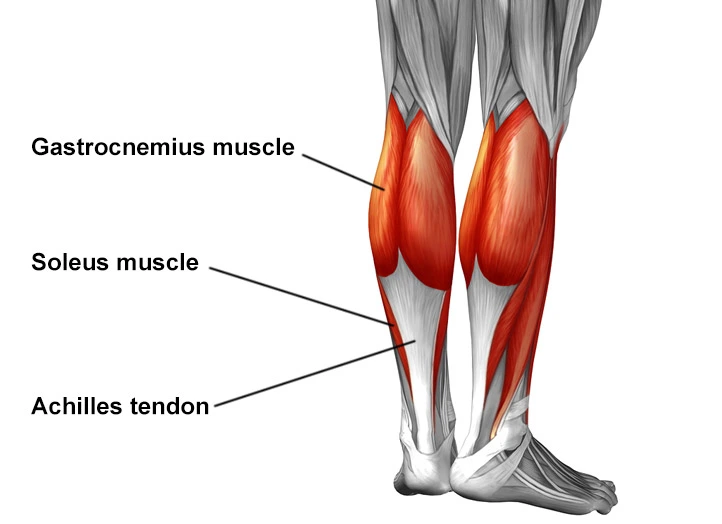
- The physiotherapist can focus on exercises to improve flexibility and strengthen the surrounding musculature. This includes the quadriceps, hamstring, iliotibial band, and gastrocnemius muscle.
- High-intensity quadriceps-strengthening exercises increase stress across the tibial tuberosity and are initially avoided. Stretching should initially be performed statically at a low intensity to prevent pain before progressing to dynamic or PNF stretching.
- A duration of at least thirty seconds with three repetitions is recommended at least once a day to increase the range of motion. Low-intensity quadriceps-strengthening exercises, such as isometric multiple-angle quadriceps exercises, are therefore instituted earlier in the conditioning program. High-intensity quadriceps exercises and hamstring stretching are introduced gradually and have been proven effective with high evidence rating.
- Shockwave: Extracorporeal Shockwave therapy is a treatment which has been discussed in the use of osgood-schlatters but due to the low value evidence recommendations cannot be made for this treatment.
- Activity Limitation: Non-operative treatment of this disease is based on the same principles that apply to all overuse injuries. Today, there is no need for total immobilization, or for totally refraining from athletic activities.
- Of vital importance is that the physician informs the parents, the coach, and the child athlete of the natural course of this disease. The child should continue his normal physical activities, to the limit that the pain allows it, so lower the intensity of the frequency of exercising (activity modification).
- Also swimming, as a secondary athletic activity, is very good during this disease (no discomfort). Also knee braces, tapes, and slip-on knee support with an infrapatellar strap or pad are recommended and may help during physical activities and can reduce pain.
- has shown that limitation of physical activity, physical load restriction, and conservative treatment are more effective than physical load restriction and activity limitation alone

- Taping: patellar tendon unloading technique
- This technique has not been researched in this patient population; however, patients report that it decreases pain. There are different usable ways to perform this technique.





7 Comments