Smith Fracture
Overview
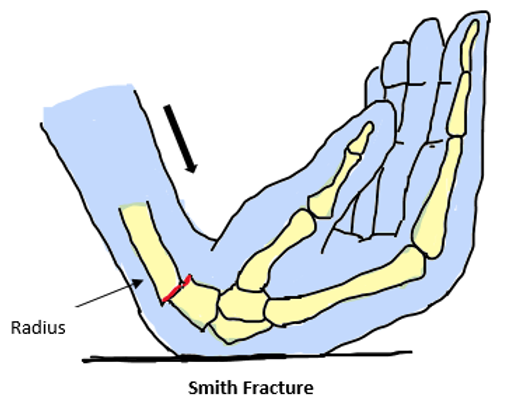
A fracture characterized by volar displacement or angulation of the distal radius is called a Smith fracture. Usually, a fall onto the hand’s dorsum with the wrist flexed causes it.
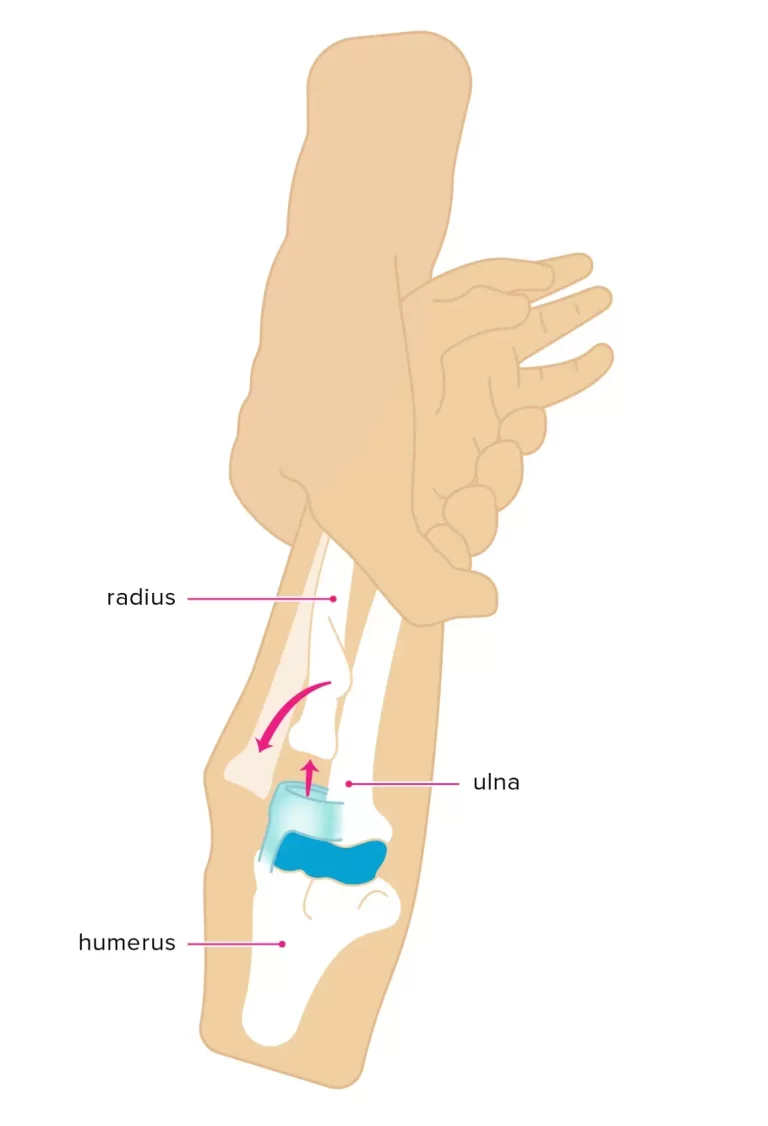
The volar, or forward, displacement fracture of the distal (i.e., away from the body, towards the fingers) end of the radius—that is, one of the two forearm bones on the lateral, or thumb side of the forearm—is known as a Smith’s fracture, also known as a reverse Colles’ fracture.
Around 5% of all radial and ulnar fractures occur in the distal radius, the most common fracture site in the upper extremities. These fractures are known as Smith’s fractures. In French literature, Smith’s fractures are called Goyrand fractures, named for the French physician Jean-Gaspard-Blaise Goyrand.
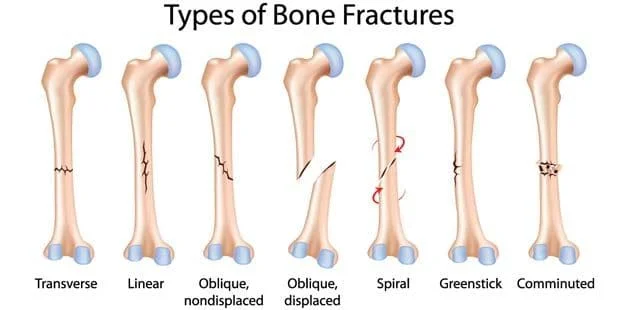
There are many distinct types of bone fractures, and the nomenclature can be bewildering. For instance, Smith fractures are sometimes described as a particular kind of distal radius fracture. One of the forearm bones, the radius points distally in the direction of your wrist.
Epidemiology
The Smith fracture is the most often fractured region in the upper extremities. More than 16% of adult fractures and 75% of forearm fractures are distal radial fractures, with over 600,000 instances occurring each year in the United States alone. In older adults, smith fractures rank second in frequency. On the other hand, 5% or so of all radial and ulnar fractures are Smith fractures.
The age group of old females and young boys has the highest frequency of Smith’s fractures. Nearly all Smith fractures occur in children who fall with high energy and in elderly people with osteoporosis who fall with low energy.
Smith fractures are the second most prevalent type of fracture in the senior population, after hip fractures. Women are six times more likely than males to get this kind of fracture between the ages of 64 and 94. The evidence points to a direct relationship between reduced bone mineral density and smith fractures brought on by low-energy trauma.
Causes
The majority of Smith’s fractures result from falls onto an extended hand or FOOSH. Volar angulation is frequently caused by the wrist flexing following falling or a direct hit to the dorsal sign.
On the other hand, it can also happen if someone trips and falls on their palm. They most often result from low-impact falls in older females with osteoporosis and high radial-impact falls in young males.
Risk Factors
Smith fractures are generally the result of trauma or accident, thus anyone can get one.
Osteoporosis is a major risk factor. Your bones are more prone to breaking if you have osteoporosis. Though women are four times more likely than men to get it, anyone can. Additionally, there is a higher risk of osteoporosis in those over 50.
Symptoms of Smith Fracture
The physical examination may show pain, edema, decreased range of motion, and a distal forearm deformity, although it is challenging to visually identify the direction of volar angulation. A malformed wrist with noticeable swelling on the volar side and the prominence of the ulna along the wrist’s dorsum are diagnostic criteria for Smith’s fracture. In addition to the distal fragment’s volar displacement, the distal radioulnar joint and the triangular fibrocartilage complex are frequently disrupted. Additionally connected may be ulnar styloid base fractures.
It is essential to assess the neurovascular condition of the affected extremity. According to research, symptoms of acute carpal tunnel syndrome from compression to the median nerve may be present in up to 15% of Smith’s fractures. Less frequently, there is compression of the ulnar and radial nerves. Smith’s Fracture also presents with acute compartment syndrome of the forearm.
Signs and Symptoms of Smith’s fracture
Smith’s fractures frequently manifest as a distal forearm deformity, albeit it can be challenging to determine the direction of displacement without radiography. People who have a Smith’s fracture typically also have wrist pain, edema, and limited range of motion.
Less frequently, compression of one or more nerves from the fractured bone results in impairment of the neurovascular system in the wrist and hand. If the neurovascular system is compromised, the person may feel tingling, numbness, or weakness in the hand or wrist regions that are innervated by the compromised nerve.
Acute carpal tunnel syndrome symptoms in the thumb, index, middle, and ring fingers can occur when the median nerve is pinched. Rarely, a person may experience radial nerve compression, which can impact the thumb and index finger digits on the radial side of the hand. Rarely, ulnar nerve compression can also happen, affecting ulnar side fingers such as the ring or pinky fingers.
Acute compartment syndrome of the forearm can also occur, presenting with unexpectedly intense pain and paresthesia, a tingling sensation that is commonly referred to as “pins and needles.”
- Pain in the wrists
- Growing
- Sensitivity
- Being unable to move your wrist pain-free
- Injuries or discolorations on the wrist region
- A lump or abnormality on your wrist that isn’t normally present
Classification Of Smith Fracture
- Type I fractures:- which make up around 85% of occurrences are extra-articular fractures through the distal radius
- Type II:– Also known as a reverse Barton fracture, intra-articular oblique fractures are less common, making up about 13% of all fractures
- Type III:– juxta-articular oblique fractures are rare, occurring in fewer than 2% of cases
Diagnosis
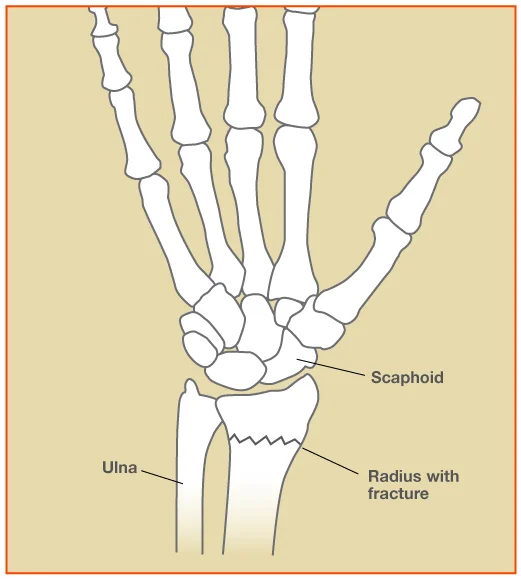
A complete medical examination of the patient, including a history of current disease, a review of medical history, and an assessment of signs and symptoms, is usually the first step in the diagnosis of a Smith’s fracture. A physical exam is then performed. AP and lateral X-rays are frequently taken after evaluation to help differentiate between Smith’s and Colle’s fractures.
To check for soft tissue injuries, further radiographs or advanced imaging techniques like a CT scan or an X-ray with an oblique view or traction may be utilized. If there are severe comminuted fractures, fractures in three or more parts, or intra-articular fracture patterns, a CT scan may also be employed for diagnosis.
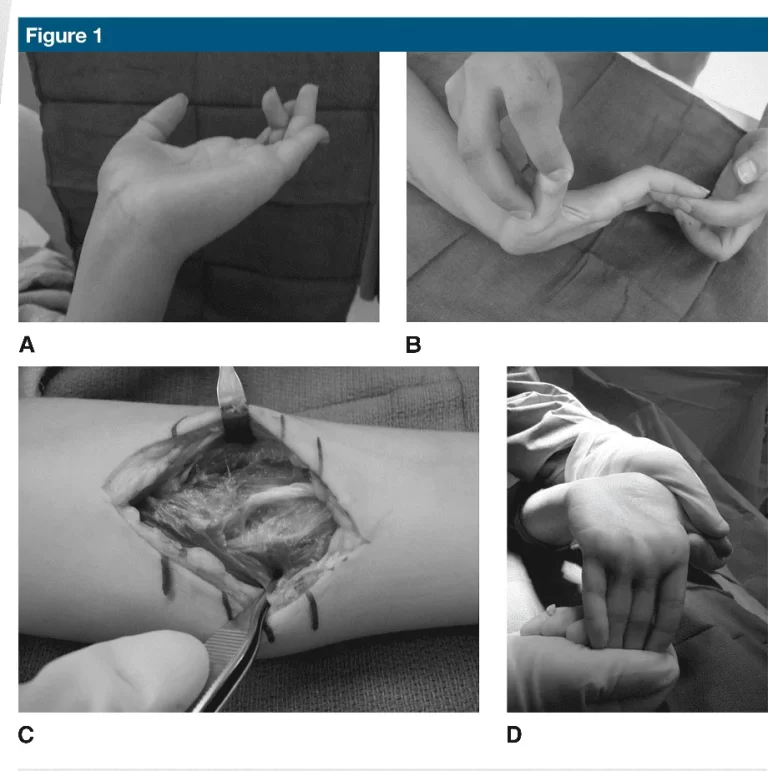
Physical Examination
A distal forearm deformity may be found on physical examination, however, it might be challenging to visualize whether the angulation is volar (Smith) or dorsal (Colles). Swelling, discomfort, and restricted range of motion are also seen on the exam. A malformed wrist with noticeable swelling on the volar side and the prominence of the ulna along the wrist’s dorsum were two of Smith’s initial diagnostic criteria.
A common occurrence is the disruption of the triangular fibrocartilage complex (TFCC) and the distal radioulnar joint (DRUJ), in addition to the volar displacement of the distal fragment. Additionally connected may be ulnar styloid base fractures.
It is critical to assess the neurovascular condition of the affected extremity. A compromise would require closed-reduction efforts to be made right away. Because of compression to the median nerve, up to 15% of these fractures may exhibit acute carpal tunnel syndrome (ACTS) symptoms. Neurological issues that are less common but exist are compression of the radial and ulnar nerves. Acute compartment syndrome of the forearm is another source of neurovascular impairment observed in Smith fractures and other distal radius fractures.

X-Rays
The fracture can be identified by AP and the wrist’s lateral radiograph. It can display the degree of angulation, displacement, and existence of a distal radial fracture with volar angulation, as well as the fracture location (extra-, juxta-, or intra-articular).
Additionally, it can provide insight into carpal malalignment, carpal fractures, and the way the radio-lunate and radio-scaphoid joints articulate. Further wrist radiographs, such as traction, oblique, and fossa lateral views, may offer vital details regarding the related soft tissue injuries.
CT-Scan
A CT scan not only helps identify the pattern of injury in cases of comminuted or intra-articular fractures, but it also aids the surgeon in formulating an operating reduction plan. In these situations, a CT scan can assist in defining and assessing the pattern of injury.
Treatment of Smith Fracture
For the smart clinician or provider, managing Smith fractures might be difficult. Naturally, restoring alignment is the ultimate aim of a successful course of treatment. These fractures frequently cannot be treated nonoperatively due to the shear fracture pattern. Even two millimeters or more of articular step-off raises the risk for the development of degenerative arthritis, so the physician must get post-reduction x-rays to ensurement of the fracture.
Selecting between conservative lost reduction and casting and surgical procedures, such as percutaneous fixation, external fixation, or open reduction internal fixation (ORIF), requires careful consideration.
Conservative Treatment
Closed reduction and splinting or casting are the methods used to treat a stable, non-displaced Smith’s fracture. Reversing the fracture deformity with longitudinal traction and placing a long arm cast with the wrist in neutral or slightly extended and the forearm in supination are the two methods used to accomplish the reduction.
Procedure sedation, hematoma block, regional nerve block, intravenous regional/Bier block, or general anesthesia can all be used for closure reduction. Weekly radiographs are recommended during the first three weeks following reduction and immobilization and before splint removal, according to AAOS clinical recommendations. For patients with distal radius fractures, Kirschner wires can also be used in conjunction with closed reduction and percutaneous pinning.
Pinning is an efficacious, low-cost treatment option for 2- and 3-part distal radius fractures with excellent long-term outcomes, however, it is not recommended in the presence of poor bone quality and multiple fragments. An infection at the pin site, pin migration, fracture settlement, and damage to the tendons, nerves, or vasculature can all result from pinning.
Surgical Treatment
The following are indications for surgical management:
- Dorsal or ventral grinding
- Engagement inside the articulation
- Unstable after reduction
- An elevation of the surface above 20 degrees
- Radial shortening more than 5 mm Articular surface step-off over 2 mm
The best course of action for treating an unstable or non-reducible fracture is open reduction internal fixation (ORIF). The American Academy of Orthopaedic Surgeons (AAOS) guidelines support volar plate internal fixation because it retains the metaphysis’s blood supply and lowers the chance of extensor tendon rupture.
Talking with the surgical team and primary care might help manage pain during the recovery phase. Studies indicate that in the six weeks after ORIF with a volar locking plate, transdermal buprenorphine and codeine-acetaminophen offered better pain control than celecoxib, citing better compliance and faster functional recovery. Nevertheless, the use of opioid analgesics outside the acute management environment should be restricted.
Ligamentotaxis is used in external fixation to ensure proper placement of the fracture fragments. At the moment, this primarily helps with the early management of an open fracture with substantial tissue loss or the stabilization of patients with polytrauma before the transfer. Maintaining adequate reduction is difficult, nevertheless, in the case of Smith fractures and the volar displacement of the distal radial fragment.
Infections of the pin track and pin loosening are among the complications. Moreover, there may be higher than average reported rates of complex regional pain syndrome (CRPS). It is thought that the carpus’s over-distraction may be involved in this.
With the development of locking plates, ORIF has emerged as the most popular treatment option. This is the ideal option for unstable or non-reducible fractures. Dorsal, volar, and fragment-specific fixation are the three primary types of internal fixation. A volar plate seems to be preferred for ORIF surgery, even though Cochrane reviews and AAOS guidelines do not favor any particular technique over another. This is because the volar plate not only lowers the chance of extensor tendon rupture but also appears to better protect the metaphysis’s blood supply.
Dorsal plating virtually has no function in the Smith fracture pattern. Apart from the volar displaced distal fragments, dorsal plating is linked to a higher incidence of extensor tendon damage and rupture. With the use of tiny plates and clips, fragment-specific fixation provides personalized construction combinations based on the requirements of each unique fracture pattern. They usually take longer to complete, entail more technical skills, and frequently ask for many approaches.
Physiotherapy Management
After four to eight weeks of immobilization, rehabilitation exercises, and bracing, stable fractures are allowed to regain normal strength and range of motion without pain. After 6 to 12 weeks of immobilization for unstable fractures, rehabilitation is frequently required to recover strength and range of motion.
While Immobilized
- Elevation and cryotherapy are effective ways to relieve pain.
- Encourage finger movement to help with lymphatic drainage and preserve mobility.
- Exercises for range of motion in the shoulders and elbows are recommended.
After the cast remove
- Heat can be a useful tool for improving the range of motion and reducing discomfort, whether it comes from a heat pack or paraffin wax. To enhance the venous return, cold therapy is alternated with it.
- Scar tissue mobilization and edema reduction are two benefits of massage.
- Exercises for the elbow, shoulder, wrist, and hands can improve strength and range of motion.
- Exercises for improving mobility include ripping paper, writing, drawing, picking up small objects, typing, combing, and basic actions like buttoning shirts. Strengthening exercises include squeezing a rubber ball in the problematic wrist, shoulder, and elbow training, and isometrics for the flexors and extensors of the wrist.
Prognosis
After a closed reduction, patients recover well; functional recovery usually occurs in six weeks. Low-quality medical data is available about the long-term effects of early postoperative mobilization. For athletes to return to sport as soon as possible, solid fixation, effective bracing, early mobilization during rehabilitation, and edema management are crucial.
Complication
Complications from a Smith fracture may include:
- Acute compartment syndrome (ACS): Your muscles may get so compressed that blood cannot reach the tissue, leading to irreversible damage to your muscles and nerves.
- Malunion:- This is the result of misaligning your damaged bones throughout the healing process.
- Carpal tunnel syndrome:- Improper healing from a fractured wrist can result in carpal tunnel syndrome, which makes the affected hand hurt, numb, and weak.
- Bone infection (osteomyelitis):- You are at higher risk of developing a bacterial infection if you have an open wrist fracture, meaning the bone breaks through the skin.
- Other internal damage:- Fractures can harm your muscles, nerves, blood vessels, tendons, ligaments, and the area surrounding your injury.
- Entrapment of the extensor pollicis longus (EPL) tendon:- In traumatizing environments, this issue is less frequent. The trapping of the malunion in both conservative and ORIF operations involves the extensor pollicis longus (EPL) tendon. The literature frequently references the EPL’s late split.
- Complex regional pain syndrome (CRPS):- reported in up to nearly 40% of fractures.
Different Diagnosis
- Colles Fracture – Extraarticular fracture of the distal radius accompanied by dorsal displacement and angle
- Barton Fracture – Intraarticular fracture of the distal radius accompanied by dorsal displacement and angle
- Reverse Barton Fracture – Fracture of the distal radius intraarticularly with volar displacement and angulation
- Die-Punch Fracture -Fracture of the articular surface accompanied by a lunate facet depression
- Chauffer’s Fracture – Fracture of the radial styloid by avulsion
- Distal Radioulnar Joint (DRUJ) disruption- Damage to the lunate facet and the sigmoid notch of the radius
- Triangular Fibrocartilage Complex (TFCC) tear – Injury to the ulnar aspect of the wrist’s cartilaginous structure
- Galeazzi Fracture -Fracture including dislocation of the DRUJ and the distal part of the radius
Prevention
Roughly speaking, wrist breaks are almost always unintentional. Make sure your workstation and house are clear of debris that could trip you or others, as falls are the leading cause of wrist fractures. Ensure that the adults in your life who are over 50 also practice appropriate fall prevention.
Summary
Smith’s fracture is a rare but important wrist joint fracture that should be considered in any accident near this joint. In 75% of the cases in this series, the diagnosis was not made.
Smith’s fractures can be divided into four different categories based on the patient’s age and X-ray appearance.
It is recommended that all of Smith’s fractures be treated with the hand in maximum supination for six weeks while it is in an above-elbow plaster cast.
All patients have some degree of handicap even with appropriate treatment, however, this is far less than in cases when the fracture is misdiagnosed, treated as a Colles’ fracture, or treated with open reduction.
FAQs
What is the difference between Smith’s and Colle’s fracture?
Whereas a Colles fracture causes dorsal displacement, bending the bone fragment towards the back of the hand, a Smith’s fracture causes volar displacement, with the shattered radius fragment projecting towards the palm side of the hand.
Which is more common Colles or Smith?
Although much less frequent than Colles fractures, Smith fractures are the second most prevalent kind of distal radius fractures.
What are the criteria for a Smith’s fracture?
A deformed wrist with significant swelling on the volar side and the prominence of the ulna along the wrist’s dorsum are diagnostic criteria for Smith’s fracture.
What is the difference between Colle’s and Smith’s mechanism?
The many mechanisms causing Colles and Smith fractures are depicted in this figure. Falling on an outstretched hand can result in a fractured collarbone. Smith fractures, on the other hand, result from landing on a flexed hand.
What are the complications of Smith’s fracture?
The main issue is wrist malunion brought on by inadequate distal radius shortening or reduction. A permanent “garden-spade deformity” may arise from this. Patients with prior Smith fractures are also more likely to develop osteoarthritis and carpal tunnel syndrome.
References
- C. (n.d.). Smith Fracture (Distal Radius Fracture): Definition & Treatment. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22329-smith-fracture
- Smith’s Fracture. (n.d.). Physiopedia. https://www.physio-pedia.com/Smith%27s_Fracture
- Schroeder, J. D., & Varacallo, M. (2022, November 25). Smith Fracture Review – StatPearls – NCBI Bookshelf. Smith Fracture Review – StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK547714/#:~:text=A%20Smith%20fracture%20is%20a,if%20not%20severe%20with%20casting.
- Editor, D. T. (2020, July 22). Smith’s Fracture : Wheeless’ Textbook of Orthopaedics. Wheeless’ Textbook of Orthopaedics. https://www.wheelessonline.com/joints/smiths-fracture/
- Smith’s Fracture – Symptoms, Causes, Treatment & Surgery. (2019, July 19). Sportsinjuryclinic.net. https://www.sportsinjuryclinic.net/sport-injuries/wrist-pain/acute-wrist-injuries/smiths-fracture