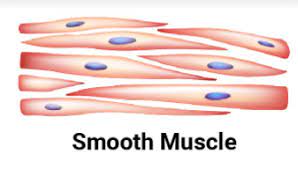
Smooth Muscle
What is a Smooth Muscle?
Along with cardiac and skeletal muscle, smooth muscle is one of the three forms of muscular tissue. It is a non-striated muscular tissue that is devoid of the other muscle kinds’ distinguishing characteristics.
It is present in many body systems, such as the reproductive, respiratory, gastrointestinal, and ocular systems, and performs the role of contracting and causing involuntary motions. The ultrastructure, mechanism of contraction, and physiological role of smooth muscle in humans will all be covered in this article.
Structure of Smooth Muscle
The cells that make up smooth muscle fibers are long, spindle-shaped, and taper at both ends. Histological identification is aided by its unique shape and the existence of a single central nucleus. Compared to the fibers of skeletal muscle, these fibers are thousands of times shorter.
Differences between striated and smooth muscle. Unlike striated muscle, t-tubules, myofibrils, and sarcomeres are lacking. Thick and thin filaments, as well as the contractile proteins myosin and actin, are present. These are ordered differently, though. Attached to a dense body are thin filaments (similar to the Z-disc of cardiac and skeletal muscle).
Unlike skeletal muscle, smooth muscle cells do not contain troponin, hence the troponin-tropomyosin complex does not control the production of cross-bridges. Rather, calmodulin also referred to as calcium-modulated protein, controls the creation of cross-bridges. The steps involved are as follows:
L-type voltage-gated calcium channels open as a result of membrane depolarization, allowing external calcium ions to enter the cell along their concentration gradient.
Myosin light chain kinase is activated by the calcium-calmodulin complex, which is formed when intracellular calcium ions bind to calmodulin.
By hydrolyzing ATP, MLC kinase phosphorylates the myosin heads, activating them.
Myosin heads can adhere to actin-binding sites and tug on the thin filaments after they have been phosphorylated.
The dense bodies, which are interconnected throughout the sarcoplasm, serve as anchors for these filaments. The entire muscle fiber contracts as a result of the thin filaments pulling on the dense bodies as they pass through the thick filaments.
Myosin light chain phosphatase facilitates the dephosphorylation of the myosin head, which is necessary for smooth muscle relaxation.
Until ATP-dependent calcium pumps aggressively move calcium ions back into the sarcoplasmic reticulum and extracellular fluid, muscle contraction can go on. Sarcoplasmic calcium concentrations are usually modest in order to preserve muscular tone and a slightly constricted muscle.
Moreover, a specific kind of cross-bridge known as a latch-bridge persists between the heads of myosin proteins and actin filaments, maintaining the connection of the thick filaments even in the absence of ATP and calcium. The smooth muscle lining the arterioles particularly needs to maintain its tone.
Smooth muscle contraction is regarded as involuntary because it is not controlled consciously. Hormones, the autonomic nervous system’s activation of neurons, and other local variables can cause smooth muscle contraction.
Smooth muscle does not develop an organized neuromuscular connection with autonomic nervous system neurons. Rather, varicosities—swellings of axons packed with neurotransmitters—are in close proximity to the sarcolemma.
Smooth muscle frequently contracts on its own and has the ability to produce action potentials in response to external stimuli thanks to pacemaker cells found in the walls of hollow organs. Depending on the neurotransmitter released, the nerve supply has the ability to either stimulate or depress the fiber’s activity.
The GI tract’s interstitial cells of Cajal are one type of these pacemaker cells.
Stretching a muscle can, in some cases, cause it to contract on its own by inducing the stress-relaxation response. As the muscles stretch, the mechanical tension causes the muscles to contract, which is quickly followed by relaxation in the stress-relaxation response. This is particularly crucial for hollow organs that constantly expand when they fill, like the stomach and bladder. As the organ shrinks and empties, this response keeps the smooth muscle surrounding it taut, preventing premature emptying and “flabbiness” in the empty organ.
The function of Smooth Muscle
Smooth muscle is distributed across many bodily systems and, depending on where it is located, performs a range of activities.
Cardiovascular system: all vascular segments in the tunica media layer, with the exception of capillaries, contain vascular smooth muscle cells. Blood vessel diameter is controlled by smooth muscle contraction and dilatation (vasoconstriction and vasodilation, respectively), which regulates blood distribution and blood pressure.
Smooth muscle layers are found in the walls of the bronchi and bronchioles of the respiratory system, which aid in controlling the amount of air that enters the lungs.
Large layers of smooth muscle line the gastrointestinal tract, aiding in the movement of food down the tube by peristalsis and the expulsion of bile from the gallbladder into the digestive system.
Urinary system: To help flow urine out of the body, layers of smooth muscle are present in the bladder and ureter walls.
Male reproductive tract: The vas deferens contain layers of smooth muscle that enable sperm to pass through the system and force glandular secretions from the prostate, seminal vesicle, and bulbourethral glands to be ejected.
Female reproductive system: During labor, oxytocin stimulates the smooth muscle that makes up the uterus’s myometrium to contract, assisting in the birth of the fetus.
Ophthalmic system: The ciliary muscle dilates and contracts to alter the lens’s size and shape, which alters how much light enters the eye.
The erector pili muscles, which are connected to the skin’s hair follicles, work together to lift hairs in reaction to temperature fluctuations.
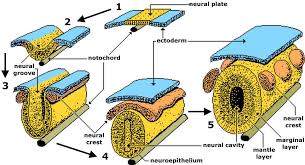
Embryology
Both neural crest and mesoderm cells give rise to smooth muscle. This is so because smooth muscle supports a wide range of bodily tissues. Neural crest cells are special because they migrate during the development of the embryo. Neural crest cells are the source of several tissues found throughout the body. In particular, neural crest cells are crucial for the control of blood arteries and the formation of smooth muscle throughout the body.
Multiple vascular smooth muscle cell lineages can give birth to vascular disorders with site-specific localization, which makes this a medically significant phenomenon. Aortic aneurysms and atherosclerosis, for instance, frequently manifest at certain arterial sites. This was previously believed to be connected to the underlying vascular structure and hemodynamics.
Nonetheless, there is mounting evidence that the location and manifestation of the disease may be influenced by the smooth muscle cell embryonic lineage. The growth of the endothelium network is also significantly influenced by the formation of smooth muscle cells.
Mural cells, also known as vascular smooth muscle cells, are crucial for the growth and stability of arteries. Mural cells are highly dependent on the regulation of blood flow, endothelial network expansion, and vessel stability. They wrap around bigger vessels.
On the other hand, nothing is known about how their developmental origins or the signaling pathway leading to vessel development influence each other. A key goal for vascular tissue engineering and therapeutic revascularization is the production of vascular smooth muscle cells.
Blood Supply and Lymphatics
Because smooth muscles are found all over the body, each region has a different blood supply and lymphatic contribution. Blood is supplied to smooth muscle in almost every artery in the body, whether it is endothelial smooth muscle found inside the artery or smooth muscle found within an organ system, such as the gastrointestinal tract’s arteries.
Understanding how smooth muscles affect blood flow becomes increasingly crucial. For instance, smooth muscle in the cardiovascular system modifies the vessel’s diameter to help control blood flow. Vascular diseases of smooth muscle, as was previously mentioned, can have devastating consequences on the body and result in serious pathology.
It has recently been demonstrated that smooth muscle development is also connected to atherosclerosis, which was previously believed to be only a consequence of hemodynamics and arterial structure. Studies have even demonstrated that pulmonary hypertension may develop as a result of persistent vascular smooth muscle activation. Asthma may arise in the lungs due to pathologic smooth muscle activation. When the smooth muscles in the airways constrict, the result is asthma. According to recent research, there may be a hereditary component to the thickening of the smooth muscle layer even prior to the development of asthma.
Nerves
The innervation of smooth muscle varies greatly depending on its function and location, much like the blood supply. The sympathetic nervous system is the main innervation of vascular smooth muscle. Vascular smooth muscle cells are contracted by alpha-1 and alpha-2 receptors, causing vasoconstriction and systemic hypertension. Although they also react to sympathetic stimulation, beta-2 receptors have a vasodilatory effect, which lowers blood pressure throughout the body.
However, smooth muscle cell contraction is also significantly influenced by parasympathetic activation. Research on the subject as early as 1925 showed how the gastrointestinal tract is affected by parasympathetic innervation. In recent times, scientists have demonstrated how the enteric, parasympathetic, and sympathetic nervous systems all function in tandem to affect and contract smooth muscle. The spinal levels T1 through L2 of the spine contribute to the sympathetic stimulation of smooth muscle.
All of these contributions end up in the sympathetic trunk, which directs autonomic nerve impulses to various bodily parts and organs. The vagus nerve, the pelvic splanchnic nerve, and the cranial nerves are the three main components of the parasympathetic nervous system. The vagus nerve, for example, innervates the gastrointestinal tract from the esophagus to the proximal portion of the large intestines and branches out to the heart, larynx, trachea, bronchi, liver, and pancreas.
Each parasympathetic nerve regulates a distinct area of the body. The autonomic nervous system is the combined name for the sympathetic and parasympathetic nervous systems. The intricate workings of the autonomic nerve system enable precise, unconscious regulation of many vital bodily processes, including blood pressure, heart rate, respiration rate, urine, and digestion.
In smooth muscle tissue, autonomic nervous system innervation ultimately results in the release of calcium. Smooth muscle contraction requires an influx of calcium. The smooth muscle cell increases its calcium content in two separate ways. L-type channels in the membrane’s caveolae allow calcium to enter the cell after depolarization, hormones, or neurotransmitters.
Through ryanodine receptors and IP3, intracellular calcium subsequently triggers the release of calcium from the sarcoplasmic reticulum (SR); this mechanism is known as calcium-induced calcium release. The sarcoplasmic reticulum’s release of calcium into smooth muscle is not physically connected to the ryanodine receptor, in contrast to skeletal muscle. After entering the cell, calcium can attach to calmodulin and cause it to change into activated calmodulin. Myosin light chain kinase (MLCK) is subsequently activated by calmodulin, and MLCK phosphorylates a regulatory light chain on myosin.
After entering the cell, calcium can attach to calmodulin and cause it to change into activated calmodulin. Myosin light chain kinase (MLCK) is subsequently activated by calmodulin, and MLCK phosphorylates a regulatory light chain on myosin. Following phosphorylation, the myosin head undergoes a conformational shift that raises myosin ATPase activity and facilitates contact between the myosin head and actin. Tension is therefore created when there is a cross-bridge cycling event.
The amount of tension produced is correlated with the cell’s calcium content. Compared to skeletal muscle, smooth muscle exhibits substantially less ATPase activity. The substantially slower cycling speed of smooth muscle is caused by this aspect.
The prolonged contraction duration, however, may result in a smooth muscle contraction with a higher force. The usage of connexins improves smooth muscle contraction even more. Connexins facilitate the passage of calcium and other chemicals to nearby smooth muscle cells, enabling intercellular communication. This process enables quick cell-to-cell communication and a smooth contraction pattern.
Steps included in smooth muscle cell contraction:
- Depolarization of membrane or hormone/neurotransmitter activation
- L-type voltage-gated calcium channels open
- Calcium-induced calcium release from the SR
- Increased intracellular calcium
- Calmodulin binds calcium
- Myosin light chain kinase activation
- Phosphorylation of myosin light chain
- Increase Myosin ATPase activity
- Myosin-P binds Actin
- Cross-bridge cycling leads to muscle tone
- Depolarization of membranes or activation of hormones and neurotransmitters
- Voltage-gated calcium channels of the L-type open
- Calcium-caused release of calcium from the SR
- elevated intracellular calcium levels
- Calcium binds to calmodulin.
- Activation of myosin light chain kinase
- Light chain phosphorylation of myosin
- Boost ATPase activity in myosin
- Myosin-P binds Actin; muscle tone is produced via cross-bridge cycling.
Smooth muscle contraction is stopped by myosin light chain dephosphorylation. Smooth muscle is phosphorylated when it is activated, in contrast to skeletal muscle. This raises the possibility of an issue because muscular relaxation cannot be achieved by merely lowering calcium levels. Rather, the enzyme myosin light chain phosphatase (MLCP) is in charge of dephosphorylating the myosin light chains, which eventually causes smooth muscle relaxation.
Muscles
Smooth muscle can be located in all the organ systems below:
Gastrointestinal tract
Cardiovascular: Blood vessels and lymphatic vessels
Renal: Urinary bladder
Genital: Male and female reproductive tracts
Respiratory tract
Integument: erector pili of the skin
Sensory: Ciliary muscle, iris of the eye
Location
Skin
| Arrector pili muscles | Situated in the dermis inserted into hair follicles below sebaceous glands causing piloerection The role of hair follicles in regulating temperature, maintaining the structure of the follicular units, and producing sebum. |
| Nipple | Smooth muscle bundles present in the areola and around lactiferous ducts For nipple erection and milk expression |
| Scrotum | Tunica dartos in subdermal layer Assists in scrotal thermoregulation |
| Vulva | In the dermis of the labia major also the smooth muscle is situated Can represent vestigial homologue to male dartos muscle |
Eye
| Iris | Also known as superior tarsal muscle; small bundles of smooth muscle within the upper eyelid adjoining the levator palpebrae superioris help keep the eyes open |
| Ciliary body | Also known as superior tarsal muscle; small bundles of smooth muscle within the upper eyelid adjoining the levator palpebrae superioris help keep the eyes open |
| The ciliary muscle helps to control the shape of the lens (accommodation) | Also known as superior tarsal muscle; small bundles of smooth muscle within the upper eyelid adjoining the levator palpebrae superioris |
| Orbit | Also known as superior tarsal muscle; small bundles of smooth muscle within the upper eyelid adjoining the levator palpebrae superioris assist put the eyes open |
Cardiovascular
| Elastic arteries | Tunica media: More elastic fibers and not so much smooth muscle relative to muscular arteries carrying blood and enduring the intense pressure of blood discharged from the heart (such as the pulmonary arteries and aorta) |
| Arteries in the muscles | Media from Tunica: Compared to elastic arteries, smooth muscle is greater and fewer elastic fibers Constrict and dilate (e.g., radial artery, femoral artery) as necessary to alter the volume of blood given. |
| Arterioles | primarily made up of smooth muscle; vital for regulating blood pressure and preserving systemic vascular resistance |
| Capillaries | The Composed of a single endothelial layer and a pericytic layer (see below) allowing for the diffusion of nutrients and oxygen |
| Venules | The Composed of a single endothelial layer and a pericytic layer (see below) allowing for the diffusion of nutrients and oxygen |
| Veins | Less smooth muscle and connective tissue than arteries making their walls thinner and allowing them to accommodate a large volume of blood at relatively low pressures |
| Capillary pericytes | Pericytes in capillaries Pericytes, which are smooth muscle cells with a lot of filaments inside of them, are crucial in maintaining tissue-specific processes including the blood-brain barrier and controlling blood flow. |
| Lymphatics | Muscular media are thin wisps present in larger lymphatics. |
| Endocardium | A primitive layer of smooth muscle is frequently seen in the endocardium; this layer is not to be mistaken for Purkinje cells or conduction system tracts. |
Lung
| Conducting airways | Smooth muscle, which is found in the walls of the airways from the trachea to the terminal bronchioles and gradually disappears farther away, controls the bronchomotor tone of the airways. The muscle may have a passive role in the stiff trachea, completing the tube’s circumference. |
| Respiratory airways | Bundles of smooth muscle can be seen at the level of the alveolar ducts, intersperse by alveolar openings, which may appear as isolated round or oblong aggregates in cross-section |
Gastrointestinal
| Muscularis mucosae | Muscularis mucosae- Between the submucosa and the mucosa, a thin muscle layer Layers: inner circular and outer longitudinal except in the esophagus where it is only longitudinal. Thickest in the distal esophagus. In the rectum, it goes into the upper transition layer of the anal canal Gives a structural foundation for the mucosa and puts the glands in a continuous movement to expel their contents. |
| Muscularis propria (externa) | Thick muscular layer between submucosa and subserosa/serosa Layers: inner circular and outer longitudinal except in the stomach where there is an extra innermost oblique layer. In the esophagus: the upper portion is entirely skeletal muscle, the middle part is a combination of skeletal and smooth, and the last part is entirely smooth Include the myenteric plexus of Auerbach and interstitial cells of Cajal responsible for peristaltic movement. Three longitudinal smooth muscle bands in the intestinal wall are called teniae coli. |
| Anal canal | The thickened extension of the intestinal wall’s circular smooth muscle is known as the internal anal sphincter. |
| Pelvic floor and perineum | Perineal smooth muscle: the rectourethralis in men and the rectovaginalis in women are considered homologous structures contributing to the stabilization of the pelvic floor. |
Biliary system
| Lacks smooth muscle except for the common bile duct (particularly the lower one-third) and cystic duct at the junction with gallbladder (also known as the spiral valve of Heister), serving to prevent overdistention or collapse of the cystic duct | Muscularis propria: loosely arranged bundles of circular, longitudinal, and oblique fibers, lying directly beneath the lamina propria (no muscularis mucosae or submucosa) |
| Extrahepatic biliary tract | A concentric ring of muscle regulates the flow of bile and pancreatic secretions into the duodenum and prevents the reflux of duodenal contents. |
| Sphincter of Oddi | A concentric ring of muscle generates the flow of bile and pancreatic secretions into the duodenum and inhibits the reflux of duodenal contents. |
Genitourinary
| Bladder | Muscularis mucosae-Smooth muscle strands that are discontinuous Muscularis propria (detrusor muscle): 3 coats with interwoven orientation, inner and outer, longitudinal and central circular, which seem to be randomly arranged Detrusor supplies micturition and permits the bladder to stretch for the storage of urine. |
| Ureter | Muscularis propria with indistinct layers |
| Renal pelvis | Muscularis propria becomes thinner along the major and minor calyces |
| Male ducts & seminal vesicles | Efferent ductules, epididymis, and vas deferens all contain smooth muscle which functions to propel sperm and fluids Massive in vas deferens (inner and outer longitudinal layers and middle circular), which supply spermatozoa from epididymis to ejaculatory duct There is also a noticeable layer of smooth muscle surrounding the seminal vesicles. |
| Penis | The primary erectile tissues of the penis, known as the corpora cavernosa, are made up of an anastomosing vascular network with smooth muscle and fibrous tissue in between. Corpus spongiosum surrounds the penile urethra with less smooth muscle than that of the cavernous As the outside temperature drops, the scrotal and penile dartos continue to envelop the penile shaft, causing the genital tissues to retract. |
| Prostate | Anterior fibromuscular stroma constitutes the anterior nonglandular portion of the prostatic surgical capsule, composed of vertically oriented smooth muscle continuous with the bladder detrusor muscle, which may play a role in maintaining urethral resistance. The prostate itself has abundant fibromuscular stroma |
| Urethra | Internal urethral sphincter: collar of smooth muscle at the neck of the bladder continuous with the detrusor muscle of the bladder This function helps in maintaining urinary continence and prevents the backward flow of semen into the bladder. |
Female reproductive
| Uterus | Smooth muscle in the corpus is more concentrated than in the cervix or lower uterine segment. This muscle distribution is in line with the cervix’s passive function during parturition. |
| Vagina | Smooth muscle musculature is continuous with that of the uterus |
| Fallopian tube | Smooth muscle is thickest in the isthmus and becomes thinner towards the fimbriated end. The remainder of the tube wall contains 2 layers of smooth muscle |
| Ovary | As the fimbriated end is approached, the thickness of smooth muscle gradually decreases from the isthmus. The remainder of the tube wall contains 2 layers of smooth muscle |
Smooth Muscle Organisation
Smooth muscle is organized in 2 different forms. These 2 types of arrangement are found in various locations and have different characteristics.
| single smooth muscle (visceral) unit | Multiunit smooth muscle | ||
| 1 | Frequency | More common | Less common |
| 2 | Do not possess gap junctions, therefore fibers are not electrically coupled. Contraction doesn’t spread between cells and is confined to the cell originally stimulated | Fiber coupling | Stimulation of muscle fibers |
| 3 | Large blood vessels, eyes, and respiratory airways | Large blood vessels, eyes, and respiratory airways | · Autonomic nerves, Hormones |
| 4 | Location | Walls of all visceral organs except the heart | Large blood vessels, eyes and respiratory airways |
| 5 | Contraction | Produces slow, steady contractions to allow substances to move through the body, For example, the food present in the gastrointestinal tract. | Produces asynchronous contractions |
Physiologic Variants
There are two varieties of smooth muscle: single-unit and multi-unit. Multiple cells linked by connexins that can be activated synchronously by a single synaptic input comprise single-unit smooth muscle. Cell-to-cell communication among clusters of isolated smooth muscle cells is facilitated by lectins. Calcium waves are produced when ions and other molecules diffuse between cells as a result of this intercellular communication.
This particular characteristic of smooth muscle in single units makes synchronous contraction possible. The way that each smooth muscle cell receives its synaptic input distinguishes multi-unit smooth muscle from single-unit smooth muscle. This enables considerably greater regulation of multi-unit smooth muscle. The ciliary muscles of the eyes, the big arteries, and the airways of the lungs all contain multi-unit smooth muscle.
Surgical Considerations
Every surgery will be affected by the general function of smooth muscle because of its regulatory effects on autonomic regulation. Keeping an eye on the patient’s vital signs throughout surgery is critical to its effectiveness, as the autonomic nervous system—which controls smooth muscle contraction—can be greatly impacted by the stresses of the process. Even changing the way smooth muscle functions can be the goal of surgery, as in the instance of a vagotomy. Peptic ulcer disease may be caused by overstimulation of the vagus nerve; vagotomy, a traditional surgical operation, tries to cure this problem by cutting the vagus nerve at the level of the stomach, hence eliminating stimulation.
Though recent improvements in medical therapy for peptic ulcer disease have made this procedure less popular, certain people may still benefit from it. Another instance is the management of specific neuroendocrine tumors, such as adrenal pheochromocytomas, which might release excess catecholamines during surgery and result in cardiovascular problems.
Understanding how alpha and beta blockades impact smooth muscle and how those alterations impact other body systems is essential for proper management. When planning and carrying out any surgery, having a thorough understanding of the role that smooth muscle contraction plays and how it affects various body systems becomes essential because of its regulatory control effects.
Clinical Significance
It is astounding to learn that something as basic as smooth muscle contraction can trigger asthma, given the significant healthcare burden associated with the condition. Smooth muscle is a vital component of the human body, present in nearly every organ system, and necessary for survival. Smooth muscle is involved in the maintenance of blood pressure and flow in the cardiovascular system, in the opening and closing of airways in the lungs, in the motility and absorption of nutrients in the gastrointestinal system, and in nearly every other organ system.
A thorough grasp of smooth muscle anatomy, physiology, function, and applications in disease is crucial for medical practitioners due to the smooth muscle’s widespread distribution throughout the body and its unique qualities.
From a functional perspective, all vital signs are preserved and are under the control of smooth muscle physiology. Smooth muscle has probably contributed to the development of the patient’s condition, whether it is a chronic illness or an immediate emergent one. Many treatments that can save lives in an urgent situation specifically target smooth muscle.
In these situations, health personnel will be able to save lives if they have a solid foundation and understanding of smooth muscle. A deeper comprehension of smooth muscle would enable medical professionals to improve patient’s quality of life.
The biopsychosocial model also includes the psycho-social aspects that are sometimes disregarded in relation to smooth muscle diseases. For instance, a patient with neurogenic bladder disease may withdraw from society in an effort to minimize the stigma attached to their illness. Healthcare professionals should be aware of the various ways that smooth muscle dysfunction will affect their patients when treating it.
As with everything in medicine, more studies will probably be done in the future to improve our knowledge of smooth muscle and how it affects disease in general. Future ramifications of the smooth muscle research being conducted today, such as the restoration of endothelium tissue, could pave the way for novel approaches to encourage revascularization.
FAQ
What role does the digestive system’s smooth muscle play?
The GI tract’s smooth muscle’s primary job is to mix and move intraluminal materials to facilitate effective meal digestion, gradual nutrient absorption, and residual evacuation.
Is multinucleated smooth muscle?
Smooth muscle cells are mononucleate cells that can be found alone, in groups or layers inside different tissues, or in rare cases, they can form distinct muscles. Contractions of smooth muscle cells are sluggish and rely on the autonomic nervous system. Mononucleate striated cells that contract quickly, rhythmically, and spontaneously are cardiac muscle cells.
Smooth muscle is found where?
Smooth muscle fibers are spindle-shaped, and found in the walls of all hollow visceral organs (such as the liver, pancreas, and intestines), with the exception of the heart. They are also controlled involuntarily. Skeletal muscle fibers are present in muscles that attach to the bone.
Which layers make up the smooth muscle?
The outside longitudinal, middle circular, and inner oblique muscles make up the three layers of smooth muscle. These muscles’ construction aids in blending and breaking down the contents into chyme, a nutritional suspension that is propelled into the duodenum.
Which terms are used to refer to smooth muscle?
Smooth muscle, also known as visceral, non-striated, or involuntary muscle, is distinct from skeletal muscle, which is striped, striated, or voluntary. Because smooth muscles are located in the interior, or visceral, organs, they are also referred to as visceral muscles.
References
- Smooth Muscle tissue – Structure – Contraction – TeachMePhysiology. (2023, July 17). TeachMePhysiology. https://teachmephysiology.com/histology/tissue-structure/muscle-histology/smooth-muscle/
- Hafen, B. B. (2023, July 17). Anatomy, smooth muscle. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK532857/
- Histology-smooth muscle. (n.d.). https://www.pathologyoutlines.com/topic/softtissuesmoothmuscle.html




9 Comments