Suboccipital Nerve
Introduction
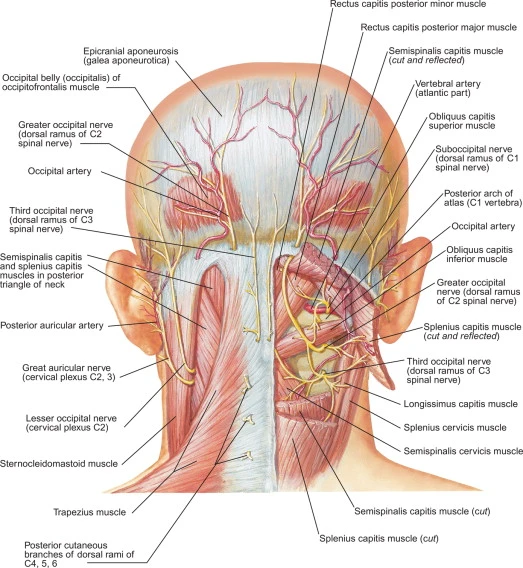
The suboccipital nerve is also referred to as the dorsal ramus of the first cervical nerve since it arises from the posterior/dorsal ramus of the first cervical spinal nerve (C1). The suboccipital nerve runs to the posterior neck region from its origin. This nerve follows the vertebral artery along its route, which is why damage to both of these structures frequently happens at the same time.
Most of the fibers of the suboccipital nerve are motor fibres. This nerve’s main job is to give the suboccipital muscle group motor innervation. These muscles include the semispinalis capitis, rectus capitis posterior major, rectus capitis posterior minor, obliquus capitis superior, and obliquus capitis inferior. These muscles cooperate to control the head and neck’s postural alignment.
Origin and direction
The first cervical nerve (C1) emerges from the vertebral canal just superior to the first cervical vertebra (atlas) and inferior to the occipital bone. The nerve then divides into the suboccipital nerve, which has a bigger dorsal ramus and a smaller ventral ramus. Because it emerges right below the occipital bone, this nerve is known as suboccipital (under occiput).
The vertebral artery and the posterior arch of the atlas were anterior to and inferior to, respectively, the suboccipital nerve courses. It penetrates the suboccipital triangle after puncturing the posterior atlantooccipital membrane. It follows the extradural segment (horizontal part) of the vertebral artery via the suboccipital triangle and concludes by releasing motor branches for the innervation of the muscles of the neck.
Innervation and branches
The nerve splits into multiple branches when it enters the suboccipital triangle, innervating both the muscles that make up the suboccipital triangle and other suboccipital muscles.
The rectus capitis posterior major muscle (superomedial border), obliquus capitis superior muscle (superolateral margin), and obliquus capitis inferior muscle (inferolateral margin) all make up the suboccipital triangle. The rectus capitis posterior minor muscle and semispinalis capitis, which make up the roof of the suboccipital triangle, are also innervated by the suboccipital nerve.
The cutaneous branch of the suboccipital nerve occasionally joins the occipital nerves in innervating the scalp.
Rectus capitis posterior Major
The bigger of the two rectus capitis muscles is the rectus capitis posterior major. It is placed next to the rectus capitis posterior minor on the lateral side.
Attachments: Inserts into the lateral portion of the inferior nuchal line of the occipital bone. gets Originates from the spinous process of the second cervical vertebrae (axis).
Head extension and rotation are the actions.
Suboccipital nerve is innervated (posterior ramus of C1).
Rectus Capitis posterior minor
The most medial suboccipital muscle is the rectus capitis posterior minor. This muscle and the dura mater, the outer membrane of the meninges, are connected by connective tissue, which may contribute to cervicogenic headaches.
Attachments: originates from the C1 vertebra’s posterior tubercle, a crude spinous process. Attaches the C1 vertebra (basic spinous process). attaches to the medial portion of the occipital bone’s inferior nuchal line.
Action -The head extension.
Innervation-Suboccipital nerve (posterior ramus of C1).
Obliquus Capitis inferior
The muscle with the most inferior positioning among the suboccipital muscles is the obliquus capitis inferior. It is the only muscle in this group that is unconnected to the skull.
Attachments: originates from the transverse process of the C1 vertebra and connects to the spinous process of the C2 vertebra.
action-Head rotation and extension
Innervation-Suboccipital nerve (posterior ramus of C1).
Obliquus Capitis superior
Attachments -Laterally in the suboccipital compartment is where you’ll find the superior obliquus capitis.
The occipital bone (between the superior and inferior nuchal lines) is where the obliquus capitis superior, which originates from the transverse process of C1, is located.
Action: The head is extended.
innervation -Suboccipital nerve is (posterior ramus of C1).
Suboccipital Triangle
Three of the suboccipital muscles surround the suboccipital triangle. It houses the vertebral artery, the suboccipital venous plexus, and the suboccipital nerve. The vertebral artery can be seen during surgery. These are its boundaries:
superomedial -Rectus capitus posterior major is .
superlateral -Obliquus capitus superior,
inferior-Obliquus capitus inferior,
Floor: The posterior arch of the C1 vertebra (atlas) and the posterior atlantooccipital membrane
Roof -Semispinalis capitus
Physiologic variants
When the origins of the C1 spinal nerve and, consequently, the suboccipital nerve are examined in cadaveric research, there are differences between people. In 80 cadaveric specimens, it was discovered that 60% of the time, dorsal rootlets coexisted with ventral rootlets, and 30% of the time, these dorsal rootlets combined to create a dorsal root ganglion. Consequently, it is surprising that in about 40% of specimens, there were no dorsal rootlets that helped to form the C1 spinal nerve.
The nerve’s function or subsequent branching patterns as the neural supply of the suboccipital group of muscles are unaffected by these inter-individual variations in the nerve’s origins. Additionally, the ventral ramus of the C1 spinal nerve split to form the suboccipital nerve, and 15 cadaveric specimens showed a connection with the dorsal ramus of the C2 spinal nerve
Considerations for Surgery
In procedures targeting the posterior neck at the levels of C1 and C2, the suboccipital nerve may be harmed. The suboccipital nerve may be harmed during procedures involving the midline suboccipital approach, such as distal vertebral artery bypass surgery or access to the brain’s fourth ventricle, and posterior methods for cervical neck fusions.
Clinical Relevance
Cervicogenic headaches and occipital neuralgia may both be caused by the suboccipital nerve. Whiplash injuries may potentially put the nerve at risk of harm. It is a novel target for these regional pain syndromes’ intervention and treatment as a result.
Headache from a spinal puncture
For cesarean section deliveries, pregnant women who receive spinal anesthesia may experience post-dural puncture headaches. These headaches typically have postural symptoms and may be accompanied by neck stiffness or, less frequently, photophobia, tinnitus, or vomiting. It has been estimated that the total incidence of post-dural puncture headaches is around 25%. The incidence varies with body mass index, the technique used, and the number of tries necessary to properly achieve spinal anesthesia.
The best course of treatment for the presumptive pathological mechanism of CSF leak following a puncture has been the implantation of an epidural blood patch, according to current practice. Bilateral suboccipital muscle injections with either saline solution or a mixture of dexamethasone and lidocaine were contrasted in a randomized control experiment. According to the study, those who had the steroid-anesthetic combination had lower headache scores, used oral analgesics less frequently, and experienced a remission of their nausea.
Spasm of the suboccipital muscles
The suboccipital muscles, like other muscles, can get strained and cause headaches, neck pain, or spasms. Additionally, whiplash injuries from car accidents or other injuries involving rapid deceleration can harm the suboccipital muscles and the suboccipital nerve. According to one notion, lesions to the rectus capitis posterior minor muscle may be the cause of suboccipital nerve damage from whiplash. Similar to other muscular strains, suboccipital muscle strains are typically treated supportively with exercises to improve posture, massage, stretching, NSAIDs, yoga, acupuncture, and physical therapy.
Oblique Neuropathy
Recurrent headaches that are restricted to the occipital region of the head and neck are a symptom of occipital neuralgia, also known as C2 neuralgia. Occipital neuralgia is defined as a sudden onset neuropathic pain that crosses the dermatomes of the larger occipital nerve and the lesser occipital nerve. It is often unilateral but can occasionally be bilateral. Occipital neuralgia is hypothesized to have a pathogenesis that results from external compression irritating either the larger or lesser occipital nerve. The occipital nerve area typically experiences a short shock, shooting, lightning-like, or stabbing pain. Specific movements or pressure to the occipital region may cause this pain. For instance, from fractured cervical vertebrae, cervical spondylosis, or too tensed muscles. Because of the anatomical differences Given that some anatomic variants of the suboccipital nerve attach to and anastomose with the lesser and greater occipital nerves, it may contribute to the etiology of occipital neuralgia.
When the cervical vertebrae are moved or palpated, cervicogenic headaches and migraines manifest as unilateral headaches or migraines. Due to referred pain from nerves, the discomfort can appear anywhere on the scalp, but it typically appears in the back of the neck. The pathophysiology of the C1-C3 nerves in the cervical vertebrae is thought to be the pathogenesis of cervicogenic headaches. Cervicogenic headaches may be caused by the suboccipital nerve, particularly in some anatomical variations where it interacts with the larger and lesser occipital nerves. Occipital nerve blocks can be both therapeutic and frequently diagnostic for occipital neuralgia and cervicogenic headaches.
Causes
Occipital neuralgia may be brought on by strained neck muscles or pinched nerves. Additionally, a head or neck injury could be the cause. Occipital neuralgia comes in two varieties: primary and secondary. An underlying illness is connected to a subsequent disorder.
- Occipital neuralgia may be brought on by any of the following factors, however in many cases, persistent neck stress or other causes are to blame.
- Upper cervical spine osteoarthritis
- greater and/or lesser occipital nerve injuries
- Compression of the C2 and/or C3 nerve roots or the greater and/or lesser occipital nerves as a result of degenerative alterations to the cervical spine
- the disease of the cervical disc
- the C2 and C3 nerve roots being affected by tumors
- Gout, Diabetes
- Infection symptoms of inflammatory blood vessel disease
- Occipital neuralgia is characterized by ongoing throbbing, burning, and agonizing pain interspersed with occasional shocks or shooting pains that typically begin at the base of the head and radiate to the scalp on each or both sides of the head. On the affected side of the head, patients frequently experience pain behind the eye. Additionally, even a minor motion like brushing your hair could cause pain. Many patients describe the pain as having migraine-like symptoms, and some may also suffer symptoms similar to those of cluster headaches and migraines.
Diagnostic Tests
Occipital neuralgia is difficult to diagnose because there isn’t a single test that can definitively confirm or exclude the diagnosis. To check for anomalies, a physical examination and a neurological exam are typically performed. A doctor may prescribe additional imaging to rule out any other potential reasons for the pain if the results of the physical and neurological examinations are ambiguous. An MRI exam, which may produce three-dimensional images of certain bodily structures and can identify any impingement, may be prescribed. The size and shape of body structures can be seen in a computerized tomography scan (also known as a CAT scan). Occipital nerve blocks are sometimes used by clinicians to corroborate their findings.
Treatment
Treatment for occipital neuralgia aims to lessen discomfort but does not offer a cure. Non-surgical and surgical interventions are also options.
Nonsurgical Procedures
Heat: Patients frequently get relief when heating pads or other devices are put on the sore location.
either massage or physical treatment.
Oral pharmaceuticals include anti-inflammatory drugs, muscle relaxants, and anticonvulsants.
Percutaneous nerve blocks, which include administering injections directly into the afflicted nerves, can be used to both diagnose and treat occiput neuralgia.
Botulinum toxin (Botox) injections can be used to lessen nerve irritability.
Occipital Nerve Stimulation: During this surgical operation, electrodes are positioned beneath the skin close to the occipital nerves. The procedure utilizes the same instrument as spinal cord stimulation and works in a similar way. Because of how minimally intrusive the procedure is, no adjacent nerves or structures are harmed by the stimulation. It is an off-label application of an FDA-approved medical device.
spinal cord stimulation -Stimulating electrodes are inserted surgically between the spinal cord and the vertebrae in a procedure known as spinal cord stimulation. The device produces electrical impulses to block the spinal cord from sending pain signals to the brain.
C2,3 Ganglionectomy: In this procedure, the second and third cervical sensory dorsal root ganglions are destroyed. The procedure’s immediate and long-term consequences were researched by Acar et al. (2008). According to the study, 95% of patients saw instant alleviation, and 60% continued to experience it after a year.
Cluster headaches
Attacks of intense, unilateral pain centered in the orbital, supraorbital, or temporal region are characteristics of cluster headaches.They can cause rhinorrhea, tearing, and sweating, and because of how painful they are, they have a very negative impact on quality of life. Injections of steroids or local anesthetics that target the greater occipital nerve have been used to treat cluster headaches. The effectiveness of a high-volume local anesthetic suboccipital nerve block in treating cluster headaches in individuals who had failed to respond to prior medical therapies was investigated in a case series observation research. According to the study, the reaction was helpful, with responders responding on average after 10.3 weeks, and two patients reporting pain freedom for 44 weeks. The intervention was determined to be safe and well tolerated, and subsequent research with more patients could examine this therapeutic option for this group of individuals who suffer from terrible cluster headaches that won’t go away.
Symptoms
- commonly occurring symptoms
- signs and symptoms of a cluster headache that damage the face
- group headacheImage enlarged
- Although you may initially experience migraine-like nausea and an aura, cluster headaches typically strike suddenly and without warning.
- Common headache warning signs and symptoms include:
- Usually in, behind, or around one eye, but it can also spread to other parts of your face, head, and neck, which is excruciating agony.
- Uneven suffering
- Restlessness
- a lot of tears
- Your affected eye on the affected side is red.
- the affected side of the nose will be congested or running
- forehead or face sweating on the troublesome side
- Pale skin (pallor) or facial flushing
- Your affected eye’s surrounding area is swollen,
- the eyelid on the affected side is drooping.
Contrary to migraineurs, cluster headache sufferers are more inclined to pace or rock back and forth while sitting. Although they typically affect one side, some migraine-like symptoms, such as sensitivity to light and sound, can accompany a cluster headache.
Characteristics of the cluster period
- Typically, a cluster phase lasts from a few weeks to months. Each cluster period’s beginning time and length could remain the same from one period to the next. Examples of seasonal cluster periods are every spring or every autumn.
- Episodic cluster headaches are common. In cases of episodic cluster headaches, the headaches continue for a week to a year, then go away for a period of three months or more before returning.
- Pain-free periods may last less than one month during chronic cluster episodes that last longer than a year.
During a period of clustering
- Headaches are common in a day or several times a day.
- An assault might last for anywhere between 15 minutes and three hours.
- The attacks frequently happen every day at the same time.
- The majority of assaults happen at night, typically 1-2 hours after you go to sleep.
- The intensity of the pain typically decreases quickly and stops abruptly as it started. Most victims of attacks are not in pain, but they are worn out.
- when to go to the doctor
- If you’ve only recently begun to have cluster headaches, consult your doctor to rule out other conditions and determine the best course of action.
- Even in extreme cases, headache discomfort is typically not caused by an underlying illness. The rupture of a weak blood artery (aneurysm) or a brain tumor are two dangerous underlying medical conditions that might occasionally be indicated by headaches.
- Additionally, if your pattern of headaches changes or they start to feel different all of a sudden, consult a doctor if you have a history of headaches.
signs and symptoms
- a terrible headache that comes on suddenly and sounds like thunder
- A headache accompanying a fever, nausea, vomiting, a stiff neck, mental disorientation, seizures, numbness, or difficulty speaking could be signs of a number of conditions, such as a brain tumor, stroke, meningitis, or encephalitis.
- even after a slight bump or tumble, a headache with a head injury is common, especially if it gets worse.
- unlike any headache you’ve ever had, it came on suddenly.
- a headache that gets worse over time and has a different pattern
Causes
- Cluster headache patterns suggest that the hypothalamus, the brain’s biological clock, maybe a cause of cluster headaches, even though the exact explanation is unknown.
- Contrary to migraine and tension headaches, triggers like certain foods, hormonal changes, or stress are rarely responsible for cluster headaches.
- However, once a cluster period begins, drinking alcohol may quickly result in a splitting headache. As a result, many people who have cluster headaches refrain from drinking when they have one.
- The usage of drugs like nitroglycerin, a prescription used to treat heart disease, is another potential trigger.
risk elements
Cluster headache risk factors include:
- Sex. Cluster headaches tend to affect more men than women.
- Age. Cluster headaches typically appear in adults between the ages of 20 and 50, though they can appear at any age.
- Smoking. Smokers are more likely to experience cluster headache attacks. However, most of the time quitting smoking has no impact on headaches.
- using alcohol. If you regularly experience cluster headaches, drinking alcohol during that time may make attacks more likely.
- a family’s past. Having a parent or sibling who has experienced a cluster headache may make you more susceptible.
FAQ
What is the suboccipital nerve’s origin?
The suboccipital nerve, also known as the dorsal ramus of the first cervical nerve, arises from the posterior/dorsal ramus of the first cervical spinal nerve (C1). From its origin, the suboccipital nerve passes to the posterior neck area.
what does the suboccipital nerve do?
The rectus capitis posterior major, rectus capitis posterior minor, obliquus capitis superior, and obliquus capitis inferior are the four suboccipital muscles that are innervated by the suboccipital nerve.
What Innervates the suboccipital muscles?
The suboccipital nerve, which is created by the dorsal ramus of C1, innervates the muscles. The vertebral artery and suboccipital nerve are located in the suboccipital triangle, which is formed by three of the four muscles.
Is suboccipital nerve motor or sensory?
spinal nerves in the neck
The suboccipital muscles receive motor innervation from the dorsal ramus (suboccipital nerve), which travels between the vertebral artery and the posterior arch of the atlas.
What advantages can suboccipital release offer?
In order to treat musculoskeletal issues including neck discomfort and headaches, medical professionals can employ the suboccipital release technique, which is rather simple. Due to the manipulation of the occipital-atlanto region, this approach is also adaptable and can assist in regulating the autonomic system in the body.
Can occipital nerves regenerate?
Occipital neuralgia might disappear on its own, although it might take some time. Not every person needs to be treated with medicine and surgery. Occipital neuralgia can disappear on its own if the source of the inflammation is treated.
The suboccipital nerve travels at what level of the spine?
The suboccipital nerve refers to the first cervical nerve’s (C1) dorsal main ramus. Between the skull and the atlas, the first cervical vertebra, it leaves the spinal cord. The occipital bone and the first three cervical vertebrae are visible in the median sagittal slice.
Suboccipital nerve headaches: what are they?
With time, the upper cervical ligaments become overly stretched, which causes the suboccipital muscles to contract. When they are worn out, they can cause severe pain. One of the main signs of upper cervical instability is suboccipital muscular tension or headache.
What is the suboccipital muscle’s blood supply?
Blood flow
The vertebral artery and the deep descending branches of the occipital artery both supply blood to all of the suboccipital muscles.
What is the suboccipital group’s primary function?
At the base of the occipital bone, there are four pairs of deep muscles collectively known as the suboccipital muscles. Their primary movements involve rotating and extending the head. They are made up of the rectus capitis posterior major, rectus capitis posterior minor, and the obliquus capitis superior and inferior.
What role does the suboccipital triangle have in clinical practice?
The vertebral artery and suboccipital nerve are located in the suboccipital triangle, which is formed by three of the four muscles. To prevent potentially fatal bleeding, this landmark is especially crucial for surgeons working in the posterior cervical region.