Supraspinatus Tendinitis: Physiotherapy Management
Definition of Supraspinatus Tendinitis:
Supraspinatus tendinopathy is a common and disabling condition that becomes more prevalent after middle age and is a common cause of pain in the shoulder. A predisposing factor is a resistive overuse.
The supraspinatus tendon of the rotator cuff is involved and affected tendons of the musculoskeletal system and becomes degenerated, most often as a result of repetitive stresses and overloading during sports or occupational activities.
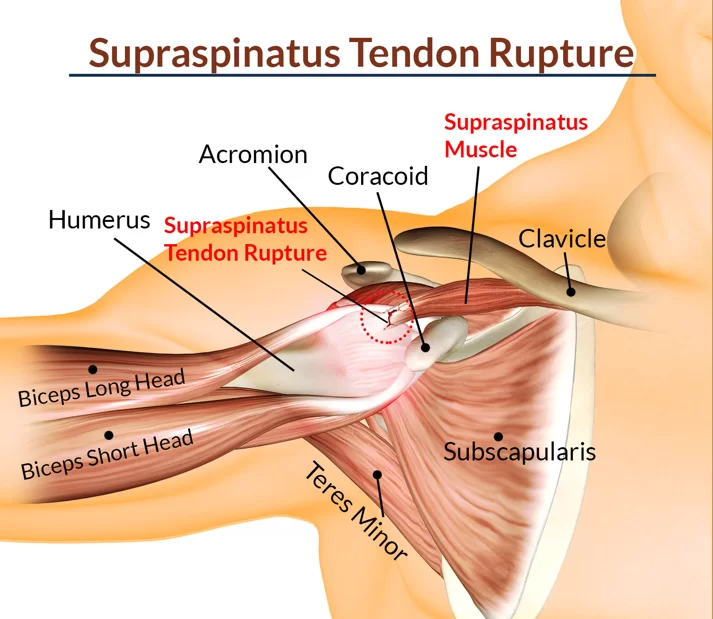
The tendon of the supraspinatus commonly impinges under the acromion as it passes between the acromion and the humeral head. This mechanism is multifactorial.
Anatomy of the Supraspinatus Muscle, Tendon, and Relevant Other Body Parts:
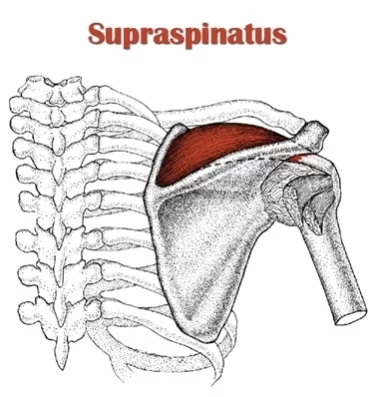
The supraspinatus muscle is of the greatest practical importance in the rotator cuff, derives its innervation from the suprascapular nerve, and stabilizes the shoulder, exorotates, and helps abduct (lift up sideways) the arm, by initiating the abduction of the humerus on the scapula.
Any friction between the tendon and the acromion is normally reduced by the sub-acromial bursa.
The anterior margin of the supraspinatus is defined by the posterior edge of the rotator interval that separates the supraspinatus from the rolled superior border of the subscapularis. The posterior margin of the supraspinatus is marked by the extension of the raphe between the supraspinatus and infraspinatus around the scapular spine. The anterior portion of the supraspinatus is composed of a long and thick tendinous component, whereas the posterior portion has been shown to be short and thin.
An anatomic dissection study of the supraspinatus footprint found that the mean anterior to posterior dimension of the supraspinatus tendon was 25 mm, with a mean medial to lateral thickness of the footprint of 12 mm – the mean distance from the cartilage to the supraspinatus footprint was 1.5 mm at the mid-tendon.
The supraspinatus and infraspinatus tendons fuse 1.5 cm proximal to their insertions. Collagen is the major matrix protein of supraspinatus tendons, consisting of > 95% type I collagen, with lesser amounts of other collagens including collagen type III.
The anatomy of the supraspinatus’s insertion is of key relevance in terms of its extracellular matrix composition and has been categorized into four transition zones. The first zone is the proper tendon, made up of large type I collagen and small amounts of decorin. The second zone is fibrocartilage and consists largely of types II and III collagen, with small amounts of types I, IX, and X collagen. The third zone is mineralized fibrocartilage and consists of type II collagen, with significant amounts of type X collagen and aggrecan. The fourth zone is bone and is largely type I collagen with a high mineral content. This effective bone-tendon attachment is achieved through a functional grading in mineral content and collagen fibre orientation. The supraspinatus enthesis is a highly specialized inhomogeneous structure that is subjected to both tensile and compressive forces.
What are the Causes of Supraspinatus Tendinitis?
The mean age of onset of this complication is in the sixth decade (age 50 to 59), and it is more frequent in diabetic patients. It is also a common cause of shoulder pain in athletes whose sports involve throwing and overhead motions.
The causes of supraspinatus tendinitis can be primary impingement, which is a result of increased subacromial loading, and secondary impingement, which is a result of rotator cuff overload and muscle imbalance.
What are the signs/Symptoms Of Supraspinatus Tendinitis?
Patients present with progressive subdeltoid aching that is aggravated by abduction, elevation, or sustained overhead activity. They also feel tenderness and a burning sensation in their shoulder. The pain may radiate to the lateral upper arm or may be located in the top and front of the shoulder. It typically becomes worse with overhead activity. Initially, the pain is felt during activities only, but eventually may occur at rest.
One has to think of supraspinatus tendinopathy when the patient says:
Pain increases with reaching.
Pain is felt after frequent repetitive activity at or above the shoulder.
The patient feels the weakness of resisted abduction and forward flexion, especially with pushing and overhead movements.
Patient has difficulty sleeping at night due to pain, especially when lying on the affected shoulder, and with an inability to sleep.
Patient has difficulties with simple movements, such as brushing hair, putting on a shirt or jacket, or reaching the arm above shoulder height.
Patient has a limited range of motion in the shoulder.
Patient had a former shoulder trauma.
The shoulder may be warm and there may be fullness anterolaterally. Further, there is a painful arc between 70° and 120° of abduction.
So supraspinatus tendinitis is usually consistent with anterior instability causing posterior tightness. The problems that patients with Supraspinatus Tendinitis complain off, are pain, inflammation, decreased ROM, strength, and functional activity.
Differential Diagnosis of Supraspinatus Tendinitis:
In general, the causes of an acute painful shoulder can be classified into different categories, according to the prevailing pathoanatomy. These include
- Acromioclavicular Joint Injury
- Bicipital Tendonitis
- Brachial Plexus Injury
- Cervical Disc Injuries
- Cervical Discogenic Pain Syndrome
- Cervical Radiculopathy
- Cervical Spine Sprain/Strain Injuries
- Clavicular Injuries
- Contusions
- Degenerative causes like rotator cuff tear, cervical spine radiculopathy, and osteoarthritic glenohumeral joint
- Infraspinatus Syndrome
- Infective causes like acute pyogenic arthritis and osteomyelitis
- Inflammatory causes like gouty arthritis, adhesive capsulitis or frozen shoulder, and calcific tendonitis
- Myofascial Pain in Athletes
- Neoplastic causes like tumor metastasis
- Shoulder Dislocation
- Subacromial impingement
- Superior Labrum Lesions
- Swimmer’s Shoulder
- Traumatic fractures and dislocation
HOW IS INVESTIGATION DONE IN SUPRASPINATUS TENDINITIS?
More probing investigations can narrow down the differential diagnoses, which could include:

blood for white cell counts, search for abnormal blood biochemistry and inflammatory markers, as well as radionuclide imaging and MRI.
The MRI findings of rotator cuff tendinopathy are characterised by thickened inhomogeneous rotator cuff tendon with increased signal intensity on all pulse sequences. Fluid intensity filling an incomplete gap in the tendon on fat-suppressed T2-weighted sequences changes are seen on MRI for partial-thickness tears. On MRI, an area of high signal intensity on all pulse sequences outlines complete disruption of the tendon
Outcome Measures :
Diagnosis is usually clinical, but imaging can be useful. Shoulder x-rays can reveal calcifications in rotator cuff tendons and in the bursa. In longstanding cases, there may be degenerative changes, such as cystic/sclerotic changes at the greater tuberosity and decreased humeral head-acromion distance, secondary to upward migration of the humeral head. In acute calcific tendinitis, calcifications may be irregular, fluffy, and ill-defined. Dynamic ultrasound can demonstrate thickening of the subacromial bursa and impingement during abduction. Magnetic resonance imaging (MRI), rather than computed tomography (CT), is the preferred modality since it produces more detailed soft-tissue images.
Examination of Supraspinatus Tendinitis:
The anamnesis often reveals that, in case of a calcification, due to trauma, pain emerges later on, after a few hours.
The physical examination consists of taking the temperature, looking for external wounds or bruises over the affected should,r and checking the skin temperature. Further, the examiner will palpate in the area of the tendinous insertion of the supraspinatus muscle for checking tenderness and pain. Both passive and active movements will be performed.
With clinical examination, other causes of shoulder pain should be excluded. So the neck, shoulder and chest wall have to be examined
The shoulders are inspected for symmetry, localized swelling, and muscle atrophy. There may be tenderness below the acromion and over the greater tuberosity. Internal rotation of the shoulder can facilitate palpation of the supraspinatus insertion on the greater tuberosity.
The most important clinical maneuvers are as follows:
Painful arc
Testings:
Neer’s sign
Hawkin’s sign
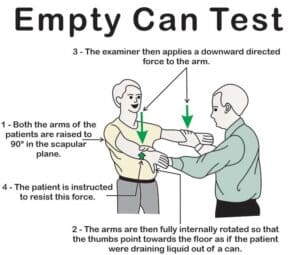
Supraspinatus challenge test = “The Empty Can” sign = Job‘s test
Drop arm test
Impingement test
Neer’s test, Hawkin’s sign, Empty Can sign
If sonography is done, the standard method for sonographic evaluation of the supraspinatus tendon requires the arm behind the back (Crass position) or hand on the back pocket (modified Crass position).
Yet diagnosis is usually clinical, but imaging can be useful. Shoulder x-rays can reveal calcifications in rotator cuff tendons and in the bursa. In longstanding cases, there may be degenerative changes, such as cystic/sclerotic changes at the greater tuberosity and decreased humeral head-acromion distance, secondary to upward migration of the humeral head. In acute calcific tendinitis, calcifications may be irregular, fluffy, and ill-defined. Dynamic ultrasound can demonstrate thickening of the subacromial bursa and impingement during abduction. Also, sonography and Magnetic resonance imaging (MRI) can be done.
Supraspinatus tendinosis can be graded using a modified 4-point scale from 0 to 3 based on previous studies. Diagnosis is based on the appearance of the rotator cuff tendons (grading system) and the presence or absence of signs denoting involvement of the subacromial bursa and subacromial–subdeltoid plane
Treatment:
Medical Management:
The treatment used to manage a supraspinatus tendonitis depends on the etiology of the pathology. At first, a conservative treatment is preferred. This treatment involves physiotherapy, nonsteroidal anti-inflammatory drugs (NSAIDs), ice treatments, and resting. Corticoid injections can also be used in addition to physical therapy. A surgical intervention can be a solution if there is no improvement after 3-6 months of conservative treatment.
NSAIDs may be the first choice for mild to moderate symptoms if there are no contraindications to these agents. A short-term use (7-14 days) of NSAIDs is useful to relieve the pain associated with tendinitis. However, there is little evidence supporting a long-term course of NSAIDs.
Moderate to severe symptoms may require a local subacromial corticosteroid injection. For more information about corticosteroid injections.
The major indications for surgery are ongoing pain, loss of function, failure to respond to conservative therapy for 3 months, or evidence of an acute tear in a younger patient. Surgical approaches include calcium deposit resection, with or without subacromial decompression, bursal resection, and acromioplasty, using either arthroscopic or open methods. It’s also possible to split off the coraco-acromial ligament to enlarge the space between the acromion and humerus. This can cause instability, but we can compensate for it with some training of the rotator cuff. With physiotherapy, it takes patients up to 4 months to recover. The goal of surgery is to obtain pain relief, increased range of motion, and increased power.
ABursal resection: Removement of the subacromial bursa.
Acromioplasty: Generally, it implies the removal of a small piece of the surface of the acromion that is in contact with a tendon, causing, by friction, damage to the latter tissue.
Physiotherapy Management of Supraspinatus Tendinitis:
The main goal in the acute phase (initial phase) is to alleviate pain, inflammation, prevent aggravation of pain, reduce muscle wasting, and normalize the arthrokinematics of the shoulder girdle. A period of rest should be considered in order to avoid further aggravation and shoulder discomfort.
Electrotherapy modalities should be considered in order to avoid painful aggravation. Modalities such as SWD, IFT, TENS, ultrasound, and cryotherapy can provide temporary relief in the acute phase.
Strengthening exercises, such as isometric exercises, should be considered in order to work out the shoulder girdle musculatures. Proper home exercise programs should also be taught in conjunction with proper ergonomics.
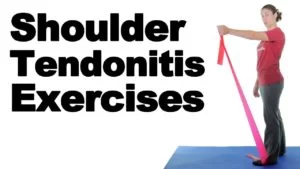
The management of supraspinatus tendonitis consists of different progressive exercises. There are three phases of treatment: Immobilization, passive/assisted range of motion, and progressive resistance exercises of the Supraspinatus Muscle.
Early management includes avoidance of repetitive movements that aggravate the pain. Patients should be informed about pain-provoking postures and movements. Cryotherapy, soft tissue techniques, and wearing a sling/taping are some other techniques to relieve pain. Gentle range-of-motion exercises, such as Codman’s classic pendulum exercises, maintain range of motion and prevent the development of adhesive capsulitis. Once pain has been reduced, joint mobilisations, massages, muscle stretches, active-assisted and active exercises are needed to improve the ROM again. Active-assisted mobilisations can be done by the patient himself/herself by using an exercise bar. We can also use a rope and pulley; this way, the unaffected arm is able to pull the affected one into anteversion. Strengthening exercises should work on the external rotators, internal rotators, biceps, deltoids, and scapular stabilizers.
Strengthening these muscles will keep the shoulder joint more stable and prevent further injuries. Eccentric exercises will also be more effective than concentric exercises.
I.E.:

Sidelying external rotation with dumbbell against gravity.
Prone horizontal abduction with dumbbell against gravity
Prone anteflexion in the plane of the scapula
Prone row with external rotation
External rotation with Thera-tubing (standing position)
Horizontal abduction with Thera-tubing (standing position)
Rows with Thera-tubing (standing position)
Elevation in the plane of the scapula (standing position)
Scapula settings
Scapular protraction and retraction
Joint mobilization may be included with inferior, anterior, and posterior glides in the scapular plane.
Stretching exercises should be done by repeating the exercise 3 times and holding the stretch each time for 30 seconds.
Neuromuscular control exercises also may be initiated. PNF patterns will increase strength in rotator cuff muscles and increase the stability of the shoulder. We can use four different patterns.
Modalities that also may be used as an adjunct include cryotherapy, hyperthermia, transcutaneous electrical nerve stimulation, and ultrasound. Intensive ultrasound therapy has been shown to increase calcium resorption, but this requires frequent treatment that may not always be practical.

Self-exercise for Supraspinatus Tendinitis :
Patient’s starting position: sitting, arm abducted to a position before symptoms appear, contact with three finger tips of the left hand in the supraspinous fossa.
Movement: pressure into the supraspinous fossa, active adduction of the right glenohumeral joint, then releasing the pressure into the supraspinous fossa, and back to the starting position.
Patients suffering from non-calcifying supraspinatus tendinopathy may benefit from low-energy extracorporeal shock wave therapy, at least in the short term.
At the end of the therapy, you should initiate plyometric and sports-specific exercises.
Patient education is again re-emphasized, as well as maintaining proper mechanics, strength, and flexibility, and having a good understanding of the pathology. The patient should also show an understanding of a home exercise program with the proper warm-up and strengthening techniques.




8 Comments