Swollen Calf
What is a Swollen Calf?
Swollen calf refers to the abnormal enlargement or puffiness in the lower leg area between the knee and ankle mainly the backside. This condition can be caused by various factors, ranging from minor injuries to serious medical conditions.
The swelling may be accompanied by pain, tenderness, and restricted movement, impacting an individual’s daily activities.
Introduction
The calf muscles, known as the gastrocnemius and soleus, make up the bulk of the lower back portion of the leg. These powerful muscles attach at the knee joint and extend down to merge with the Achilles tendon at the heel. The gastrocnemius is the larger, outer muscle that gives the calf its distinctive curved shape. The soleus lies underneath, attaching lower to the leg bones.
These calf muscles play a key role in activities like walking, running, jumping, and standing on tippy toes. They contract to propel the body forward and lift the heel. The calf muscles must push against resistance from body weight to pump blood back up from the lower legs.
If the calf muscles become injured, strained, or damaged, they can easily become swollen and painful. This occurs because swelling is the body’s response to heal damaged tissue. When calf muscles are overworked, small tears in the muscle fibers cause localized trauma. Blood vessels leak fluid containing nutrients and infection-fighting cells into the tissue. This shows up as puffiness, enlargement, and swelling visibly shifting the shape of the calf.
Some swelling and soreness after calf exercise are normal. However excessive, persistent, or painful swelling should not be ignored. Chronic swelling strains the tissue and skin, potentially leading to permanent damage. Swollen calves can greatly impact mobility if left untreated.
Swelling may indicate an underlying blood clot, vein damage, or systemic disease. Getting a proper diagnosis is key to reducing swelling and restoring normal function. With proper self-care, medications, physiotherapy, or procedures, swollen calf muscles can heal and regain strength. Catching calf issues early prevents complications and long-term leg health impacts.
Causes of Swollen Calf
Environmental Causes
Lifestyle Factors
- Being Overweight: Carrying excess body fat puts increased pressure on the lower leg veins and lymphatic system. This can cause fluid buildup and swelling in the calves. Losing weight can relieve the pressure.
- Pregnancy: Hormone changes during pregnancy relax vein walls and slow blood return from the legs. Weight gain and uterus pressure on veins also contribute. Elevation, compression stockings, and staying active can help reduce swelling.
- Menstruation: Hormone shifts related to a woman’s monthly cycle can temporarily cause water retention and calf swelling. This normally resolves once menstruation ends.
- Prolonged Standing: Gravity pulls blood into the lower limbs when standing. Pooling blood stretches vessels and fluid leaks into calf tissues. Movement and elevating of legs periodically can prevent swelling.
- Prolonged Sitting: Inactive calves aren’t contracting to pump blood back to the heart efficiently. Blood and lymph fluid can accumulate, stressed by gravity’s pull. Periodic movement and walks are helpful.
Medications
- Antidepressants: Certain depression medications like SSRIs and MAOIs affect serotonin levels which can influence sodium retention and increase calf swelling.
- Hormone Medications: Birth control pills, hormone replacement therapy, and medications that alter hormone levels can trigger fluid retention and swollen calves as a side effect.
- Steroids: Both oral and topical corticosteroid medications impact fluid balance and can cause swelling localized in the legs and calves.
Traumatic Causes
- Muscle Strain: Overstretching or tearing calf muscles and connective tissue from sudden exertion causes bleeding and inflammation. Fluid rushes to aid healing but remains trapped within compartments surrounded by fascia. Strains require RICE treatment – rest, ice, compression, and elevation.
- Broken Bones: Major trauma like an ankle twist or hard fall that breaks the tibia or fibula bones can severely damage soft tissue in the calf. Swelling results from internal bleeding and fluid buildup around the injury. This requires prompt medical treatment including possible surgery.
- Post-Surgery: Incisions into the calf muscle during procedures like compartment release or vein stripping cause localized trauma. Swelling occurs when fluid and blood fill the wound to help heal and fight infection. Elevation and medication help reduce post-op swelling.
Systemic Diseases
Organ Failure
- Heart Failure: A weak heart doesn’t effectively pump blood out of veins. Blood backs up causing swelling in feet and legs. Lying down and diuretics provide relief.
- Kidney Failure: Damaged kidneys cannot properly filter fluid and sodium from the blood. This floods and overwhelms the body’s tissues causing severe widespread swelling including the calves.
- Liver Failure: Scarring of liver cells obstructs blood and lymph flow through the liver. The build-up of fluid in the form of ascites or peripheral edema moves down the body into the legs.
Vascular Issues
- Blood Clots: A deep vein thrombosis (DVT) blocks blood flow out of the calf. Painful swelling results from the backed-up blood. Partial clots can break off and travel to the lungs causing life-threatening pulmonary embolism.
- Poor Circulation: Weak valves or veins prevent efficient blood return from the lower legs. Gravity pulls blood downward into the calves and causes swelling that is worse after standing or at night.
Inflammatory Conditions
Autoimmune Disease:
- Rheumatoid arthritis causes joint inflammation and destruction that can spread into the ankle and feet
- Swelling in these joints leaks fluids that gravity pulls upwards into the calf region
- Lupus can also cause inflammation in the lower leg joints and skin that results in calf swelling
Infection
- An infection of the dermis layer called cellulitis spreads swelling across lower leg areas like the calf. The immune response fills tissues with white blood cells and proteins to fight bacteria. Antibiotics treat the infection and reduce inflammation-related swelling.
Pulmonary Embolism
- A blood clot that forms in the leg veins breaks off and travels to the lungs
- This blocks blood flow and causes pressure buildup in lung arteries
- Fluid leaks from flooded lung vessels into calf area tissue due to backup pressure
- Swelling and pain occur as blood struggles to return from the lower limbs
Deep Vein Thrombosis (DVT)
- Blood clotting within deep calf veins obstructs proper blood flow
- Leaked fluids get trapped below the thrombosis, causing localized swelling
- Pain, heat, and redness occur as blood pools and inflammation develops
Crush Injury
- Traumatic compression of the calf muscles causes muscle and nerve damage
- Fluid rushes to the area as the tissues heal, creating dramatic swelling
- Inflammation related to injured tissue builds up and tightens within muscle compartments
Compartment Syndrome
- Internal bleeding and swelling spread rapidly within an enclosed muscle compartment
- The fascia layers surrounding muscles cannot stretch to accommodate the flood of fluids
- Extreme inflammation and pressure buildup occur cutting off circulation to the calf tissues
Cellulitis Infection
- Bacteria spread across lower leg layers of skin, fat, and muscle tissue
- The body’s immune response triggers inflammation that fills the calf region with fluid
- Redness, heat, swelling, and pain spread as muscles become infected
Achilles Tendon Rupture
- The Achilles tendon tears partially or completely due to sudden overstretching
- Bleeding and inflammation occur at the rupture site
- Fluid fills the space between torn tendon ends and leaks into calf tissues
- The swelling spreads up the leg as the blood struggles to return upwards
Diagnosis of a Swollen Calf
- Medical History – Doctor asks about symptoms, onset, injury/trauma, risk factors, other illnesses
- Physical Exam – Checks for swelling, skin changes, warmth, redness, pain when touched
- Ultrasound – Uses sound waves to evaluate blood clots, blockages, muscle/tissue abnormalities
- Blood Tests – Assess infection markers, clotting time, kidney/liver/heart function
- CT or MRI Scans – Cross-sectional images checking for masses, fluid, bone breaks
- Vein Function Tests – Assess blood flow, and valve competency to rule out varicose veins
Preventing a Swollen Calf
Exercise Properly
- Warm up calves properly before exercise with stretches
- Build calf conditioning gradually without overdoing activity
- Allow rest days between calf-intensive workout sessions
- Wear supportive shoes with adequate heel cushioning
Maintain Healthy Weight
- Extra weight puts pressure on calves, cutting off circulation
- Losing excess fat reduces calf swelling triggers
Compression Stockings
- Gradient pressure helps pump blood back from calves
- Supports vein function and prevents blood pooling
Lifestyle Factors
- Stay hydrated and limit sodium to avoid water retention
- Elevate legs periodically when sitting or sleeping
- Avoid crossing your legs for extended times
- Stretch calves routinely when traveling for long periods
Seeking preventative vascular or podiatry care helps detect risk factors like poor circulation or posture issues contributing to calf swelling. Addressing these proactively can prevent long-term calf issues.
Treatments for a swollen calf
Medications
- Diuretics: Remove excess fluid through increased urination, relieving swelling
- Blood Thinners: Prevent clot formation and progression for deep vein thrombosis
- Antibiotics: Used for infections causing calf swelling like cellulitis
- Anti-inflammatories (NSAIDs): Reduce swelling and pain from strains, injuries
Physical Therapy Treatment
- Ice: Apply ice packs to the swollen calf for 15-20 minutes several times per day to reduce inflammation and pain. Cold therapy constricts blood vessels.
- Compression: Gradient compression stockings, wraps, or intermittent compression devices are used to prevent blood and fluid from accumulating in the calf. This also aids circulation.
- Massage: Light massage using downward strokes helps push excess fluid out of the tissues. This also prevents scar tissue formation.
- Exercises: Specific stretches and strengthening moves improve calf flexibility and muscle pump activity to circulate blood and lymph fluid properly.
- Ultrasound: Sound waves are used to warm deep calf tissues and improve blood flow. Ultrasound also helps break up scar tissue.
- Elevation: Keeping the leg raised above heart level utilizes gravity to drain fluid from the calf region. This is especially important when inactive or sleeping.
- Contrast Baths: Alternate hot and cold water immersion to improve circulation
- Passive Stretching: Gently stretch calf muscles and tendons to maintain flexibility and range of motion, prevent contractures
- Tilt Table Standing: Slowly adapt the patient to upright standing to allow drainage
- Manual Edema Mobilization: Special tissue mobilization techniques to clear extracellular fluid
A combination approach of medication, compression, activity modification, and physical therapy typically provides the best reduction of calf swelling and restoration of function after injury.
Symptoms
- Visible swelling or enlargement of the calf area
- Tight or shiny skin over the swollen region
- Pain or tenderness when pressure is applied
- Redness, warmth, and hardness may indicate infection
- Numbness or tingling due to nerve compression
- Leg fatigue, heaviness, or aching after activity
- Noticeable difference in calf shape/contour compared to other leg
Complications
Permanent Tissue Damage
- Prolonged swelling stretches the calfskin, fascia, and muscle fibers beyond capacity
- Fatty tissue gets damaged beneath the skin as swelling cuts off blood supply
- This can lead to pitting edema and long-term deformity in the calf shape
Deep Vein Thrombosis:
- Swelling related to a blood clot builds pressure inside deep calf veins
- The clot can dislodge and travel to the lungs causing pulmonary embolism which can be life-threatening
- Unrelieved swelling leads to dangerously high pressure inside muscular compartments
- Compresses nerves and blood vessels eventually causing muscle death if not treated promptly
Infection Spreading:
- Swelling due to infection like cellulitis allows bacteria to proliferate
- Further tissue death and systemic illness can occur if swelling is not controlled
Leg Ulcers:
- Persistent swelling stretches and damages skin integrity leading to open wounds
- Poor circulation impedes calf ulcer healing allowing infection entry
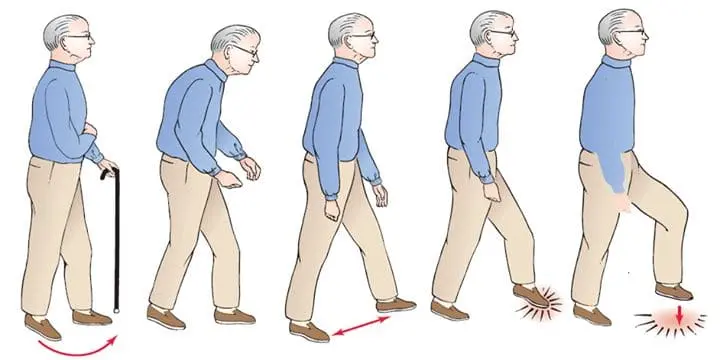
Reduced Mobility:
- Long-term swelling leads to limited ankle/knee function, walking difficulties
- Can necessitate assistive devices to prevent fall risks
Seeking prompt diagnosis and treatment is key to preventing the wide-ranging complications and potential disability associated with persistent calf swelling.
When to See a Doctor
- Severe or sudden calf swelling
- Rapid doubling in calf size
- Skin redness, heat, purpling, or blistering
- Numbness, tingling, or inability to move the ankle/toes
- Signs of infection like fever, nausea, dizziness
- Shortness of breath or chest pain along with calf swelling
- Swelling lasting more than 3 days without improvement
- Known injuries such as a strained muscle or broken bone
- Recent major surgery of the hips, legs, or abdomen
Seeking prompt medical attention ensures serious causes like blood clots, compartment syndrome, or infections are diagnosed and treated early before further calf damage or complications occur.
Summary
A swollen calf occurs when fluids accumulate in the muscles and tissues of the lower leg, leading to enlargement, tightness, and potential deformity in the shape of the calf. Causes range from minor strains to serious medical conditions like blood clots, infections, and organ failure. Symptoms include visible swelling, redness, warmth, pain, numbness, and difficulty walking.
While calf swelling from standing too long or working out intensely may resolve with at-home rest and ice, persistent swelling demands medical attention. Swelling left unchecked can compress nerves and tissue leading to compartment syndrome, skin damage, reduced mobility, and in worst cases, amputation or pulmonary embolism. Prompt diagnosis via exams and imaging determines the underlying condition.
Treatments focus on relieving pressure and restoring circulation to the calf through methods like medication, compression, surgery, and physical therapy techniques to drain fluid and mobilize tissue. Preventative measures like gradient stockings, activity modification, and addressing risk factors are key, especially for those with chronic conditions causing poor circulation or edema.
Seeking urgent care for sudden or severe unexplained calf swelling allows early treatment of blood clots, infection, or other dangers before lasting calf injury and disability occurs. Ongoing management of chronic swelling can maintain calf health, strength, and function.
FAQs
What causes calf muscle swelling after exercise?
Overexertion can strain calf muscles and ligaments, causing microscopic tears where fluid builds up during healing.
Do swollen calves mean a blood clot?
Possibly, as a symptom of dangerous deep vein thrombosis. However many conditions cause calf swelling, so an exam is needed.
Should I wrap or elevate a swollen sore calf?
Yes, using compression and elevation can significantly help reduce calf swelling.
When should I worry about calf swelling?
If severe, comes on suddenly, persists over 2-3 days, or includes numbness/weakness, seek medical care promptly.
Can physical therapy help edema in calves?
Yes, techniques like massage, compression, and specialized exercises can effectively help drain calf fluid accumulation.
References
- Street, K. (2022, March 16). Swollen Calf: Common Causes of Swelling. buoy.
- Clinic, C. (2023, December 8). 5 Reasons Your Legs May Be Swollen and What To Do About It. Cleveland Clinic. https://health.clevelandclinic.org/when-is-leg-swelling-a-sign-of-something-serious
- Mrcgp, T. H. (2023, September 13). Swollen Legs. https://patient.info/signs-symptoms/oedema-swelling/swollen-legs
- Writer, S. (2023, March 13). Swollen Calf. Vascular Medicine. https://angiologist.com/swollen-calf/