Cervicobrachial Syndrome
What is Cervicobrachial Syndrome?
Cervicobrachial Syndrome, also known as Cervicobrachalgia, refers to the condition characterized by pain and stiffness in the cervical spine, accompanied by symptoms in the shoulder girdle and upper extremities. It may display as tingling, numbness, or pain in the arm, upper back, & upper chest, occasionally escorted by headaches.
Description
When a combination of neck-related complaints and radiating symptoms occur in the arm, the condition is referred to as cervicobrachial syndrome or cervicobrachialgia. This syndrome specifically pertains to a cervical disorder characterized by pain radiating into the upper limb. Previously known as ‘lower cervical syndrome,’ it is associated with pain, numbness, weakness, and swelling in the neck and shoulder region. Additionally, there are sensory disturbances and pain that extend from the cervical spine into the upper limb, following a distinct radicular pattern along the distribution of the ventral branch of a spinal nerve.
It’s important to note that cervical radiculopathy typically represents a non-radicular phenomenon. However, a diagnosis of cervical radiculopathy can be made when there are evident sensorimotor deficits within the corresponding nerve root territory. On the other hand, the term ‘cervicobrachial syndrome’ should be used to describe a collection of neck and arm symptoms without a known and proven cause. If a patient can be objectively diagnosed with cervical radiculopathy or thoracic outlet syndrome, a specific and documented diagnosis should be utilized.
Clinically Relevant Anatomy
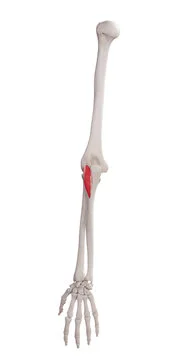
The cervicobrachial syndrome can often be attributed to cervical radiculopathy, which is characterized by discogenic brachialgia caused by lesions affecting the C5/6 and C6/7 motion segments. It is worth noting that the distribution of cervical dermatomes and myotomes doesn’t directly align, meaning that the myotome does not necessarily correspond to the underlying dermatome. Consequently, various muscles in the upper trunk, which are primarily innervated by cervical nerve roots, are frequently affected in cervical syndromes. Such muscles include the rhomboids, supraspinatus, infraspinatus, deltoid, serratus anterior, and latissimus dorsi.
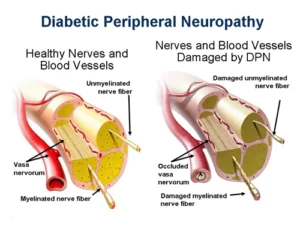
Further, the cervicobrachial syndrome can even originate from neurogenic & vascular compression within the thoracic outlet. This compression occurs when there is a narrowing of spaces in this region, leading to the compression of structures such as the brachial plexus, subclavian artery, or subclavian vein. These compressions contribute to the manifestation of symptoms associated with cervicobrachial syndrome.
Epidemiology of Cervicobrachial Syndrome
Cervicobrachialgia has been reported to have a higher prevalence compared to isolated neck pain. This particular complaint is frequently encountered among patients who seek physiotherapy interventions for both neck and arm pain. In a study conducted by Radhakrishnan et al., it was discovered that 32% of patients with cervicobrachial pain experienced recurrent episodes over an average period of 4.9 years.
The majority of individuals affected by this condition are engaged in manual work that involves continuous and repetitive tasks. These tasks often include activities like computer work, writing, manipulating or moving objects, as well as lifting or performing overhead work. It is important to note that tasks requiring the neck to be held in the same position for extended periods can be particularly aggravating factors for this condition.
Symptoms of Cervicobrachial Syndrome
The cervicobrachial syndrome is appropriately used when patients present with complaints of pain accompanied by neurological disorders such as tingling, sensory disturbances, or even a loss of motor skills in the arm, hand, and fingers. In some cases, there may be a noticeable decrease in power and impaired control of motion.
Currently, there are no universally agreed-upon clinical criteria for diagnosing cervicobrachialgia. However, common findings associated with this condition often include pain and fatigue experienced in the wrists, forearms, shoulders, and neck. Patients may also report a sensation of swelling in their hands, as well as a feeling of heaviness or numbness in the upper extremity. Pain is typically exacerbated by physical activity and relieved by rest, although there are instances where pain worsens during nighttime, leading to sleep disturbances. Some individuals describe the sensation of wearing gloves despite not wearing any. It is not uncommon for these symptoms to be accompanied by severe headaches.
The term “cervicobrachial syndrome” is used by some physicians to describe symptoms suspected to be caused by cervical nerve root irritation that cannot be objectively confirmed. Conversely, other physicians reserve this term for patients whose symptoms may arise from undetectable thoracic outlet syndrome. Additionally, some physicians utilize the term as a synonym for “myofascial pain syndrome,” which involves symptoms in the neck and/or shoulder believed to originate from muscle-related issues.
Patients with cervicobrachialgia tend to be more sensitive to sensory and motor stimuli, particularly on the side where they experience symptoms. Their detection thresholds are often elevated compared to patients without cervicobrachialgia. Furthermore, there is a higher prevalence of poor postural control among individuals with cervicobrachialgia when compared to healthy patients.
Diagnosis of Cervicobrachial Syndrome
Neck aches can originate from different reasons, involving pain arising in the shoulders & arms (painful shoulder), cervical radiculopathy, levator scapulae syndrome, polymyalgia rheumatica (painful shoulder), earlier phases of rheumatic diseases, for example, rheumatoid arthritis (RA) (at any age) or ankylosing spondylitis (in individuals aged 30 years and above), as well as infections or bone lesions of the cervical spine (e.g., Spondylodiscitis or metastases). Cervical pains can also be provoked by sudden movements or repeated muscular strains, often due to joint and ligament irritation. The proximity of the vertebral artery and autonomic nerve fibers to these joints adds a neurovascular component. Further probable diagnoses contain trapped nerves, sprained shoulder muscles, supraspinatus tendinitis for shoulder pain with positive static muscle tests, sprained rib muscles for medial scapula pain, carpal tunnel syndrome (CTS) in case of hand pins and needles sensation, and epicondylitis for forearm pain.
Similar to thoracic outlet syndrome, cervicobrachial syndrome involves identifiable vascular or neurological compression. However, unlike thoracic outlet syndrome, cervicobrachial syndrome presents with certain unexplained symptoms, resembling those seen in repetitive strain injury.
Diagnostic Procedures
Before initiating symptomatic treatment, it is necessary to complete the following diagnostic procedures:
- Conduct a thorough examination of the neck and shoulder to rule out any underlying causes. This includes a comprehensive physical examination.
- Perform X-ray imaging of the neck (cervical spine) in different directions to obtain a clearer understanding of the condition.
- Consult a neurologist who may recommend additional diagnostic tests such as electromyography (EMG) and magnetic resonance imaging (MRI) or computed tomography (CT) scans of the neck.
- Consider angiography or venography to assess for potential vascular injuries.
The purpose of obtaining radiographic images is primarily to exclude any objectively identifiable causes for the symptoms. These X-rays can help identify abnormalities in the first rib or the presence of accessory ribs. MRI or CT imaging is useful in evaluating spinal injury or pathology, both current and prior. EMG can assist in identifying or ruling out nerve damage. For assessing vascular injuries or thrombosis, conventional angiography, magnetic resonance angiography, or venography may be employed.
Outcome Measures
n patients with cervicobrachialgia, several measures can be employed to assess their condition:
- The Northwick Park Neck Pain Questionnaire can be used to evaluate the function of individuals. This questionnaire has demonstrated reliability in the short term and sensitivity to changes over the long term.
- Pain levels can be measured using the Short-Form McGill Pain Questionnaire (SF-MPQ), which includes the Present Pain Intensity (PPI) index and a visual analog scale (VAS). These tools provide a comprehensive assessment of pain severity.
- To evaluate physical outcomes, the cervical range of motion (CROM) can be measured. This helps assess the extent of mobility in the neck region.
For individuals experiencing wrist pain and disability, the Patient Rated Wrist Evaluation (PRWE) is a suitable tool. This questionnaire consists of 15 items and is designed to assess wrist pain and its impact on daily activities. It comprises two subscales:
- The pain subscale contains 5 items rated on a scale of 1 to 10. The total score ranges from 0 to 50, with higher scores indicating greater pain severity.
- The function subscale consists of 10 items divided into two sections: specific activities (6 items) and usual activities (4 items). The maximum score in this subscale is 50, with lower scores indicating better functional ability.
Physical Examination
To investigate and reproduce symptoms, various physical tests can be employed to aid in the diagnosis of cervicobrachialgia. These tests include:
- The Adson maneuver: The patient holds their breath while the physician observes for symptoms while tilting the head back and to the side.
- The elevated arm stress test: Symptoms may be induced by hyperabduction of the arm.
A loss of pulse during these tests may indicate thoracic outlet syndrome, which can contribute to cervicobrachialgia.
For assessing cervical radiculopathy, both chronic and acute problems, the following tests can be used:
- Shoulder abduction test: This test, along with the Spurling test, is specific for diagnosing cervical radiculopathy. It involves raising the arm to the side to provoke symptoms.
- Spurling test: This test helps identify cervical radiculopathy by reproducing symptoms through neck extension, lateral bending, and applying axial compression.
- Upper limb tension test: This test is more sensitive and can indicate cervical radiculopathy if positive. It involves stretching the upper limb nerves to assess their response.
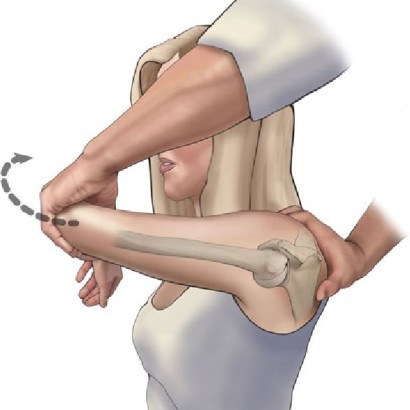
To assess the compliance and mechanosensitivity of neural tissues in the upper limb, the neural tissue provocation test (NTPT) can be performed using the median nerve. Regardless, the standard test needs 90° of shoulder abduction, which may be inconvenient for patients with cervicobrachial aches. In such cases, a modified NTPT test can be utilized.
Medical Treatment for Cervicobrachial Syndrome
The treatment approach for cervicobrachialgia is primarily conservative and focused on managing symptoms. Surgical interventions are not typically utilized for the treatment of cervicobrachialgia.
To alleviate pain and address sleep disturbances, medications are often prescribed. These may include painkillers, non-steroidal anti-inflammatory drugs (NSAIDs), and muscle relaxants, particularly for chronic pain. In cases involving vascular compression, vasodilators or calcium-channel blockers may be recommended by doctors.
Cervical epidural injections of corticosteroids can also be considered as a treatment option to reduce inflammation. These injections are effective in providing immediate and long-lasting pain relief, as well as improving range of motion and overall performance in individuals with chronic cervicobrachialgia.
Cervical epidural steroid injections administered in the posterior neck muscles are conservative treatments that yield prompt and prolonged effects. They alleviate pain, enhance range of motion, enable patients to reduce their analgesic medication dosages and facilitate a faster return to work compared to those who did not receive steroid injections.
A study involving two groups, namely the single injection group and the continuous injection group, evaluated the efficacy of epidural blocks. The single injection group received an epidural block with bupivacaine and methylprednisolone at intervals of 4 to 5 days, whereas the continuous injection group received continuous epidural bupivacaine every 6, 12, or 24 hours, along with methylprednisolone every 4 to 5 days. The continuous injection group demonstrated superior pain relief compared to the single injection group.
These treatment approaches aim to alleviate pain, reduce inflammation, and enhance functional outcomes for individuals with cervicobrachialgia. Healthcare professionals need to tailor the treatment plan based on the specific needs and conditions of each patient.
Physiotherapy Treatment
Manual physical therapy is an integral part of conservative treatment and has proven effective in managing pain, joint restrictions, and disability, especially when combined with therapeutic exercises. In a recent study, two types of traction, manual and mechanical, were compared.
In group A, mechanical traction was applied in a supine position using mechanical traction equipment. The traction force applied was 10-15% of the patient’s body weight, with a 10-second pull followed by a 5-second rest, repeated for 10 minutes in a single session.
In group B, manual traction was applied in a supine position with a 25-degree neck flexion. A 10-second pull followed by a 5-second rest was repeated 10 times in a single session. Further, the C-3 to C-7 elements were mobilized by prominent posteroanterior glide in a prone position, with each glide sustained for 5 seconds and repeated 10 times per session in both groups. Both groups were also advised to perform active range of motion exercises, stretching, and isometric strengthening training at home.
The study found that mechanical traction was more effective than manual traction in managing pain and disability in the treatment group.
Another study concluded that a combination of mechanical traction and exercises for patients with radiculopathy improved patient functioning and reduced pain. Similarly, Moretti et al. found that manipulative therapy for benign cervicobrachialgia of mechanical origin was more effective in both the short and long term.
Furthermore, combining mobilization with manipulation was found to have a small beneficial effect on patients who did not receive therapy.
Multimodal care, including mobilization, manipulation, and exercises, provided the best pain relief compared to only manipulation or manipulation combined with mobilization.
Physical therapy treatment for cervicobrachialgia includes various aspects:
- Conservative Treatment Goals:
- Reduction of pain through techniques such as transcutaneous electric nerve stimulation (TENS), cryotherapy, deep heat treatment, ultrasound, cognitive and behavioral pain management, and deep tissue massage.
- Improvement of function and range of motion through passive and indirect manual therapy techniques, manipulative physiotherapy treatment (e.g., cervical lateral glide mobilization technique), and active exercise therapy for the neck, shoulder, and arm.
- Exercises for Postural Control and Endurance:
- Teach patients correct posture and have them maintain it during activities of daily living (ADL). This is achieved through psychological recognition of incorrect posture, correction with feedback from the therapist, and progressively advancing to active exercises in lying and standing positions. The ultimate goal is to transfer these methods to functional everyday life situations, improving postural performance and reducing neck pain and dizziness.
- Cervical Mobilization:
- Effective treatment for cervicobrachialgia, particularly using a contralateral glide technique. It increases the range of motion in the upper limbs and reduces pain.
- The therapist cradles the head and neck, and performs a lateral translatory movement away from the involved side, minimizing gross cervical side flexion or rotation. Neural tissue provocation tests may be applied during the glide. Uncomfortable positions can be modified by positioning the patient’s arm in an unloaded position.
- Additional Therapies and Techniques:
- SNAGS (self-sustained natural apophyseal glide) delivers pain alleviation.
- Endurance exercises for the cervical-scapular region improve pain relief compared to no treatment.
- Combining cervical stretch, strengthening, and stabilization exercises has beneficial effects compared to no treatment, resulting in immediate pain reduction.
- Home exercises and ergonomic evaluation are important for rehabilitation, providing information about activities and positions at work that may aggravate the condition. Improvements were observed in pain intensity, pain quality scores, and functional disability levels.
- Using neck support while sleeping reduces the intensity of cervical spine pain. Recommending special pillows can help alleviate post-treatment complaints.
Conclusion
Multiple studies have explored various therapeutic interventions for cervicobrachial pain, including manual therapy, cervical traction, strength training, and postural control training. However, limited research exists with specific inclusion criteria. Future studies need to determine the categories of cervicobrachial pain that respond best to particular therapeutic interventions. By identifying these correlations, more targeted and effective treatment approaches can be developed.
FAQ
What is the cause of Cervicobrachial neuralgia?
Cervicobrachial neuralgia is an ordinary cause for rheumatologist consultation. It can be described as cervicalgia related to a radicular ache of the upper limb, induced by a nerve compression. The most regular reason is mild disc herniation.
What is a cervicobrachialgia diagnosis?
Diagnosis of cervicobrachialgia implicates a comprehensive clinical evaluation & diagnostic testing. Medical history: The doctor collects details regarding symptoms, like neck and arm aches, weakness, numbness, or tingling in the arm, as well as the medical history & earlier cervical spine damage.
How long can Cervicogenic last?
A “cervicogenic seizure” can last 1 hour to 1 week. Pain generally is on one side of the head, frequently connecting with the side of the neck where there is raised tightness. Nearly, the range of motion (ROM) will be reduced.
Is cervical a neuro problem?
Cervical radiculopathy also known as the pinched nerve is a illness that results in neurological dysfunction induced by compression & inflammation of any of the nerve roots of the cervical spine (neck). Neurological dysfunction can contain radiating pain, muscle weakness, and numbness.





3 Comments