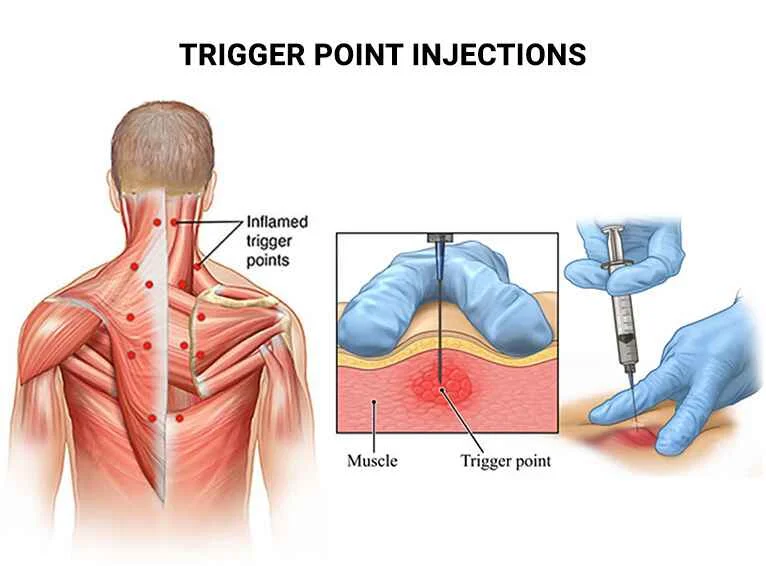
Trigger Point Injection
Myofascial discomfort is typically brought on by a “knot” or trigger point in your muscle and can be relieved with a trigger point injection (TPI).TPIs are widely used and usually safe.
Introduction
First determined by Dr. Janet Travell in 1942, myofascial trigger points are localized “knots” situated in a taut band of skeletal muscle. These are frequently palpable spots that, when palpated, create a characteristic referred pain along with local discomfort and, on occasion, a local twitch response.
In addition to producing stiffness and a reduction in range of motion, trigger points can occasionally be related to long-term musculoskeletal diseases. Stress on muscle fibers may result in the formation of trigger points following acute trauma or from repetitive microtrauma.
A common mistake is that tender spots are also known as trigger points. Tender spots suggest a localized nodule that created discomfort directly under the area of palpation; they are not the same as referred pain.
The patient’s musculoskeletal system might have one or more trigger points. Trigger points can be treated in several ways, such as with ultrasound, physical manipulation therapy, the Spray and Stretch method, and injections.
What are trigger point injections?
Myofascial pain, particularly in the arms, legs, neck, and lower back, can be relieved by a trigger point injection.
Painful “knots” in your muscles that may be extremely sensitive to pressure or contact are known as trigger points. They can occur as a result of repeated microtrauma or acute trauma that stresses the muscle fibers. It causes the muscle fibers to remain contracted. Rubs on the muscles can occasionally feel these knots.
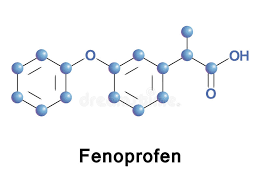
Injections of local anesthesia, either alone or in association with corticosteroids, botulinum toxin, or no injectable material at all (dry needling) are frequently used in trigger point procedures.
Injections of trigger points can be used to treat chronic muscle pain associated with myofascial trigger points, which are extremely sensitive fiber bundles found in tight muscle bands.
Treatment involves direct injection of medication into myofascial trigger points. Based on the degree and underlying cause of the pain, the doctor will choose the most appropriate medication.
Trigger point injections can involve:
- A local anesthetic that blocks muscle pain receptors, like lidocaine.
- An anti-inflammatory corticosteroid that decreases swelling in the muscle and connective tissue around a nerve.
- Botox, also known as botulinum toxin A, inhibits nerve signaling pathways and stops muscles from contracting.
During the process, the physician will inject the medication into a myofascial trigger point using a tiny needle.
When the doctor inserts the needle, people with taut muscles might experience a crunching sensation. Usually, as the muscle relaxes, this sensation goes away.
Anatomy and Physiology
The pathophysiology of trigger points appears to be associated with unusual motor end-plates in muscles where nociceptive and motor neurons coexist, as well as heightened central sensitization in the spinal cord. According to EMG research, trigger locations display spontaneous electrical activity, which may indicate the creation of aberrant action potentials.
The concept is backed by histological evidence from muscle biopsies that show hyper-contracture in the muscles, which is compatible with a continuous release of calcium from the sarcoplasmic reticulum as a result of brain activity and action potential production. Affected tissue may have a decreased range of motion and muscular tension as a result of the localized pain that patients may experience.
Trigger point injections are most frequently used to treat the quadratus lumborum, trapezius, levator scapulae, masseter, sternocleidomastoid, and temporalis muscles. Clinical symptoms of trigger points affecting the trapezius muscle include tension headaches, shoulder, and proximal arm pain. The main muscle responsible for trigger points causing pain in the groin area is the iliopsoas muscle.
Equipment
Materials for trigger point injections involve the following:
- Gauges 27 to 30 Acupuncture needles OR 1.5-inch needles are used for dry needling procedures.
- A syringe that holds 3, 5, or 10 milliliters.
- Generally non-sterile gloves.
- Anesthetic agent (optional): Lidocaine or bupivacaine devoid of adrenaline.
- To decrease discomfort, think about adding 5% sodium bicarbonate as a buffer.
- May involve a small amount of corticosteroid, such as triamcinolone.
- Take into consideration different prolotherapy solutions as sterile saline or D5W.
- Topical anesthetic spray, such as ethyl chloride, is optional.
- Consider including optional steroids in the local anesthetic mixture, such as dexamethasone or triamcinolone.
- skin-cleaning products such as 2% chlorhexidine or alcohol pads.
- A blood pressure monitor with a pulse oximeter.
Personnel
Trigger point injections can be carried out by healthcare providers with the required education and expertise, such as doctors, physician assistants, and nurse practitioners. It is suggested to have medical support personnel on hand to help with operation preparation.
What is the preparation of trigger point injection?
It is important to advise the patient about the advantages and disadvantages of trigger point injections. Due to the procedure starting, obtain written approval from the patient or guardian decision maker. Before starting the procedure, another member of the medical team should be available for a time-out and have equipment ready at the person’s bedside.
The patient may be in a seated or lying down position, depending on the location of the trigger point. Use alcohol pads or 2% chlorhexidine to clean the area, then let it dry. Before starting the operation, some therapists like to mark each trigger site with a skin marker or a retracting pen tip as a guide. Be sure to anesthetize the trigger points before starting the treatment if you plan to use a topical anesthetic spray.
Post-trigger point injection
Patients may use the affected muscle after having a trigger point injection, although they are advised to avoid strenuous exercise for a few days following the procedure. Within 24 to 72 hours following the injection, the majority of patients report feeling less discomfort. A month or more may pass before pain subsides.
Injections may need to be repeated to provide long-term pain relief. Patients may receive injections more frequently if the sole ingredient is anesthetic rather than steroid medicine. This is because using steroids raises the possibility of tissue injury.
What is the technique of trigger point injection?
The doctor should pinch the trigger point between their fingers to stabilize the tissue after identifying it and cleaning the area above it with their non-dominant index and thumb fingers. After sustaining the area, the clinician will needle the affected area rhythmically by repeatedly inserting and retracting the needle without fully withdrawing it from the muscle. They will do this using the dominant hand and insert the needle related to the 5 or 10-mL syringe into the trigger point at a 30-degree angle. The doctor should keep moving in different directions with this motion until the patient’s contractions stop or the muscle feels properly relaxed.
As the doctor inserts and retracts the needle into the strained muscle, a “crunching” or “pulling” sensation could be felt; this should subside during the therapy. Once the trigger point is relaxed, the point is finished being treated if dry-needling is used. If the clinician wants to use an injection, they should first aspirate to make sure the needle is not in a vascular structure before injecting 0.2 to 1 mL of the chosen solution into the spot.
You might take a direct or fanning approach. Repeat the previous procedures if treating more than one spot. Dry needling and local lidocaine injection produce similar effects; nevertheless, it has been demonstrated that local anesthetic administration is linked with reduced discomfort following needle placement. The use of ultrasonography for guided injection provided it is accessible and the physician is qualified, may be considered to check the intended structure and depth while avoiding neurovascular structures.
What happens during a trigger point injection procedure?
What to expect from a trigger point injection operation is as follows:
- You may be lying down on an exam table or seated, depending on where the trigger point is.
- Your doctor will use an alcohol pad to clean the affected area of your skin.
- Your physician might apply a skin marker at the trigger site.
- Your healthcare provider will press the trigger point between their fingers to stabilize the tissue after determining its location by tactile evaluation. You might feel awkward doing this.
- They will rhythmically continue needling the area by repeatedly inserting and retracting a small needle attached to a syringe into the trigger point, without fully removing the needle from the muscle or your skin.
- Your muscles will probably twitch or spasm. Until the muscle twitches stop or the area feels sufficiently relaxed, your physician will keep moving the affected area in different directions.
- After that, your healthcare professional will inject a local anesthetic—with or without corticosteroids or botulinum toxin—into the affected area.
- After the surgery, you will be allowed to return home.
How painful is a trigger point injection?
Although trigger points are usually uncomfortable to the touch, you may feel some discomfort while your healthcare professional locates the trigger point by hand before the injection.
When the needle and medication are inserted by your healthcare professional, you may feel stinging and burning. There’s a possibility that you’ll experience a momentary spike in pain as the needle tips the trigger point. Although it could hurt, this is a positive indication that the needle is in the right place.
Who needs to have a trigger point injection?
If other treatments, such as heat therapy, massage therapy, myofascial release, over-the-counter pain medication, physical therapy, or trigger point injections, have not relieved your trigger point discomfort, you might benefit from one.
To relieve the pain, physicians usually combine trigger point injections with physical therapy and stretches.
When a trigger point injection is used initially to treat pain in individuals who are unable to perform physical therapy or stretching because of severe discomfort, this tactic may be especially helpful. More effective physical treatment may result from the trigger point injection.
Your doctor needs to perform a complete physical examination and rule out other potential causes of your discomfort before recommending a trigger point injection. These other probable causes include:
- Muscle strain.
- pain’s structural causes.
- spinal stenosis, herniated discs, and degenerative arthritis are examples of conditions affecting the spinal column that can cause back discomfort.
- Radiculopathy relates to pinched nerve discomfort.
How common are trigger point injections?
About 85% of people will have trigger points and myofascial pain at some point in their lives.
Physical therapy, stretching exercises, trigger point injections, and/or physical therapy are common ways that primary healthcare practitioners and pain specialists assess and treat myofascial pain.
What can I anticipate following an injection of a trigger point?
You can return home after a trigger point injection and resume using the afflicted muscle. However, you should stay away from intense exercise during the initial days.
What are the risks of trigger point injection?
Although major problems from trigger point injections are uncommon, they can result in:
- Infection at the injection site.
- Bruising.
- Muscle or nerve damage.
- Rare accumulation of gas or air in the area between the lungs and the chest wall can lead to the collapse of one or both lungs.
A major trigger point injection problem can be reduced with the aid of ultrasound imaging.
What are the side effects of trigger point injection?
Trigger point injections can cause various immediate and long-term side effects, involving:
- Pain or temporary numbness in the vicinity of the injection site.
- The skin near the injection site is discolored or has dimpling.
- Lightheadedness or dizziness.
- Bleeding.
Furthermore, trigger point injections based on anesthesia may result in myonecrosis, a serious type of muscle injury. This could recover in three to four weeks.
After a few hours, the injection site’s nearby pain, swelling, and soreness normally go away. Consult your physician if any adverse effects do not go away after a few weeks of treatment.
What are the indications of trigger point injection?
A therapeutic approach for treating myofascial trigger points, particularly in symptomatic individuals, is trigger point injections (TrPi), which have shown progress in deactivating trigger points. It is suggested that they create a transient relaxation of the tense muscular cord, which facilitates better perfusion, ATP replenishment to release the actin-myosin chains that extend the muscle fiber, and metabolite waste disposal.
These elements support the disruption of the pain-tension cycle.
Trigger point injections are suggested when there is a palpable, painful location that results in a referred pain pattern. Prolonged or sporadic headaches, temporomandibular joint discomfort, back pain, restricted range of motion due to trigger points, and groin pain are common associated complaints.
What are the contraindications of trigger point injection?
Trigger point injection contraindications include the following:
Absolute:
- Patient refusal.
- Active infection over the site.
- Local open skull defect.
- TrP is not safely accessible by needle.
Relative:
Patients on anticoagulants, expectant patients, and patients with indistinct anatomical landmarks should all be treated with caution.
- In those who have a known allergy, avoid using local anesthetics.
- Severe fibromyalgia.
- History of keloid formation.
- Poorly controlled psychiatric disorder.
- The patient is highly anxious or needle-phobic.
What are the uses of trigger point injection?
Injections into trigger points may relieve pain associated with disorders affecting the nervous and musculoskeletal systems, like the ones listed below.
Many muscle groups, particularly those in the arms, legs, lower back, and neck, can be treated with TPI. TPI can also be used to treat tension headaches and fibromyalgia. The approach is also used to relieve myofascial pain syndrome, a persistent pain that affects the tissue around muscles and is unresponsive to normal therapies. TPI’s effect in treating myofascial pain is still being investigated, though.
Why trigger point injections are used
- Lower back.
- Neck.
- Arms.
- Legs.
Chronic pain in the aforementioned regions is commonly linked to:
- Poor posture.
- damage to the muscle.
- Poor mechanics cause the muscles to get stressed.
- Joint disorders.
Injections of trigger points are also utilized to alleviate pain related to specific health issues like:
- Fibromyalgia.
- Myofascial pain syndrome.
- Tension headaches.
Myofascial pain syndrome
Myofascial pain syndrome is a chronic pain condition that affects the muscles and surrounding tissue. Trigger point injections may help relieve its symptoms.
Trigger points in myofascial pain syndrome cause pain in seemingly unrelated body parts. We refer to this phenomenon as referred to pain.
Following the relaxation of the affected muscles, trigger point injections have been shown to alleviate localized muscle pain. It is thought that these injections disrupt the nerve signaling pathways responsible for referred pain.
Possible causes of myofascial trigger points involve:
- Injury or trauma to a muscle.
- Repetitive motions.
- Poor posture.
- Psychological stress.
A person who has myofascial pain may also feel the following symptoms in addition to referred pain:
- Pain in particular muscle regions.
- Pain that gets worse when the affected muscle is moved or stretched.
- knots in the person’s muscles that are tactile.
- Weakness or stiffness in the muscles.
- A restricted range of movement.
Fibromyalgia
Although it affects soft tissue rather than joints, fibromyalgia is a chronic pain disorder that has some symptoms similar to arthritis.
Although the specific cause of fibromyalgia is still unknown, the following are potential risk factors:
- An autoimmune condition like lupus or rheumatoid arthritis in the past.
- Trauma, either physical or mental.
- Fibromyalgia runs in the family.
- Infections.
- Being a woman.
Symptoms of fibromyalgia involve:
- Stiffness and pain all over the body.
- Headaches.
- Hand and foot numbness or tingling.
- Digestive problems.
- Fatigue during the day and poor sleep.
- Trouble focusing.
- Signs of anxiety or depression.
In the past, fibromyalgia was recognized by medical professionals in patients who complained of pain or soreness in particular body trigger points.
Fibromyalgia causes widespread, or systemic, pain as opposed to the localized pain felt in the muscles associated with myofascial pain syndrome.
This shows that neurological issues that affect the brain’s ability to process sensory data are the cause of fibromyalgia pain.
That means there are similarities in the pain profiles caused by myofascial trigger points and fibromyalgia, and some researchers think that myofascial trigger points are a factor in fibromyalgia pain.
Headaches
The American Migraine Foundation states that trigger points in the head, neck, and shoulders may aggravate tension-type headache disorders as well as migraines.
In a 2014 study, researchers examined the prevalence of myofascial trigger points in 20 physiotherapy students who experienced episodic migraine attacks and 20 healthy participants who did not experience migraine attacks.
The myofascial trigger point count was considerably higher in the migraineurs’ group, according to the researchers.
Myofascial trigger points and pressure pain sensitivity in individuals with episodic or chronic tension headaches were studied by the authors of a 2016 study.
The pressure sense for pain was higher in those with more myofascial trigger points than in those with fewer points. According to the research, myofascial trigger points may have an impact on how severe certain headaches are.
When do patients need a trigger point injection?
When a patient has pain radiating from a trigger point to the surrounding area, trigger point injections are performed. Myofascial pain syndrome and fibromyalgia are two ailments that may be treated with trigger point injections. On the other hand, trigger sites frequently reoccur in chronic pain syndromes.
What are trigger point injections used for?
Trigger point injections are one way that medical professionals manage myofascial pain. Muscle is referred to as “myo,” and fascia as “fascial.”
The thin, white connective tissue that envelops each muscle in your body is called fascia.
In myofascial pain, one or more trigger points are usually the cause of the pain and tenderness. Trigger points in your muscles are tactilely similar to little lumps, nodules, or knots.
Though trigger points can form in any muscle, trigger point injections are most frequently used to treat those muscle groups:
- Masseter (a muscle in your jaw).
- Muscles on either side of your neck: levator scapulae.
- Gluteus medius (a muscle in your hip).
- Your deepest low back muscle is called the quadratus lumborum.
- The muscle that runs across your shoulders and back of your neck is called the trapezius.
- The muscle in the front of your neck is called the sternocleidomastoid.
- One of your head’s side muscles is called the temporalis.
Certain kinds of discomfort or problems can be called on by trigger points. Tension headaches, for instance, might be brought on by trigger points that impact your trapezius muscle.
Piriformis syndrome can be brought on by a trigger point that affects the piriformis muscle, which presses against the sciatic nerve in your buttocks. Your buttocks and the back of your leg hurt or get numb from it.
What are the benefits of trigger point injections?
People who have been experiencing pain associated with trigger points and have not found relief with more conservative therapies, such as over-the-counter pain medication or physical therapy, may find relief with trigger point injections, which are generally safe.
Depending on the weakened muscle, trigger point injections can also result in a noticeable increase in general muscle functionality and range of motion.
What is a complication of trigger point injection?
Complications of trigger point injections involve the following:
- Pain.
- Bleeding.
- Infection.
- Reaction to the anesthetic agent that is allergic.
- Systemic anesthetic toxicity.
- Hemostasis formation.
- Vascular injury.
- Although they are rare, there have been reports of side effects like pneumothorax, especially with needling trigger points in the cervicothoracic area.
- The use of a pincer grasp is advised for trigger points along the thoracic cage to move affected tissue away from the intercostal gaps. The risk of entering the pleura may also be reduced by using a tangential vector as opposed to a vertical one.
- There has also been one case report of severe hypokalemic paralysis.
- The dry-needling considered has side effects such as post-treatment discomfort, vasovagal and syncopal reaction, treatment-site hemorrhages, and acute cervical epidural hematoma.
Do they work?
People with chronic muscle pain might realize that trigger point injections provide instant pain relief and improved range of motion.
All people are not affected by these injections in the same way, though. Some patients find that their pain significantly subsides within a few days or weeks of receiving the injections, while others may require more time.
Trigger point injections are completely ineffective for certain individuals.
Researchers examined the effects of these injections in patients with abdominal muscle pain in a small 2019 study. Two years after the first injection, participants reported noticeably less pain. A total of five individuals required an extra injection, and one did not respond to the treatment.
Although some people may benefit greatly from trigger point injections, other researchers have discovered that this treatment may not always work.
How frequently will patients need trigger point injections?
A trigger point should ideally resolve with a single injection. This could happen if a patient has a single isolated trigger point, particularly if the trigger point’s underlying cause has been eliminated (such as a trigger point set on by a mild trauma that happens repeatedly or a movement that the patient would no longer execute). Trigger points caused by long-term illnesses like myofascial pain syndrome and fibromyalgia frequently repeat because of the underlying issue.
Trigger point injections can then be given either frequently or just as necessary in certain situations. The medication being injected determines how frequently trigger point injections are administered. The injections can be given as continuous therapy as often as once a month if just lidocaine or a combination of anesthetics is used. TPIs should be given far less frequently when a steroid medicine is injected, at the treating physician’s discretion, due to the possibility of tissue damage or shrinkage from the steroid treatment.
Trigger Point Injection for Pain Management
Some people can profit from trigger point injections (TPI) as a form of pain management. Trigger points, or knots of muscle that form when muscles do not relax, are treated with TPI to alleviate pain in certain locations of the body. These knots are frequently felt beneath the skin. Pain produced in another region of the body, or pain felt in the vicinity of a trigger point, might result from irritation of nearby nerves.
What Happens During a Trigger Point Injection?
A tiny needle is inserted by a medical expert into the patient’s trigger point during the TPI process. The injection may also contain a corticosteroid as well as saline or a local anesthetic. The trigger point is rendered dormant by the injection, which also reduces pain. A rapid course of treatment will frequently provide long-lasting relief.
Typically, injections are administered in a doctor’s office and take a few minutes. In one visit, several areas might receive injections. In cases where a patient is allergic to a particular treatment, a dry needle considered without medication can be employed.
How long do trigger point injections last?
Between 24 to 72 hours following the trigger point injection procedure, the majority of patients report feeling less discomfort. Usually, pain alleviation lasts for approximately one month. Your doctor may recommend more injections if the pain persists after this point to give long-term pain relief.
When should I see my healthcare provider?
Make in touch with your doctor if you’ve had a trigger point injection and you’re showing symptoms of infection, including fever or warmth where the injection was given.
Injections for trigger points are a popular and typically safe treatment for trigger point-related myofascial pain. The injection can provide pain relief for almost a month, if not longer, even though the process may be uncomfortable initially.
Consult your healthcare provider about trigger point injections if you have a muscle knot that isn’t going away with conservative measures like taking painkillers. They can react to all of your inquiries.
Clinical Significance
Many primary-care doctors and pain specialists often diagnose and treat musculoskeletal pain, which is a common complaint. Having a multimodal approach to pain treatment is crucial to giving patients safe and efficient outcomes. When applied as a primary or supplemental treatment, trigger point injections have the potential to decrease musculoskeletal pain.
Clinicians can treat pathologic tissue directly, address the cause of a patient’s discomfort, and break the pain cycle with minimal to no side effects by focusing on specific myofascial pain sites.
Without the need for painkillers, patients might see a noticeable improvement in their general functionality and range of motion. Trigger point injections can provide significant outcomes, so in the right situation, they should be taken seriously as a therapeutic option.
Summary
For chronic discomfort such as myofascial pain syndrome, fibromyalgia, and tension-type headaches, trigger point injections may be a safe therapy option. The injections are given straight into the injured muscle by a physician or other medical professional. A corticosteroid, a local anesthetic, or botulinum toxin A may be injected.
Some people may have immediate pain relief from trigger point injections, but others may not respond to the procedure. More specific information regarding the advantages and disadvantages of this treatment can be obtained from a physician.
FAQs
How long do trigger point injections last?
The duration of trigger point injection benefits varies based on the patient’s condition and the medication given. It might last for several days to several months. Many patients have a certain number of shots spaced one or two weeks apart. With time, the interval widens and the frequency progressively drops.
Is trigger injection painful?
The medication will be injected into the trigger point using a needle that has been inserted into your skin. As the needle is put into the trigger point, you can twitch and feel some pain. There may even be a slight burning or crushing sensation noticed by those with really strained muscles.
How much do trigger point injections cost?
You ought to prepare between $250 and $450 for trigger point injections, while the exact amount will depend on your region, the provider you select, and how many shots you require.
Is trigger point therapy painful?
Only while pressure is being given to the delicate area during trigger point therapy may it be unpleasant. Trigger point therapy can help reduce persistent discomfort and spasms in the muscles. After a session, you should notice an improvement even if you might not feel relief right away.
Is trigger point injection safe?
Injections at trigger points are generally safe and have a minimal chance of consequences. Temporary soreness or numbness around the injection site is the most frequent adverse effect. Acetaminophen (Tylenol®) or ibuprofen (Advil®) may be given by your healthcare practitioner to address this.
How many injections are for the trigger point?
To get the most pain relief, most doctors recommend getting one injection every eight weeks for six months.
Are trigger shots expensive?
To stimulate ovulation, a “trigger shot” is often (but not always) given and can cost from $50 to $250. Blood tests and monitoring: These processes help your doctor ensure that while follicles (which contain eggs) are growing, they are not doing so at a pace or speed that could endanger multiple gestation births.
How successful is a trigger shot?
With no trigger shot and IUI, the pregnancy rate was 5.8%. This percentage increased to 18.2 percent with the trigger shot. Furthermore, the impressive 30.8 percent pregnancy rate was achieved when the trigger shot was timed to coincide with the woman’s natural spike in LH. An earlier study carefully examined the shot time.
How quickly do trigger point injections work?
Injections into the trigger points can provide immediate pain relief. Many people report feeling less discomfort right away after receiving an injection. For some, the full effects may not become apparent for days or weeks.
Who needs trigger point injections?
Trigger point injection indications include a painful location that results in a referred pain pattern. Chronic or sporadic headaches, temporomandibular joint discomfort, back pain, reduced range of motion due to trigger points, and groin pain are common concurrent complaints.
What type of doctor gives trigger point injections?
Trigger point injections are a skill that Ortho Sport and spine Physicians’ pain experts possess a great deal of experience with.
Are trigger point injections permanent?
Additionally, tension headaches and fibromyalgia can be treated with trigger point injections. A trigger point injection (TPI) may be a long-term remedy for your trigger point, or it may just provide temporary pain relief for a few weeks or months, depending on what caused it.
Can trigger points be cured?
Trigger points are rendered inactive by a variety of techniques, which involve the Spray and Stretch method, ultrasound, manipulative treatment, and injection. It’s been demonstrated that one of the best ways to deactivate trigger points and quickly relieve symptoms is through trigger-point injection.
Who should not get trigger point injections?
It is not suggested to inject trigger points while a local or systemic disease is present. Patients with bleeding disorders or those taking anticoagulants need to have their injections administered under strict medical supervision.
What can go wrong with trigger point injections?
There’s a possibility that the fat beneath the skin may shrink if a steroid medicine is injected into the trigger point, causing a dent in the skin. When anesthetic alone is given without any steroid medicine, this does not happen.
What happens after trigger point injections?
Patients who get trigger point injections can use the treated muscle but should avoid strenuous activity for a few days following the procedure. During 24 to 72 hours following the injection, the majority of patients report feeling less discomfort. A month or more may pass before pain subsides.
Can you get a massage after trigger point injections?
Given the combination of these therapies enables us to work as a team to provide our patients with a better solution for their myofascial muscle discomfort, trigger point injections are typically done before physical therapy or massage therapy.
Do you need anesthesia for trigger point injections?
A small needle is inserted by a medical professional into the patient’s particular trigger point, which is a muscle spot, during the trigger point operation. Usually, only a local anesthetic is injected. Without the need for sedation, this treatment can be carried out in a physician’s office.
Can trigger point injections hit a nerve?
Patients with headaches, low back pain, and other musculoskeletal and systemic diseases have been related to trigger point injections. Injectate deposition straight into the nerves feeding the area is a possible side effect of several of these injections.
Is an MRI required before receiving trigger point injections?
Trigger points aren’t seen on MRIs or X-rays, thus imaging is not required to diagnose one. These tests, however, may be beneficial if the trigger point is brought on by an underlying medical problem. During one visit to your doctor, many trigger points can be injected.
What is the maximum number of trigger point injections?
By medical advice, the injections are only administered repeatedly. A maximum of six trigger point injections is advised for the treatment of severe pain. But not every trigger point injection includes steroids. It is possible to give trigger point injections more frequently if they just include a local anesthetic.
Can you walk after trigger point injections?
After your trigger point injection, you will be able back to your work and exercise routine the next day. Because the steroid drug could irritate the nerves, some patients report experiencing more pain than usual following their trigger point injections after the anesthetic wears off.
Who should not get trigger point injections?
It is not suggested to inject trigger points while a local or systemic disease is present. Patients with bleeding disorders or those taking anticoagulants need to have their injections administered under strict medical supervision.
Who needs trigger point injections?
Trigger point injections are suggested when there is a palpable, painful location that results in a referred pain pattern. Chronic or sporadic headaches, temporomandibular joint discomfort, back pain, reduced range of motion due to trigger points, and groin pain are common concurrent complaints.
What happens after trigger point injections?
Patients are asked to avoid strenuous exercise for a few days following a trigger point injection treatment, although they are still able to use the treated muscle. Within 24 to 72 hours following the injection, the majority of patients report feeling less discomfort. A month or more may pass before pain subsides.
Is a trigger point injection a steroid?
Since the pain is frequently coming from many trigger points, these can be marked with a pen. The skin will be cleansed using an alcohol-based solution when detected. A combination of bupivacaine, a numbing agent, and a tiny quantity of steroid is subsequently injected into the trigger points.
Do trigger point injections have side effects?
Pain after an injection of a trigger point is one possible side effect of this technique. This isn’t extremely often, but it can happen. Usually, it disappears on its own in a few days. When no medication is administered to the trigger point (dry needling), it occurs more frequently.
Can trigger point injections raise blood pressure?
In rare cases, an injection could make you feel worse for a while. You can get flushed or feel more hungry, have hiccups or cramps in your muscles, or experience increased pressure at the injection site. Blood pressure or blood sugar elevation may persist for a maximum of two weeks after the injection.
What disease is treated by trigger point injections?
Medications, trigger point injections, or physical therapy are commonly used in the treatment of myofascial pain syndrome.
What can I do instead of trigger point injection?
There exist multiple alternative methods for managing pain, such as:
Physical Therapy: A mix of stretches and workouts intended to increase affected areas’ flexibility, strength, and mobility.
Medications: pharmaceuticals or over-the-counter drugs can help control inflammation and pain.
Reference
- Hammi, Claudia. “Injection at Trigger Point.” Go to books/NBK542196/#:~:text= at www.ncbi.nlm.nih.gov.Trigger point injections are a safe and dependable method of treating StatPearls, July 24, 2023 – NCBI Bookshelf.
- Image-Redirect Notice. www.google.com/url?sa=i&url=https%3A%2F%2Fwww.thespineandrehabgroup.com%2Ftrigger-point-injections&psig=AOvVaw3lixuT1V6sUYmqXPYqUvow&ust=1704781490923000&source=images&cd=vfe&opi=89978449&ved=0CBIQjRxqFwoTCPDRh46UzYMDFQAAAAAdAAAAABAe.
- Professional, Cleveland Clinic Medical. “Trigger Point Injections.” Cleveland Clinic, my.clevelandclinic.org/health/treatments/17582-trigger-point-injection.
- “How to Treat Pain with Trigger Point Injections.” February 2, 2005, accessed from WebMD, www.webmd.com/pain-management/trigger-point-injection.
- Eske, Jamie. Everything You Require to Know About Trigger Point Injections. 24 Dec. 2019, www.medicalnewstoday.com/articles/327384#do-they-work.
- Driver, Catherine Burt. “Side Effects from Trigger Point Injections and Medication.” MedicineNet, www.medicinenet.com/trigger_point_injection/article.htm; July 30, 2020.
- Trigger Point Injections in Washington DC, Baltimore, Maryland, Virginia | MedStar Health. www.medstarhealth.org/services/trigger-point-injections.



One Comment