Tuberosity of the Tibia
Introduction
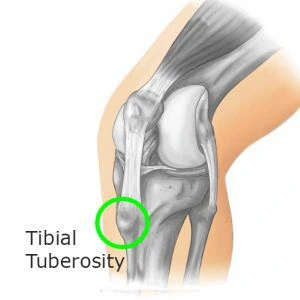
The proximal, anterior portion of the tibia has an elevation called the tuberosity of the tibia, also known as the tibial tuberosity or tibial tubercle. It is easily palpable as the patella’s inferior protrusion. The infrapatellar bursa, which is subcutaneous, lies beneath the tibial tuberosity. It defines the beginning of the anterior border of the tibia and serves as a limit for the intercondylar region in the anterior direction. The medial and lateral tibial condyles’ surfaces come to an end. The patellar ligament, commonly known as the common quadriceps tendon, has its inferior insertion at the tibial tuberosity.
The tuberosity develops in four distinct stages: cartilaginous, apophyseal, epiphyseal, and bony. As the growth plate merges in late adolescence, typical Weaker columnar cartilage takes the place of the fibrocartilaginous components. The tibial tuberosity is roughly 3 cm distal to the proximal at full skeletal development. articulating the surface of the tibia. It acts as a lever to extend the knee joint and serves as an attachment for the patella tendon.
The upper smooth and lower rough portions of the tibial tuberosity can be separated. The rough area is positioned subcutaneously and is separated from the skin by an infrapatellar bursa, whereas the smooth area acts as the ligamentum patellae or quadriceps tendon attachment site. A large bony protrusion on the front of the proximal tibia. acts as the attachment site for the patellar ligament.
Functions of Tuberosity of the Tibia
The major function of the tibia is to transfer and distribute weight from the foot to the ankle and up the leg to the knee. To keep the tibia in the right position, the comparably non-weight-bearing fibula and tibia articulate.
The tibial tuberosity acts as the tip of a large structure that stretches the knee joint and prevents it from collapsing when the foot strikes the ground as a result.
Structure of Tuberosity of the Tibia
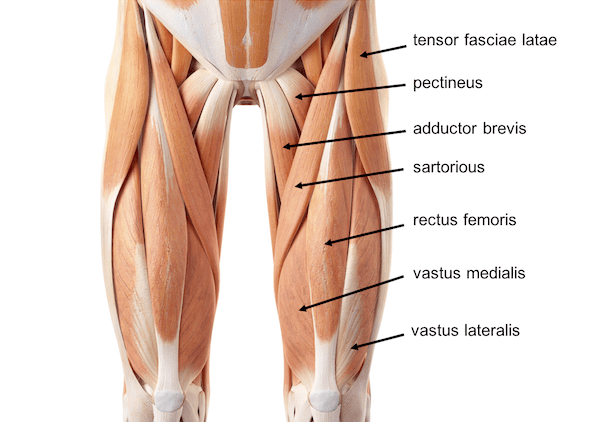
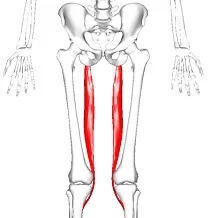
The tibial tuberosity is connected to the patellar ligament, which attaches to the patella from where the suprapatellar ligament creates the quadriceps femoris muscles’ distal tendon. The quadriceps is made up of four muscles: the rectus femoris, vastus lateralis, vastus medialis, and vastus intermedius. The femoral nerve supplies the quadriceps muscles with its fibers. The tibial tuberosity acts as the tip of a large structure that stretches the knee joint and prevents it from collapsing when the foot strikes the ground as a result. The tibial tuberosity, the patella, and the two ligaments can all be seen as surface-level structures.
Although tibial tuberosity lesions are extremely uncommon, their odd position and appearance can make them difficult to diagnose. Even though various disorders that affect this area are frequently encountered elsewhere in the bone, when they occur at the tibial tuberosity, they may have unusual imaging presentations and morphological characteristics. The current analysis discusses the stages of the tibial tuberosity’s development, elucidating why this region is vulnerable to degenerative tractional changes and damage. It also significant a number of pathologies, including benign and malignant osseous lesions, as well as anomalies that are associated with trauma and degenerative changes.
Blood supply
An arterial network that was primarily fed by the anterior tibial recurrent artery vascularized the tibial tuberosity. the popliteal artery’s branches or other arteries were also involved in supplying blood to the tibial tuberosity.
Clinical significant
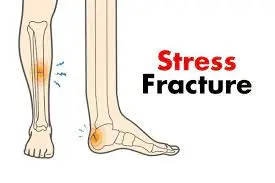
Fractures
Tibial tuberosity fractures, which are infrequent fractures, most usually affect teenagers. Tuberosity apophysis avulsion fractures may result from excessive knee flexor contractions during running and jumping exercises. Only a cast is required if the fragment is left in its normal place on the tibia. However, to restore normal function if the fracture fragment is displaced, surgery is necessary.
Tenderness in the tibial tuberosity can be brought on by Osgood-Schlatter disease or deep infrapatellar bursitis. A bony protrusion on the tibial tuberosity may be the result of ongoing Osgood-Schlatter irritation in a teenager with open growth plates or what is left of Osgood-Schlatter in adults.
Differential diagnosis
In addition to OSD, other illnesses like Sinding-Larsen-Johansson syndrome, Hoffa’s syndrome, soft tissue or bone tumors, patellar tendon avulsion or rupture, chondromalacia patella, patellar tendinitis, infectious apophysitis, accessory ossification centers, osteomyelitis of the proximal tibia, and tibial tubercle fracture should be taken into consideration.
FAQs
How does tibial tuberosity happen?
Like OSD, tibial tuberosity avulsion fractures result from a sudden contraction of quadriceps muscles placing severe strain on the patellar tendon which overcomes physical strength. This mechanism becomes more prevalent in the later years of adolescence and is violent
How do you prevent tibial tuberosity?
Modifying physical activity, and utilizing ice packs, NSAIDs, braces, and pads are all examples of conservative treatment. Symptoms usually disappear after the physis closes without any medical intervention, but in some cases, symptoms might still exist.
Is there a growth plate on the tibial tuberosity?
The tibial tuberosity’s growth plate is structurally distinct from most growth plates and does not form until several months after birth. Most growth plates are loaded primarily in compression. It differs significantly from the adjacent proximal tibial growth plate histologically.
How old must you be for the tibial tuberosity to fuse?
(11 years old) The tibial tubercle’s whole structure is cartilage. Apophysis develops between the ages of 11 and 14. Ages 14 to 18 are when the apophysis merges with the proximal tibial epiphysis. The proximal tibial epiphysis and tibial tubercle apophysis fuse when a person turns 18 years old.
What does the tibial tuberosity bump represent?
The tendon from the knee cap enters into this lump, which is known as the tibial tuberosity. Males are more likely to have Osgood-Schlatter disease, which often affects children between the ages of 10 and 15 and manifests during a time of fast growth.