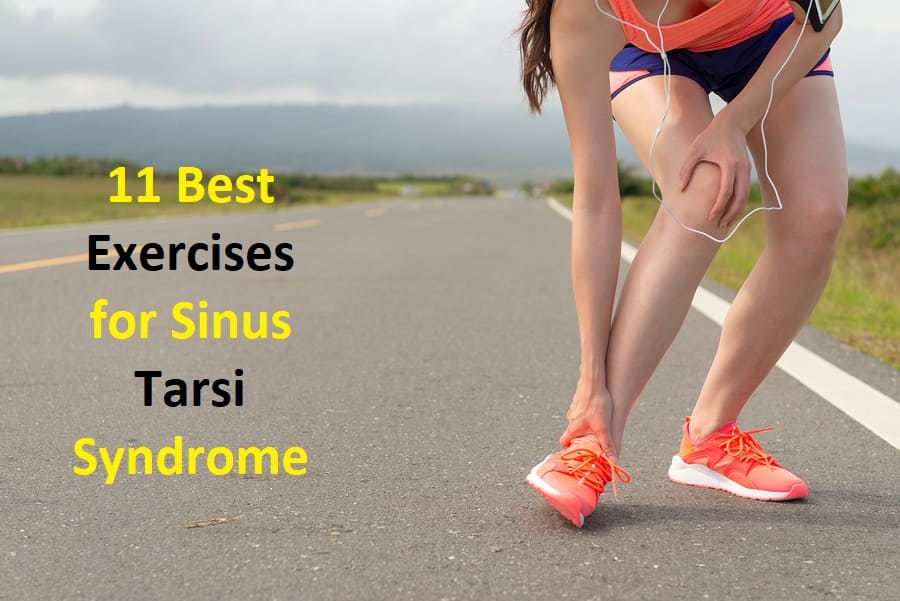
11 Best Exercises for Sinus Tarsi Syndrome
When dealing with Sinus Tarsi Syndrome (STS), incorporating appropriate exercises into your rehabilitation routine can be instrumental in managing symptoms and promoting healing. STS is a condition characterized by pain and tenderness in the sinus tarsi region of the ankle, often resulting from overuse, biomechanical imbalances, or prior ankle injuries.
Exercise can play a pivotal role in addressing the underlying causes of STS, such as weakened ankle stabilizers, compromised biomechanics, and decreased range of motion. The right exercises can help enhance ankle strength, improve proprioception (awareness of joint position), and restore flexibility—all of which are crucial for a balanced and pain-free gait.
However, it’s important to note that the effectiveness of exercises can vary depending on individual factors, such as the severity of your STS and any associated conditions. Therefore, before starting any exercise regimen, it’s advisable to consult a qualified healthcare professional, such as a physical therapist or orthopedic specialist, to receive a personalized exercise plan tailored to your specific needs.
In the following sections, we will explore some of the exercises commonly recommended for individuals with Sinus Tarsi Syndrome. Remember that these exercises are intended to serve as a general guideline and should be performed under the guidance of a medical professional to ensure their appropriateness and safety for your condition.
Introduction:
Between the talus and calcaneus bones is a tube or tunnel called the sinus tarsi. Illness or pain in this region is known as sinus tarsi syndrome. The main reasons for this syndrome are trauma to the ankle or foot (such as an ankle sprain) or overuse (such as prolonged standing or walking).
Additionally, the sinus tarsi may compress if the person has pes planus or an overpronated foot. Some signs include pain on the lateral side of the ankle, near the lateral malleolus, as well as difficulties walking on irregular surfaces or a sense of instability.
According to current analyses of sinus tarsi syndrome (STS), this condition is principally characterized by subtalar joint instability brought on by ligamentous injuries that induce synovitis and the infiltration of fibrotic tissue into the sinus tarsi area.
Causes and risk factors
- Some experts evaluate that roughly 70–80% of cases of sinus tarsi syndrome are the result of ankle sprains or the ankle rolling outward.
- 20–30% occur due to excessive foot pronation, or rolling inward, and may occur over time.
- Flat feet
- Pressure on the subtalar joint
- Aarthritis in the subtalar joint
- Joint instability
- Scar tissue
- Repeated injury to the area
Symptoms
- Pain or discomfort
- swelling around the ankle and heel
- Instability
Pain typically appears on the exterior of the foot in the back below the ankle joint. Weight-bearing exercises, including walking on the joint, can induce a worsening of symptoms.
A person may also detect improved pain when bending the foot inward or outward. The pain may happen when sitting, standing, or walking. When sinus tarsi syndrome occurs, a person may have trouble walking on uneven floors, such as grass or gravel. They may feel unsteady when walking or as if their foot may give out on them.
Physiotherapy Treatment :
The foot has been immobilized by a brace or tape during the healing of the joint and the ligaments because the STS frequently follows an ankle sprain.
As a result, STS requires mobilization of the ankle, particularly the subtalar and talocrural joints. Exercises for joint mobilization should be performed in all directions, although pronation and supination are especially important. Also important is they should be executed at full range of motion, provided there is no pain impulse. There are no available random control trials for the effectiveness of STS rehabilitation programs.
The therapy may include friction massages, electrotherapy (such as ultrasound), laser therapy, cryotherapy, and other sorts of deep massages to affect the tissues in the sinus tarsi. To reduce swelling and pain, applying cold massage to the lateral ankle may be helpful.
If an activity can be performed without pain, it should be started as soon as feasible. It’s necessary to modify a program therapy to strengthen those muscles since when you have sinus tarsi, your peroneal muscles and Achilles tendon tend to weaken.
Standing on your toes while flexing your ankle is a good exercise and eccentric activities can be performed for greater strength gains when done on the edge of a stairway.
The final phase of therapy is stability training.
To enhance proprioception and ankle stability, the patient must perform proprioceptive exercises like lunges. The cornerstone of STS treatment plans will be exercise regimens that improve lower extremity function and subtalar joint stability.
Passive joint structures, dynamic muscle actions, and neurological regulation are all necessary for joint stability. The STS therapy plan includes a variety of activities, including muscle-strengthening routines, proprioceptive training, balance training, taping and bracing, and others.
Anti-inflammatory drugs can assist in lessening inflammation in athletes who have synovitis of the joint. Ice applied to the affected area might also be beneficial.
Sinus tarsi syndrome exercise and criteria for progressions
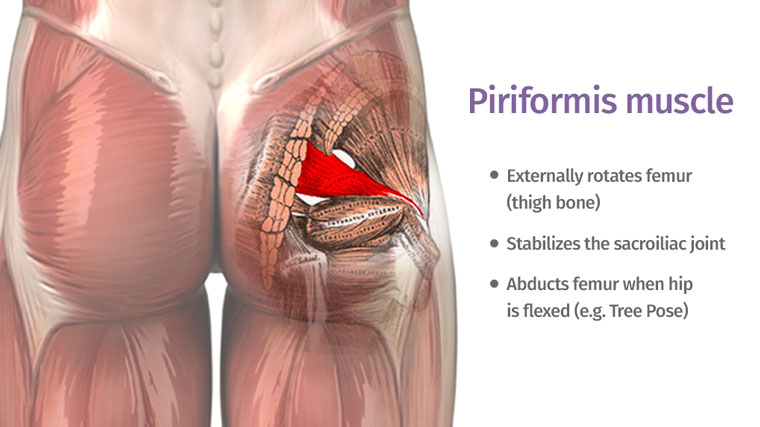
Stability Training: The basis of STS treatment plans will be exercise regimens that enhance lower extremity function and subtalar joint stability. Passive joint structures, dynamic muscle actions, and neurological regulation are all necessary for joint stability.
Given that it is believed that rips or ruptures of the interosseous and cervical ligaments of the subtalar joint are the primary lesions that cause STS, the focus will need to be placed on the dynamic muscle reflexes and neurological control of the rearfoot to make up for the loss of passive stability.
As force transducers direct and regulate the pronation and supination motions of the subtalar joint, the muscles that span the subtalar joint are crucial for preserving stability.
Although the relative strength of these muscles matters for STS recovery, their responsiveness to joint perturbations and capacity for coordinated movement is even more crucial.
To make up for the loss of proprioceptive information from the stabilizing ligaments of the joint, dynamic stability will additionally rely on the proprioceptive information from the muscle spindles and Golgi tendon organs of these muscles.
Maintaining stability via extended periods of exercise or athletic activity will also depend on the muscles’ endurance.
The development of joint stability has been referred to as a multiphase process that starts the athlete at a suitable level of activity and progresses to higher levels of exercise while preserving joint stability.
The three phases of the progression—attain, maintain, and sustain—help the athlete comprehend this process.
The postures or positions the athlete may successfully achieve will be determined in the Attain phase.
Coordinated isometric and eccentric muscular contractions of the muscles spanning the joint will be developed during the maintenance phase.
All of the neuromuscular subsystems that are required for stability during sports-specific activities will be integrated during the sustain phase.
Attain stage :
Activities: Standing on one leg with both eyes open and closed.
Single leg standing
Criteria for Progression :
The performer demonstrates how to support oneself using the foot and ankle.
Maintain stage :
Activities :
Standing on one leg while performing hip swings and star pattern reaching. The heel raises oscillation with theraband and impulse with a medicine ball.
single leg standing
heel raise
Sustain stage :
Activities:- Lunges and step-down exercises, step-up exercises,
Bilateral and single-leg hops
Forward and backward acceleration and deceleration
Pivoting and cutting maneuvers
Exercises for sinus tarsi syndrome
Patients with this illness are frequently advised to perform the exercises listed below. Before starting these workouts, you should talk to your physiotherapist about their suitability. In general, they should be done three times a day, and only if they don’t worsen or bring on symptoms.
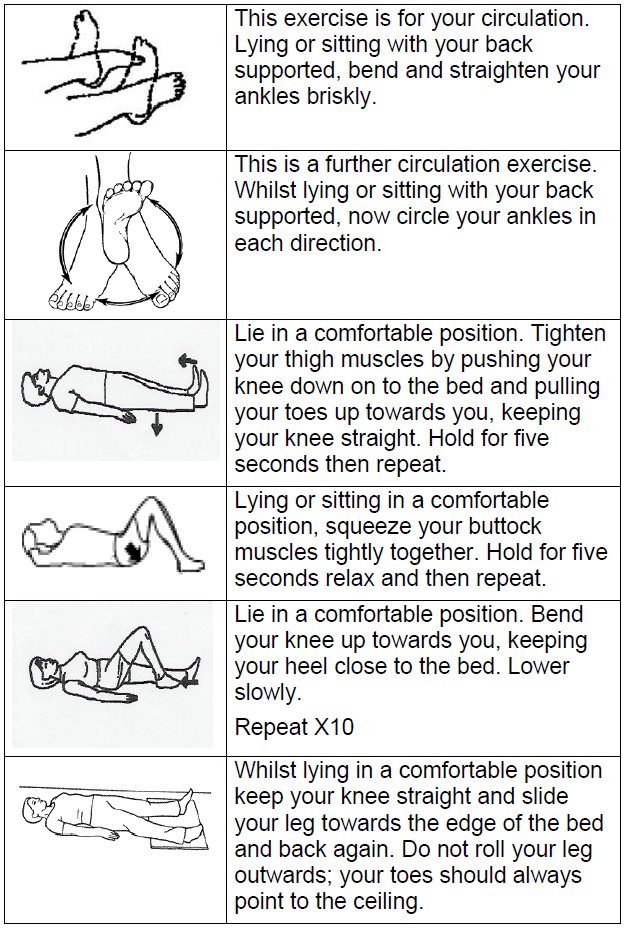
Foot and Ankle Up and Down
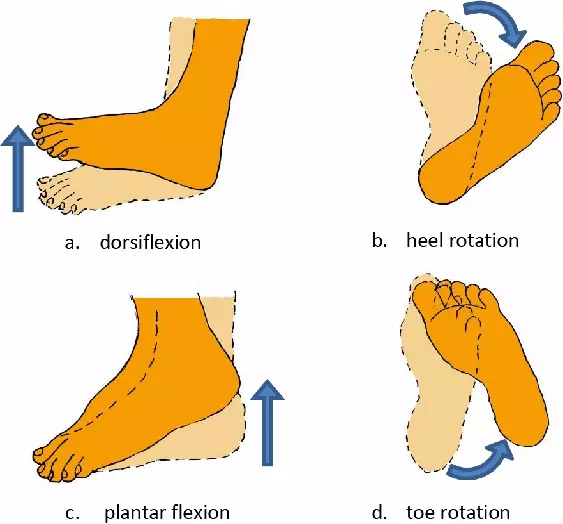
This exercise is also known as dorsiflexion and plantarflexion. As far as it is comfortable and pain-free, move your foot and ankle up and down (figure 3). As long as the symptoms don’t worsen, repeat 10 to 20 times.
Left leg, up and down foot and ankle
Foot and Ankle In and Out
This exercise is also known as Eversion and inversion. As far as it is comfortable and pain-free, move your foot and ankle in and out. Repeat 10 to 20 times as long as the symptoms don’t worsen. (Right leg) Foot and Ankle In and Out.

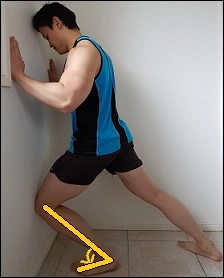
Lunge Stretch
Put your stretched leg in front of you as shown, and lean your hands against the wall. Do not lift your heel. As far as you can comfortably do so without experiencing pain, gently move your knee forward over your toes. If symptoms do not worsen, hold for 5 seconds, then repeat 10 times at a mild to moderate stretch.
Right lunge stretch
Soleus Stretch for Sinus Tarsi Syndrome
- the injured leg behind you as you stand up straight.
- While bending your back leg, keep your heel on the ground.
- A pull on the rear of your leg should cause you to stop and hold.
- 45 seconds of holding
- 3–4 times each day, repeat.
Please halt this exercise if you experience any pain in the front of your ankle.
Gastrocnemius Stretch for Sinus Tarsi Syndrome

- the injured leg behind you as you stand up straight.
- Keep the front knee slightly bent while keeping the back knee straight.
- Continually advance on the front leg while maintaining both heels on the ground.
- Once your back leg starts to feel stretched, stop pushing forward.
- 45 seconds of holding
- 3–4 times each day, repeat.
- Please discontinue this exercise if you experience any pain in the front of your ankle.
Posterior Tibialis Strengthening for Sinus Tarsi Syndrome

- Place the injured ankle on the opposing knee while seated.
- Put a bandage on each foot.
- The injured foot’s toes should be pointed, and they should be lifted against the band’s resistance.
- To finish one repeat, slowly retrace your steps to the beginning position.
- Yellow for the band
- 15 repetitions, 3 sets.
- Periodically: once every day
Peroneal Muscle Strengthening For Sinus Tarsi Syndrome

- In a chair sitting position place your both foot firmly on the floor.
- Wrap a bandage around each foot. Evert (turn the affected foot outwards) while fighting the band’s resistance.
- To finish one repeat, slowly retrace your steps to the beginning position.
- Band the shade of yellow
- 15 repetitions, 3 sets.
- Periodically: once every day
- Please discontinue this exercise if you experience any pain in the front of your ankle.
Calf Stretches
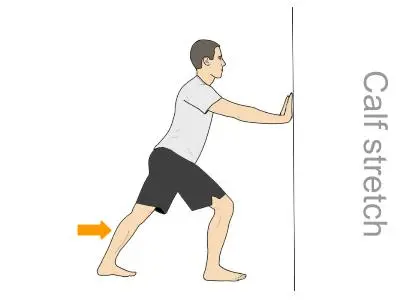
- Stretching the calves can help relieve stress and edema by loosening up the muscles around the ankle.
- While facing the wall, spread your palms shoulder-width apart against it.
- Take a step back with your injured leg and lock that knee. As far as it is comfortable for you, keep your heel on the ground.
- Bring your second leg forward while bending that knee. Keep the heel of your hurt foot near the ground. Your wounded leg’s back should feel somewhat stretched. Hold this for 20 seconds, then reset your body to neutral.
- Repeat with the second leg if you have tarsal tunnel syndrome in both of your feet. Three to five times per day, repeat this.
Posterior Tibialis Heel Lifts

- A crucial component of your tarsal tunnel is your posterior tibialis tendon. This tendon can be strengthened and stretched to help minimize any discomfort-causing swelling.
- Put your hands on the back or edge of a chair or counter as you stand in front of it in step 1. Leaning on the counter or a chair for support, slowly stand up on your toes. The “tip-toe” position should be maintained for five seconds.
- Release your support and gradually lower yourself back to the ground.
Balance Exercises for Sinus Tarsi Syndrome
Single-Leg Balance: Eyes Open

- Put your foot flat on the ground as you stand on one leg.
- Focus on a point in front of you to help with stability while holding your opposite leg out in front.
- Maintain for 60 seconds.
- Three to four times every day.
Single-Leg Balance: Eyes Closed
- Put your foot flat on the ground as you stand on one leg.
- Keep your eyes closed while keeping your opposing leg out in front.
- Maintain for 60 seconds.
- Three to four times every day.
Safety Considerations
Tarsal tunnel workouts should be performed slowly because tarsal tunnel syndrome is a result of an injury. Tarsal tunnel syndrome could become worse if you try to do too much, too soon, before your ankle has had a chance to heal.
No exercise should ever be painful. Any tarsal tunnel exercise should be stopped right away if you realize that it makes your ankle and foot feel worse. You should see a doctor if your tarsal tunnel syndrome worsens or persists.
FAQs
How long does sinus tarsi healing take?
When using conservative treatments, sinus tarsi syndrome recovery might frequently take several weeks. Individuals who have surgery often need to recover for several weeks. In some circumstances, it could take them up to 3 months to resume their athletic activity and 6–12 months to fully recuperate.
What kind of support is ideal for sinus tarsi?
Custom sinus tarsi orthotics and orthotic insoles are two conservative treatments for the syndrome.
What role does sinus tarsi have in clinical practice?
Sinus tarsi syndrome is a disorder that affects the ankle and foot and is brought on by subtalar joint instability. The most common complaints from athletes with this ailment are persistent anterolateral ankle pain and instability during functional tasks.
Proprioceptive training and balance.
alterations in activity.
exercising your muscles.
bracing, taping, or both.
suitable footwear.
What is the Tarsi syndrome’s course of treatment?
Treatment for sinus tarsi syndrome
Shoes that support flat feet can significantly alter your gait. Additionally, medial arch support orthotics for sinus tarsi syndrome can be beneficial. Some podiatrists may apply tape or braces. A specialized ankle brace may be very helpful for sinus tarsi syndrome.
Who provides care for sinus tarsal syndrome?
A foot and ankle orthopedic surgeon can determine the root of sinus tarsi syndrome and the most effective course of treatment before recommending surgery.
How can the sinus tarsi be strengthened?
Strengthening the posterior tibialis for sinus tarsi syndrome
Place the injured ankle on the opposing knee while seated.
Wrap a bandage around each foot.
The injured foot’s toes should be pointed, and they should be lifted against the band’s resistance.
To finish one repeat, slowly reposition yourself in the beginning position.
What percentage of tarsal tunnel surgeries succeed?
The success rates of surgeries range from 44% to 96%. During surgery, the flexor retinaculum is dissected from its proximal connection, which is located near the medial malleolus, down to the sustentaculum tali. There is a chance for ultrasound-guided tarsal tunnel release.