Vagus nerve stimulation
What is Vagus nerve stimulation?
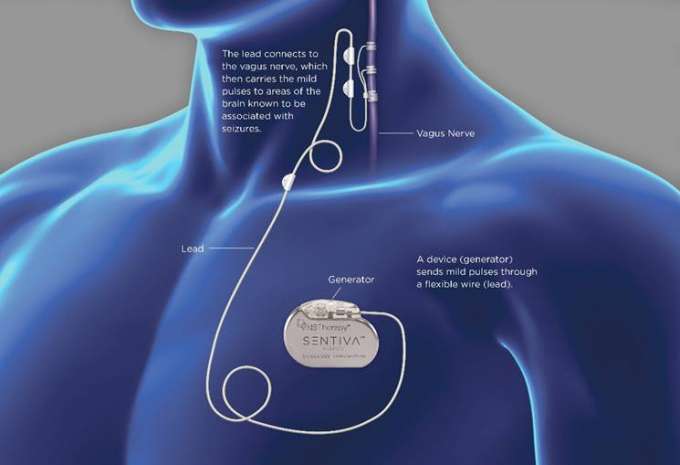
Vagus nerve stimulation (VNS) is a variety of neuromodulation, which is a treatment that varies the activity of nerves. Vagus nerve stimulation includes implanting a machine that transmits regular, mild pulses of electrical energy to your brainstem via the vagus nerve in your neck. After getting your brainstem, the electrical charge is discharged to various regions of your brain to alter the way brain cells work.
Vagus nerve stimulation functions such as a pacemaker for your heart. VNS is sometimes known as a pacemaker for the brain.
VNS is a treatment choice that you and your healthcare professional or doctor might believe after further traditional therapies haven’t been victorious. The benefit of VNS is restricted to a special group of people who have treatment-resistant epilepsy or treatment-resistant depression. More lately, VNS has been authorized as a rehabilitation aid for a choice of a person who’s had a stroke.
Anatomy and work of Vagus nerve
Your vagus nerve is one of 12 couples of cranial nerves that transmit electrical signals between your brain and various regions of your neck, head, and torso. They maintain many of your body’s functions.
Your vagus nerve is cranial nerve X (10) and is the most extended cranial nerve. You have one vagus nerve on per side of your body. Both begin at your brainstem and pass via your neck to your chest and abdomen.
Your vagus nerve is a portion of a circuit that connects your heart, neck, lungs, and abdomen to your brain.
What does the vagus nerve affect?
The vagus nerve has many various functions. The four key roles of the vagus nerve are:
Sensory: From the heart, throat, lungs, and abdomen.
Special sensory: Provides taste sensation after the tongue.
Motor Delivers motion functions for the muscles in the neck liable for swallowing and speech.
Parasympathetic: Liable for respiration, the digestive tract, respiration, and heart rate functioning.
Its roles can be broken down even distant into seven varieties. One of these is suspending the nervous system.
The nervous system can be separated into two regions: sympathetic and parasympathetic. The sympathetic side raises energy, alertness, heart rate, blood pressure, and breathing rate.
The parasympathetic side, which the vagus nerve is heavily included in, reduces blood pressure, alertness, and heart rate, and assists with relaxation, calmness, and digestion. As an outcome, the vagus nerve also assists with urination, defecation, and sexual arousal.
Other vagus nerve effects contain:
Communication between the brain and the gut: The vagus nerve provides data from the gut to the brain.
Relaxation with deep breathing: The vagus nerve conveys with the diaphragm. With deep breaths, a patient senses more relaxed.
Decreasing inflammation: The vagus nerve transmits an anti-inflammatory signal to further regions of the body.
Lowering the heart rate and blood pressure: If the vagus nerve is overactive, it can conduct to the heart be incapable to pump adequate blood near the body. In some circumstances, extreme vagus nerve activity can induce loss of consciousness and organ harm.
Fear management: The vagus nerve transmits data from the gut to the brain, which is connected to dealing with anxiety, stress, and fear hence the saying, gut feeling. These alerts assist a patient to recover from stressful and scary circumstances.
Indication of Vagus nerve stimulation
Approximately one-third of a patient with epilepsy don’t completely react to anti-seizure medications. Vagus nerve stimulation may be a possibility to decrease the frequency of seizures in a patient who hasn’t achieved control with drugs.
Vagus nerve stimulation may also be useful for a patient who hasn’t replied to intensive depression therapies, like antidepressant drugs, psychological counseling (psychotherapy), and electroconvulsive treatment (ECT).
The Food and Drug Administration (FDA) has agreed to vagus nerve stimulation for a patient who:
- Are 4 years aged and more senior
- Have focal (partial) epilepsy
- Have seizures that aren’t well-controlled with drugs
The FDA has also agreed on vagus nerve stimulation for the therapy of depression in grown-ups who:
Keep chronic, hard-to-treat depression (treatment-resistant depression)
Haven’t enhanced after attempting four or more drugs or electroconvulsive therapy (ECT), or both
Continue standard depression therapies along with vagus nerve stimulation
Further, investigators are examining vagus nerve stimulation as a potential therapy for a combination of diseases, involving rheumatoid arthritis, headaches, bipolar disorder, inflammatory bowel disease, obesity, and Alzheimer’s condition.
Contraindication of Vagus nerve stimulation
You may not be a prospect for vagus nerve stimulation if:
You’re pregnant.
Have breathing issues, involving sleep apnea, asthma, chronic obstructive pulmonary condition, or further lung conditions and diseases.
Have active peptic ulcer condition.
Have insulin-dependent diabetes mellitus.
Have only one vagus nerve.
Have dysautonomias, which include abnormal functioning of your autonomic nervous system.
Are accepting further states of brain stimulation.
Have heart arrhythmias or different heart abnormalities.
Have a record of schizoaffective disease, schizophrenia, delusional diseases, or rapid cycling bipolar disease.
Have prior surgery to your left neck including removing the region of your vagus nerve.
Risks
For most patients, vagus nerve stimulation is secure. But it does have some hazards, both from the surgery to implant the machine and from the brain stimulation.
Surgery risks
Surgical difficulties with planted vagus nerve stimulation are infrequent and are equal to the hazards of having further kinds of surgery. They contain:
- Pain where the cut (incision) is created to implant the machine
- Infection
- Problem in swallowing
- Vocal cord paralysis, which is generally temporary, but can be permanent
Side effects after surgery
Some of the side outcomes and health issues associated with implanted vagus nerve stimulation can contain:
- Voice changes
- Hoarseness
- Throat pain
- Cough
- Headaches
- Shortness of breath
- Problem in swallowing
- Tingling or prickling of the skin
- Insomnia
- Worsening of sleep apnea
For most patients, side outcomes are tolerable. They may decrease over time, but some side results may stay bothersome for as long as you use planted vagus nerve stimulation.
Modifying the electrical impulses can assist minimize these outcomes. If side outcomes are intolerable, the machine can be shut off temporarily or permanently.
How do you prepare for Vagus nerve stimulation?
It’s essential to carefully evaluate the pros and cons of planted vagus nerve stimulation before choosing to have the method. Make certain you know what all of your other therapy options are and that you and your doctor or physician both feel that planted vagus nerve stimulation is the best choice for you. Ask your doctor or physician just what you should hope during surgery and after the pulse generator is in position.
Food and medications
You may require to stop accepting specific drugs ahead of time, and your doctor or physician may ask you not to consume the night before the method.
What you can hope
Before the process
Before surgery, your doctor or physician will do a physical inspection. You may require blood examinations or further tests to make certain you don’t have any health problems that might be an issue. Your doctor or physician may have you begin bringing antibiotics before surgery to control infection.
During the procedure
Surgery to implant the vagus nerve stimulation machine can be done on an outpatient basis, though some surgeons suggest waiting overnight.
The surgery generally brings an hour to an hour and a half. You may stay awake but have drugs to numb the surgery location (local anesthesia), or you may be senseless during the surgery (general anesthesia).
The surgery itself doesn’t include your brain. Two incisions are made, one on your chest or in the armpit (axillary) area, and the further on the left side of the neck.
The pulse generator is planted in the upper left side of your chest. The machine is indicated to be a permanent implant, but it can be withdrawn if required.
The pulse generator is roughly the size of a stopwatch and operates on battery power. A lead wire is affixed to the pulse generator. The lead wire is shown beneath your skin from your chest up to your neck, where it’s connected to the left vagus nerve via the second incision.
After the procedure
The pulse generator is started during a visit to your doctor’s office a few weeks after surgery. Then it can be programmed to provide electrical stimulations to the vagus nerve at different frequencies, durations, and currents. Vagus nerve stimulation generally begins at a low level and is slowly risen, relying on your symptoms and side outcomes.
Stimulation is programmed to start on and off in precise cycles like 30 seconds on, and five minutes off. You may include some tingling feelings or little pain in your neck and temporary hoarseness when the nerve stimulation is on.
The simulator doesn’t see seizure activity or depression symptoms. When it’s turned on, the stimulator starts on and off at the intervals chosen by your doctor. You can utilize a hand-held magnet to start stimulation at a further time, for instance, if you feel an upcoming seizure.
The magnet can also be utilized to temporarily turn off the vagus nerve stimulation, which may be required when you do specific activities like public singing, speaking, or exercising, or when you’re consuming if you have swallowing issues.
You’ll require to visit your doctor or physician sometimes to make certain that the pulse generator is functioning perfectly and that it hasn’t shifted out of position. Inspect your doctor or physician before having any medical examinations, like magnetic resonance imaging (MRI), which might interrupt your machine.
Results of Vagus nerve stimulation
Planted vagus nerve stimulation isn’t a treatment for epilepsy. Most patients with epilepsy won’t prevent having seizures or bring epilepsy drugs altogether after the process. But numerous will have fewer seizures, up to 20 to 50 % fewer. Seizure intensity may decrease as nicely.
It can bring months or a year or longer of stimulation before you see any important decrease in seizures. Vagus nerve stimulation may also shorten the healing time after a seizure. A patient who’s had vagus nerve stimulation to manage epilepsy may also experience progress in mood and quality of life.
An analysis is still mixed on the uses of implanted vagus nerve stimulation for the therapy of depression. Some analyses indicate the uses of vagus nerve stimulation for depression accrue over time, and it may bring at slightly several months of therapy before you see any progress in your depression symptoms. Planted vagus nerve stimulation doesn’t function for everybody, and it isn’t intended to substitute traditional therapies.
Further, some health insurance deliverers may not pay for this method.
Analyses of planted vagus nerve stimulation as a therapy for diseases like Alzheimer’s condition, headaches, and rheumatoid arthritis have been too small to draw any definitive conclusions regarding how well it may perform for those issues. More study is required.
How it works?
VNS include a pulse generator inserted under a patient’s skin on their chest. The implantable machine, which is equal to a pacemaker, produces periodic electrical pulses to the brain through the vagus nerve. For instance, a machine may be programmed to produce for 30 seconds every 5 minutes.
It is likely to deliver further stimulation by putting the supplied magnet over the pulse generator.
Relaxation methods like yoga, breathing activities, and medication can control vagus nerve activity, improving its capability to ease anxiety and mood-related symptoms.
Routes to naturally stimulate the vagus nerve to contain:
- singing
- loudly gargling with water
- coughing
- om or mantra chanting
- meditating
- showering with cold water
- using ice water on the face
- deep breathing exercises
- laughing
What result can be expected with vagus nerve stimulation (VNS)?
In epilepsy
Vagus nerve stimulation doesn’t heal epilepsy. It likely won’t fully stop your seizures, either, and you’ll require to continue taking an anticonvulsant drug. The purpose of VNS is to decrease the length, number, and severity of your seizures.
A 454-person analysis indicated a 50% or greater decrease in seizures in 37% of persons at one year, 43% at two years, and 43% at three years.
In depression
Analysis stays unclear on how well VNS functions to manage depression. So, it’s generally not suggested until drugs, in combination with psychotherapy, have first been attempted.
The FDA established its acceptance of investigations including more than 200 patients with treatment-resistant depression. After one year, 20% to 30% of patients with depression noted marked progress. But other patients with depression didn’t enhance or their symptoms worsened.
In stroke rehabilitation
The FDA established its acceptance of the outcomes of a 108-person analysis. Persons, split into a 53-person analysis group and a 55-person control group, were invited to conduct 300 to 400 physical treatment activities for 90 minutes a day, three times a week for six weeks. The analysis group obtained VNS throughout the 90-minute sessions. Patients in the treatment group had a moderate limb mobility score growth of 5 points corresponding to a 2.4-point gain in the patient in the control group. Approximately 47% of those in the therapy group saw a 6 point or more progress in limb mobility score 90 days post-therapy corresponding with a 24% progress in a patient in the control group.
For all FDA-approved uses, it may bring one year or more extended to know if or how nicely VNS is performing for you.
FAQ
What naturally stimulates the vagus nerve?
The vagus nerve is attached to your vocal cords and the muscles behind your throat. Singing, chanting, humming, and gargling can trigger these muscles and facilitate your vagus nerve. And this has been displayed to raise heart-rate variability and vagal tone
How do you know if your vagus nerve is stimulated?
The vagus nerve stimulates specific muscles in the heart that allow slowing heart rate. When it overreacts, it can generate a sudden decrease in heart rate and blood pressure, resulting in fainting
How do you know if your vagus nerve is not working properly?
When the vagus nerve itself gets harmed, you’ll deal with some ache in your neck – but further strange symptoms will show themselves as well. You’ll see problems with your voice, issues with your throat, brain fog, a risen heart rate, too high or low blood pressure, and gut issues.
How can I reset my vagus nerve?
Some of the most famous ones feature easy hacks to tone or reset the vagus nerve, in which patient plunge their looks into ice water baths or lie on their backs with ice packs on their chests. There are even neck and ear massages, eye movements, and deep-breathing methods.
What organs are affected by the vagus nerve?
The most essential role of the vagus nerve is afferent, obtaining data of the inner organs, like the gut, heart, liver, and lungs to the brain. This recommends that the inner organs are the primary origins of sensory data in the brain.