VAGUS NERVE
INTRODUCTION
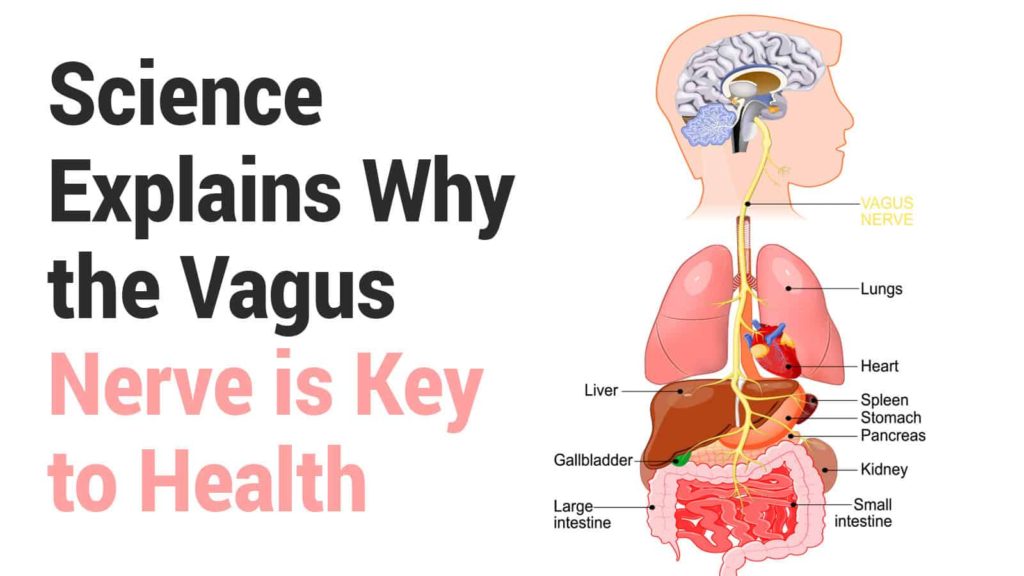
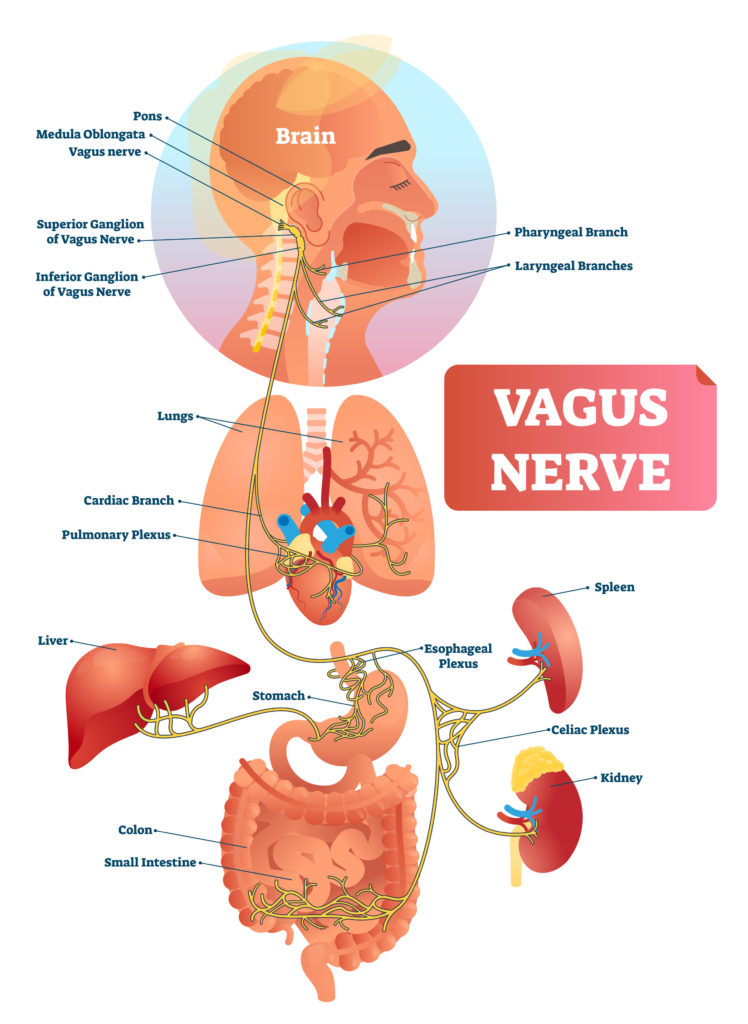
The vagus nerve is the longest and most complex of the 12 pairs of cranial nerves that emanate from the brain. It transmits information to or from the surface of the brain to tissues and organs elsewhere in the body.
The name “vagus” comes from the Latin term for “wandering.” This is because the vagus nerve wanders from the brain into organs in the neck, chest, and abdomen.
It is also known as the 10th cranial nerve or cranial nerve X.
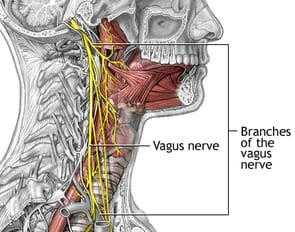
VAGUS NERVE ANATOMY
The vagus nerve has the longest course of all the cranial nerves, extending from the head to the abdomen. Its name is derived from the Latin ‘vagary’ – meaning wandering. It is sometimes referred to as the wandering nerve.
In the Head:
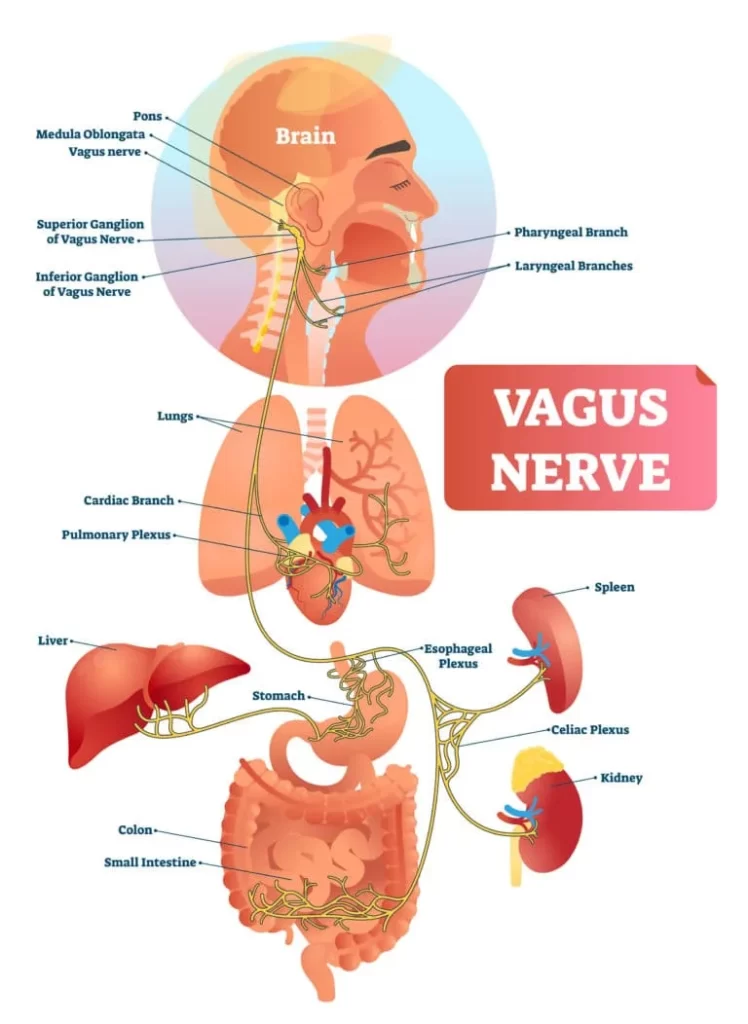
The vagus nerve originates from the medulla of the brainstem. It exits the cranium via the jugular foramen, with the glossopharyngeal and accessory nerves (CN IX and XI respectively).
Within the cranium, the auricular branch arises. This supplies sensation to the posterior part of the external auditory canal and external ear.
In the Neck :
In the neck, the vagus nerve passes into the carotid sheath, travelling inferiorly with the internal jugular vein and common carotid artery. At the base of the neck, the right and left nerves have differing pathways:
The right vagus nerve passes anterior to the subclavian artery and posterior to the sternoclavicular joint, entering the thorax.
The left vagus nerve passes inferiorly between the left common carotid and left subclavian arteries, posterior to the sternoclavicular joint, entering the thorax.
Several branches arise in the neck :
Pharyngeal branches: Provides motor innervation to the majority of the muscles of the pharynx and soft palate.
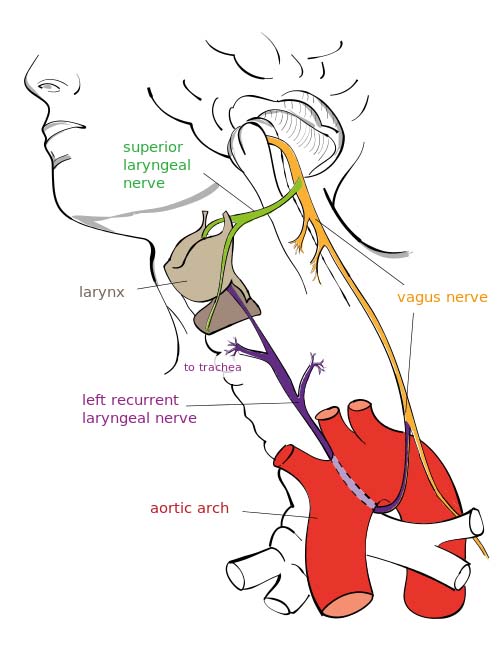
Superior laryngeal nerve: Splits into internal and external branches. The external laryngeal nerve innervates the cricothyroid muscle of the larynx.
The internal laryngeal provides sensory innervation to the laryngopharynx and superior part of the larynx.
Recurrent laryngeal nerve (right side only) : Hooks underneath the right subclavian artery, then ascends towards to the larynx.
It innervates the majority of the intrinsic muscles of the larynx.
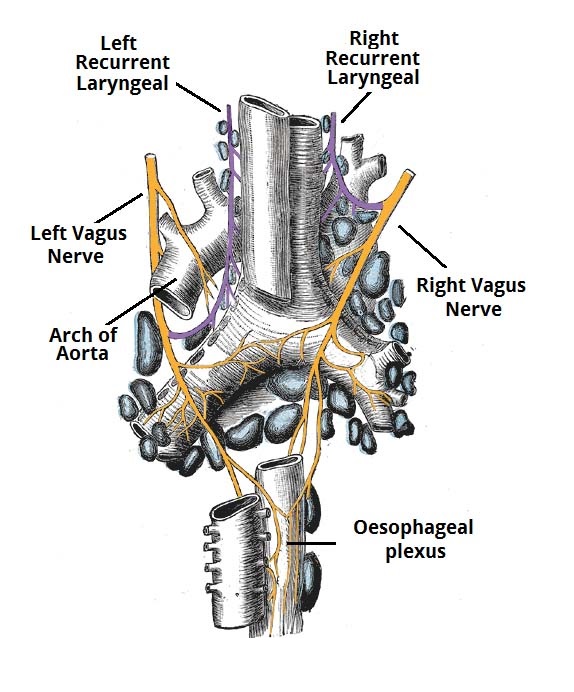
In the Thorax :
In the thorax, the right vagus nerve forms the posterior vagal trunk, and the left forms the anterior vagal trunk.
Branches from the vagal trunks contribute to the formation of the oesophageal plexus, which innervates the smooth muscle of the oesophagus.
Two other branches arise in the thorax :
Left recurrent laryngeal nerve: it hooks under the arch of the aorta, ascending to innervate the majority of the intrinsic muscles of the larynx.
Cardiac branches: these innervate regulate heart rate and provide visceral sensation to the organ.
The vagal trunks enter the abdomen via the oesophageal hiatus, an opening in the diaphragm.
In the Abdomen :
In the abdomen, the vagal trunks terminate by dividing into branches that supply the oesophagus, stomach and small and large bowel (up to the splenic flexure).
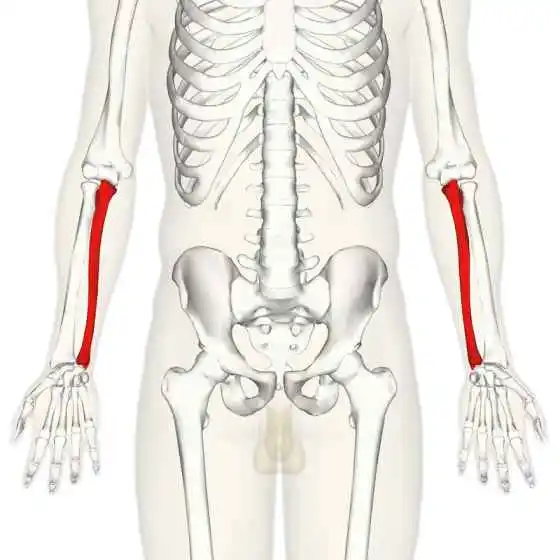
STRUCTURE OF VAGUS NERVE :
STRUCTURE OF VAGUS NERVE
- Upon leaving the medulla oblongata between the olive and the inferior cerebellar peduncle.
- The vagus nerve extends through the jugular foramen, then passes into the carotid sheath between the internal carotid artery and the internal jugular vein down to the neck, chest, and abdomen, where it contributes to the innervation of the viscera, reaching all the way to the colon.
- Besides giving some output to various organs, the vagus nerve comprises between 80% and 90% of afferent nerves mostly conveying sensory information about the state of the body’s organs to the central nervous system.
- The right and left vagus nerves descend from the cranial vault through the jugular foramina, penetrating the carotid sheath between the internal and external carotid arteries.
- Then passing posterolateral to the common carotid artery.
- The cell bodies of visceral afferent fibers of the vagus nerve are located bilaterally in the inferior ganglion of the vagus nerve (nodose ganglia).
- The right vagus nerve gives rise to the right recurrent laryngeal nerve, which hooks around the right subclavian artery and ascends into the neck between the trachea and esophagus.
- The right vagus then crosses anterior to the right subclavian artery, runs posterior to the superior vena cava, descends posterior to the right main bronchus, and contributes to cardiac, pulmonary, and esophageal plexuses.
- It forms the posterior vagal trunk at the lower part of the esophagus and enters the diaphragm through the esophageal hiatus.
- The left vagus nerve enters the thorax between left common carotid artery and left subclavian artery and descends on the aortic arch.
- It gives rise to the left recurrent laryngeal nerve, which hooks around the aortic arch to the left of the ligamentum arteriosum and ascends between the trachea and esophagus.
- The left vagus further gives off thoracic cardiac branches, breaks up into the pulmonary plexus, continues into the esophageal plexus, and enters the abdomen as the anterior vagal trunk in the esophageal hiatus of the diaphragm.
Branches :
- Pharyngeal nerve
- Superior laryngeal nerve
- Superior cervical cardiac branches of vagus nerve
- Inferior cervical cardiac branch
- Recurrent laryngeal nerve
- Thoracic cardiac branches
- Branches to the pulmonary plexus
- Branches to the esophageal plexus
- Anterior vagal trunk
- Posterior vagal trunk
- Hering-Breuer reflex in alveoli
The vagus runs parallel to the common carotid artery and internal jugular vein inside the carotid sheath.
Nuclei :
The vagus nerve includes axons which emerge from or converge onto four nuclei of the medulla :
The dorsal nucleus of vagus nerve : which sends parasympathetic output to the viscera, especially the intestines
The nucleus ambiguus : which gives rise to the branchial efferent motor fibers of the vagus nerve and preganglionic parasympathetic neurons that innervate the heart
The solitary nucleus : which receives afferent taste information and primary afferents from visceral organs
The spinal trigeminal nucleus : which receives information about deep/crude touch, pain, and temperature of the outer ear, the dura of the posterior cranial fossa and the mucosa of the larynx.
DEVELOPMENT OF VAGUS NERVE :
The motor division of the vagus nerve is derived from the basal plate of the embryonic medulla oblongata, while the sensory division originates from the cranial neural crest.
FUNCTIONS OF VAGUS NERVE :
Sensory Functions :
There are somatic and visceral components to the sensory function of the vagus nerve.
Somatic refers to sensation from the skin and muscles. This is provided by the auricular nerve, which innervates the skin of the posterior part of the external auditory canal and external ear.
Viscera sensation is that from the organs of the body. The vagus nerve innervates:
Laryngopharynx : via the internal laryngeal nerve
Superior aspect of larynx (above vocal folds) : via the internal laryngeal nerve.
Heart : via cardiac branches of the vagus nerve.
Gastro-intestinal tract (up to the splenic flexure) : via the terminal branches of the vagus nerve.
Special Sensory Functions :
- The vagus nerve has a minor role in taste sensation. It carries afferent fibres from the root of the tongue and epiglottis.
- (This is not to be confused with the special sensation of the glossopharyngeal nerve, which provides taste sensation for the posterior 1/3 of the tongue).
Motor Functions :
The vagus nerve innervates the majority of the muscles associated with the pharynx and larynx. These muscles are responsible for the initiation of swallowing and phonation.
Pharynx :
Most of the muscles of the pharynx are innervated by the pharyngeal branches of the vagus nerve:
- Superior, middle and inferior pharyngeal constrictor muscles
- Palatopharyngeus
- Salpingopharyngeus
- An additional muscle of the pharynx, the stylopharyngeus, is innervated by the glossopharyngeal nerve.
Larynx :
Innervation to the intrinsic muscles of the larynx is achieved via the recurrent laryngeal nerve and external branch of the superior laryngeal nerve.
Recurrent laryngeal nerve :
- Thyro-arytenoid
- Posterior crico-arytenoid
- Lateral crico-arytenoid
- Transverse and oblique arytenoids
- Vocalis
External laryngeal nerve:
- Cricothyroid
Other Muscles :
In addition to the pharynx and larynx, the vagus nerve also innervates the palatoglossus of the tongue, and the majority of the muscles of the soft palate.
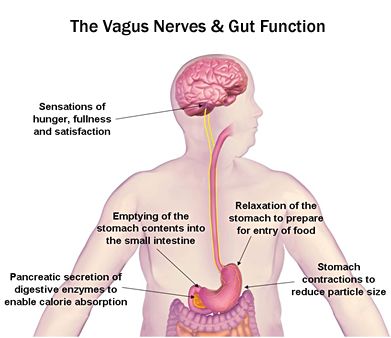
Parasympathetic Functions :
In the thorax and abdomen, the vagus nerve is the main parasympathetic outflow to the heart and gastro-intestinal organs.
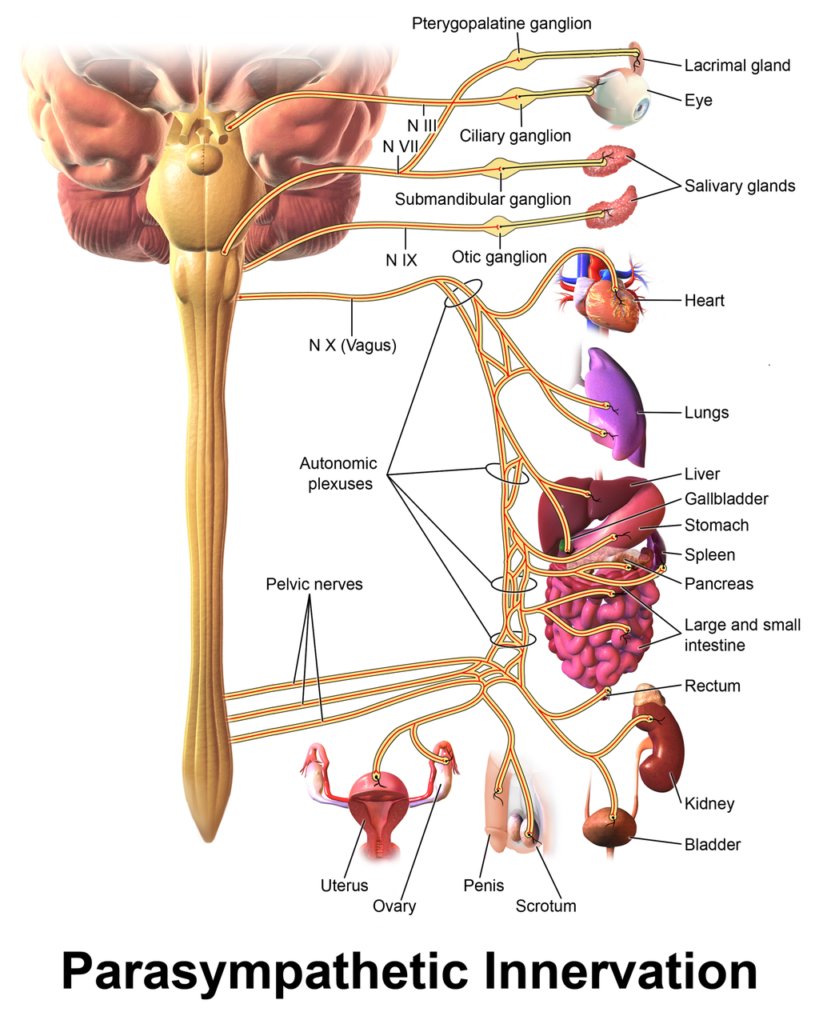
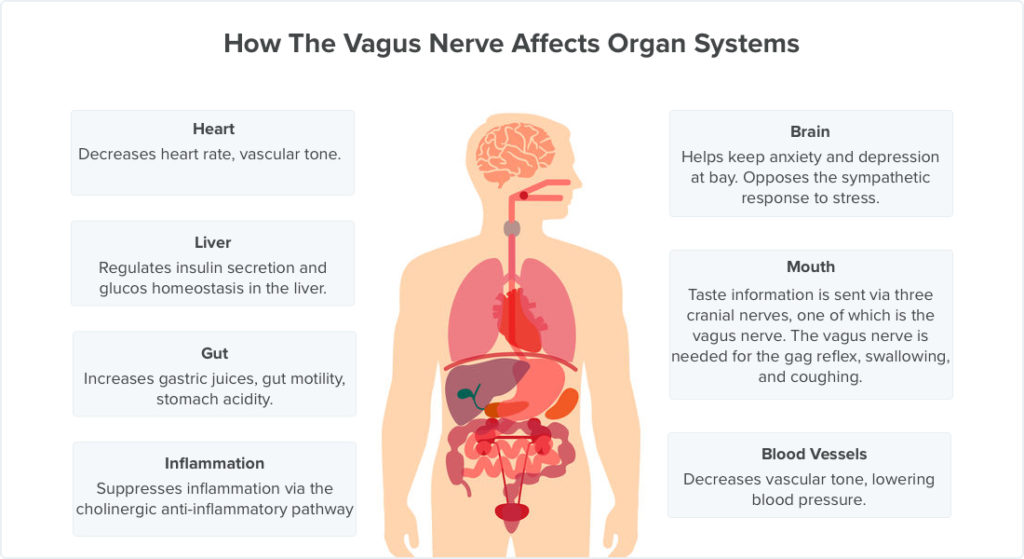
The Heart :
- Cardiac branches arise in the thorax, conveying parasympathetic innervation to the sino-atrial and atrio-ventricular nodes of the heart (For more heart anatomy, see here).
- These branches stimulate a reduction in the resting heart rate. They are constantly active, producing a rhythm of 60 – 80 beats per minute.
- If the vagus nerve was lesioned, the resting heart rate would be around 100 beats per minute.
Gastro-Intestinal System :
- The vagus nerve provides parasympathetic innervation to the majority of the abdominal organs.
- It sends branches to the oesophagus, stomach and most of the intestinal tract – up to the splenic flexure of the large colon.
- The function of the vagus nerve is to stimulate smooth muscle contraction and glandular secretions in these organs.
- For example, in the stomach, the vagus nerve increases the rate of gastric emptying, and stimulates acid production.
CLINICAL RELEVANCE
Disorders of the Vagus Nerve
Cardiovascular :
- Many pharmacological agents can be used to potentiate vagal tone in the heart therefore slowing the heart rate.
- Beta-blockers, muscarinic agonists, and cardiac glycosides such as Digoxin are just a few that can be used.
- Vasovagal syncope can ensue during a period of emotional stress for example causing a sudden drop in blood pressure and heart rate.
- Further to this, a carotid massage can compress the carotid sinus leading to the perception of high blood pressure.
- This will cause CN X to increase its firing leading to a decreased activity of the SA node and AV node.
- Overall a decreased rate and strength of contraction will ensue and the person may experience syncope.
- Many congenital heart defects such as a patent ductus arteriosus can irritate the left recurrent laryngeal nerve, leading to dysphonia (hoarse voice).
Gastro-Intestinal :
Lesions to the CN X are rare.
- A lesion to the pharyngeal branches can lead to dysphagia (difficulty swallowing) due to the involvement of the muscles of the pharynx.
- As CN X innervates the Palatopharyngeus and Salpingopharyngeus muscles a lesion here will cause the Palatoglossal arch to drop leading to Uvula deviation away from the affected side.
- The CN IX is sensory to the oropharynx and laryngopharynx with CN X being the motor efferents involved in the Gag reflex therefore a lesion in this area will cause a loss of the Gag reflex.
- Once upon a time a vagotomy could be done to reduce excess stomach acid production. However with advancements in pharmacological therapy this is no longer necessary.
Other clinical problems :
- As stated above a lesion to one of the RLN’s will cause dysphonia.
- A lesion to both RLN’s will cause aphonia (loss of voice) and a stridor (inspiratory wheeze).
- Paralysis of the RLN’s usually occur due to cancer of the larynx or thyroid gland or due to surgical complications.
Vagus nerve stimulation :
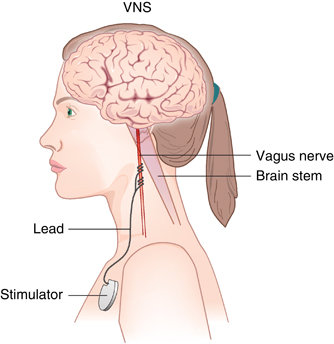
VAGUS NERVE STIMULATIONS
Vagus nerve stimulation (VNS) therapy using a neurostimulator implanted in the chest is a treatment used since 1997 to control seizures in epilepsy patients and has been approved for treating drug-resistant cases of clinical depression.
VNS may also be achieved by one of the vagal maneuvers:
- Holding the breath for 20–60 seconds, dipping the face in cold water, coughing, or tensing the stomach muscles as if to bear down to have a bowel movement.
- Patients with supraventricular tachycardia, atrial fibrillation, and other illnesses may be trained to perform vagal maneuvers (or find one or more on their own).
- Vagus nerve blocking (VBLOC) therapy is similar to VNS but used only during the day.
Vagotomy :
- Vagotomy (cutting of the vagus nerve) is a now-obsolete therapy that was performed for peptic ulcer disease.
- Vagotomy is currently being researched as a less invasive alternative weight-loss procedure to gastric bypass surgery.
- One serious side effect of vagotomy is a vitamin B12 deficiency, after about 10 years – which is similar to pernicious anemia.
- The vagus normally stimulates the stomach’s parietal cells to secrete acid and intrinsic factor.
- Intrinsic factor is needed to absorb vitamin B12 from food. The vagotomy reduces this secretion and ultimately leads to the deficiency.
- Which, if left untreated, causes nerve damage, tiredness, dementia, paranoia, and ultimately death.
- Researchers from Aarhus University and Aarhus University Hospital have demonstrated that vagotomy prevents (halves the risk of) the development of Parkinson’s disease.
- Parkinson’s disease begins in the gastrointestinal tract and spreads via the vagus nerve to the brain and dysregulated environmental stimuli.
- Such as that received by the vagus nerve from the gut, may have a negative effect on the dopamine reward system of the substantia nigra, thereby causing Parkinsons’ disease.
Chagas disease :
- The neuropathy in Chagas disease spreads in part via the major parasympathetic branches of the vagus nerve.
Sensory neuropathy :
- The hypersensitivity of vagal afferent nerves causes refractory or idiopathic cough.




8 Comments