Vitamin D
Introduction
Along with many other biological effects, vitamin D is a class of fat-soluble secosteroids that increases intestinal absorption of calcium, magnesium, and phosphate.
The two most significant substances in this category for humans are vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). The primary natural source of vitamin D is the production of cholecalciferol in the skin’s lower layers, which occurs as a result of a photochemical interaction with UVB light from UVB lamps or UVB radiation from the sun.
It is possible to consume ergocalciferol and cholecalciferol through supplements and food. Very few foods naturally contain large amounts of vitamin D, such as the meat of fatty fish.
Many breakfast cereals and plant-based milk alternatives, including cow’s milk, are fortified with vitamin D in the United States and other countries.
UV-exposed mushrooms provide beneficial quantities of vitamin D2. The dietary guidelines generally presume that an individual obtains their whole supply of vitamin D through oral means, as sun exposure varies throughout the population.
Given the risk of skin cancer, it is unclear how much sun exposure is safe. Skin production or dietary sources of vitamin D are not physiologically active. Two stages of protein enzyme hydroxylation—one in the liver and one in the kidneys—activate it.
Since most mammals can manufacture enough of it if they receive enough sunlight, vitamin D is not necessary and isn’t even considered a vitamin.
Rather, it can be viewed as a hormone since the active form, calcitriol, is produced when the vitamin D pro-hormone is activated. This form of calcitriol then acts on several nuclear receptors.
In the liver, ergocalciferol becomes 25-hydroxyergocalciferol while cholecalciferol becomes calcifediol (25-hydroxycholecalciferol). To assess a person’s vitamin D level, their serum is tested for these two vitamin D metabolites, often known as 25-hydroxyvitamin D or 25(OH)D.
The kidneys and certain immune system cells further hydroxylate calcifediol to produce calcitriol, or 1,25-dihydroxycholecalciferol, which is the physiologically active form of vitamin D.
As a hormone that circulates in the blood, calcitriol plays a vital function in controlling the amounts of calcium and phosphate in the body as well as encouraging the normal growth and remodeling of bone.
In addition, calcitriol affects immunological, neuromuscular, and cell proliferation in addition to reducing inflammation.
The metabolism and equilibrium of calcium are significantly influenced by vitamin D. It was discovered as a result of research into the food component that rickets patients (the juvenile form of osteomalacia) lacked.
Vitamin D supplements are administered for the treatment or prevention of rickets and osteomalacia. There is conflicting data about the additional health benefits of vitamin D supplementation in people with low vitamin D levels.
There is conflicting evidence about the impact of vitamin D supplementation on mortality; a meta-analysis revealed a marginal reduction in mortality among the elderly.
Aside from shielding high-risk individuals from rickets and osteomalacia, there may not be much of a benefit from vitamin D supplements for general or musculoskeletal health.
Types
There are several forms (vitamins) of vitamin D. The two major forms are vitamin D2 or ergocalciferol, and vitamin D3 or cholecalciferol. Without a subscript, vitamin D is referred to as calciferol and can be either D2 D3, or both.
In 1931, the chemical makeup of vitamin D2 was determined. 1935 saw the definition of vitamin D3’s chemical structure and the demonstration that 7-dehydrocholesterol was exposed to UV light to produce it.
Although a chemical nomenclature for vitamin D forms was suggested in 1981, other names are still often used.
Chemically speaking, the different forms of vitamin D are secosteroids, or steroids with a broken connection inside the steroid ring.
The side chain of vitamin D2, which has a methyl group on carbon 24 and a double bond between carbons 22 and 23, is where vitamin D2 and vitamin D3 differ structurally. Many synthetic analogs of vitamin D have been created.
Biology
The pharmacological effects of calcitriol, an active vitamin D metabolite, are mediated through binding to the vitamin D receptor (VDR), mostly found in target cell nuclei.
The VDR functions as a transcription factor that regulates the gene production of transport proteins (including TRPV6 and calbindin), which are involved in the absorption of calcium in the gut when calcitriol binds to it.
Vitamin D receptors (VDRs) are expressed by cells in the majority of organs, including the brain, heart, skin, gonads, prostate, and breast. They are members of the nuclear receptor superfamily of steroid/thyroid hormone receptors.
The maintenance of calcium and phosphorus levels in the blood (with the help of parathyroid hormone and calcitonin) and bone content is caused by VDR activation in the intestine, bone, kidney, and parathyroid gland cells.
Maintaining the calcium and phosphate levels necessary for bone formation, encouraging calcium absorption in the intestines, encouraging bone resorption by increasing the number of osteoclasts, and enabling proper parathyroid hormone function are some of the most significant functions of vitamin D in maintaining the skeletal calcium balance.
Because vitamin D insufficiency affects how the body processes minerals, it can lead to decreased bone mineral density and an increased risk of osteoporosis, diminished bone density, or bone fracture.
Because it is a strong stimulant of bone resorption, vitamin D plays a crucial function in bone remodeling as well. The VDR controls the division and multiplication of cells.
The immune system is impacted by vitamin D as well.
Activated T and B cells, monocytes, and other white blood cells express VDRs. In vitro, vitamin D influences the synthesis of glutathione, nitric oxide synthase, and neurotrophic factors via upregulating the expression of the tyrosine hydroxylase gene in adrenal medullary cells.
As we age, the expression of vitamin D receptors declines.
Deficiency
Vitamin D deficiency is defined as a blood 25(OH)D level below 12 ng/mL (30 nmol/liter) and vitamin D insufficiency as a blood 25(OH)D level of 12–20 ng/mL (30–50 nmol/liter) caused by an inadequate diet and insufficient sun exposure.
Worldwide, an estimated one billion adults—including those in wealthy Europe—are either deficient in or insufficient in vitamin D.
A rare disease in the developed world, severe vitamin D deficiency in children results in rickets, a softening and weakening of growing bones.
Across the world, vitamin D insufficiency is prevalent in older persons and children. Deficit causes poor bone mineralization and bone deterioration, which causes disorders that weaken the bones, such as adult osteomalacia and pediatric rickets.
A low level of 25-hydroxyvitamin D, or calcifediol, in the blood, can occur from sun avoidance.
The typical fraction of dietary calcium absorbed (between 60 and 80 percent) can be reduced to as little as 15 percent by having a vitamin D deficiency.
It has been demonstrated that persons with dark complexion who live in temperate areas have low vitamin D levels.
Melanin in the skin blocks the production of vitamin D, hence those with darker skin are less effective at producing vitamin D.
In the US, vitamin D deficiency is prevalent among African Americans and Hispanics, with wintertime vitamin D deficiency levels falling sharply.
Because melanin serves as the skin’s natural defense against sun exposure, this is caused by the skin’s melanin levels.
Bone health
A juvenile condition called rickets is marked by stunted growth and long, fragile, malformed bones that when a kid begins to walk, bend, and bow under their weight.
The usual onset period of rickets is between three and eighteen months.
Cases are still being documented in Western countries such as North America, and they are mainly observed in breastfed newborns and people with darker skin tones.
In the twenty-first century, low-income countries in Africa, Asia, or the Middle East are the main locations for this condition, which is characterized by bow legs and can be brought on by deficiencies in calcium, phosphorus, or vitamin D.
It is also more common in people who have genetic disorders like pseudo-vitamin-D-deficiency rickets.
A maternal vitamin D deficit can lead to both prenatal and postnatal bone quality degradation and overt bone disease.
In nations like Nigeria that receive a lot of sunlight throughout the year, nutritional rickets can develop even in the absence of a vitamin D deficit.
Even though osteomalacia and rickets are no longer common in the UK, outbreaks of the disease have occurred in some immigrant groups, affecting women who appeared to have had enough daylight outdoor exposure while dressed in Western clothes.
Rickets were not associated with darker skin or decreased sun exposure unless the diet diverged from a Western omnivore pattern that included large amounts of meat, fish, and eggs.
Avoiding animal products is one of the dietary risk factors for rickets.
Because breast milk is deficient in vitamin D and societal norms and environmental factors might hinder appropriate sun exposure, vitamin D insufficiency continues to be the primary cause of rickets in most countries’ newborn infant populations.
The occurrence of rickets in older toddlers and children in sunny countries like Bangladesh, South Africa, and Nigeria has been linked to low dietary calcium intakes, which are typical of cereal-based diets with restricted access to dairy products.
In the past, rickets were a serious public health issue in the United States. In the late 1920s, over two-thirds of 500 children in Denver had mild rickets.
A sharp drop in the frequency of rickets cases was correlated with a rise in the amount of animal protein in the American diet during the 20th century and greater use of milk supplemented with comparatively tiny amounts of vitamin D.
Notably, newborn vitamin supplements, vitamin D-fortified milk, and vitamin supplements have been instrumental in eliminating the bulk of ricket instances in infants with fat malabsorption problems in the United States and Canada.
Osteomalacia and Osteoporosis
Adults with osteomalacia are suffering from a vitamin D shortage. This condition is characterized by bone fragility, proximal muscle weakness, softening of the bones that causes the spine to bend, and an increased risk of fractures.
Osteomalacia raises the risk of bone fractures by decreasing calcium absorption and increasing calcium loss from bone. When 25-hydroxyvitamin D levels are less than roughly 10 ng/mL, osteomalacia is typically present.
There is no solid proof that persons with chronic pain have reduced vitamin D levels or that taking supplements reduces persistent nonspecific musculoskeletal pain, despite the theory that osteomalacia’s effects play a role in chronic musculoskeletal pain.
Osteoporosis, a disorder of decreased bone mineral density with elevated bone fragility and fracture risk, develops from osteomalacia.
Use of Supplements
Vitamin D supplementation is a dependable treatment or prevention strategy for rickets. However, it is unclear how vitamin D supplementation affects health that is not related to the skeleton.
Other than a possible drop in mortality in the elderly, a review found no effect of supplementation on the rates of non-skeletal disease.
Supplemental vitamin D does not change the course of myocardial infarction, stroke, cerebrovascular illness, cancer, osteoarthritis in the knee, or bone fractures.
According to a US Institute of Medicine (IOM) report, there was insufficient and inconsistent evidence linking the intake of calcium or vitamin D to outcomes related to cancer, cardiovascular disease and hypertension, diabetes, metabolic syndrome, falls and physical performance, immune functioning and autoimmune disorders, infections, neuropsychological functioning, and preeclampsia.
According to some academics, the IOM calculated the blood level of vitamin D linked to bone health incorrectly and issued recommendations that were overly specific.
The IOM panelists insist that the report is firmly grounded in the data and that they followed a “standard procedure for dietary recommendations”.
Mortality, All-Causes
Elderly people who take vitamin D3 supplements may have a lower chance of dying, yet this impact has not been shown to be strong enough or certain enough to warrant supplementation. Regarding the risk of death, other forms (calcitriol, alfacalcidol, and vitamin D2) do not seem to have any favorable effects.
Elevated blood levels seem to be linked to a decreased mortality risk; however, it remains uncertain if supplementation can produce this advantage.
Vitamin D deficiencies as well as excesses seem to be linked to aberrant functioning and early aging.
Serum calcifediol concentrations and all-cause mortality have a “U-shaped” relationship, whereby death is higher at high and low calcifediol levels than at moderate levels. Vitamin D-related harm level in the Black community compared to the White community.
Bone health
The widely held notion that vitamin D supplementation can help prevent osteoporosis is generally unsupported by solid data. Therefore, it is probably not necessary to use it generally to avoid this condition in people who do not have a vitamin D deficiency.
Taking vitamin D and calcium together may help avoid hip fractures in older adults with osteoporosis, but there is a tiny risk of stomach and renal issues as well.
According to a study, supplementing with 800 IU or more per day was “somewhat favorable in the prevention of hip fracture and non-vertebral fracture” in people over 65.
For those living on their own, the impact is negligible or nonexistent. Falls and reduced bone mineral density have been linked to low serum vitamin D levels. However, taking more vitamin D doesn’t seem to alter the danger.
Particularly in contact sports, athletes who are vitamin D deficient are more likely to suffer stress fractures and/or catastrophic breakage.
Athletes with inadequate (25(OH)D serum levels <30 ng/mL) or severely deficient (25(OH)D serum levels <25 ng/mL) levels benefit the most from supplementation.
Rising serum 25(OH)D concentrations are associated with incremental reductions in risk; these benefits plateau at 50 ng/mL, and levels above this do not yield any further benefits.
Limited evidence that vitamin D + calcium, but not alone, can promote healing in children with nutritional rickets has been reported in a 2020 Cochrane comprehensive review; however, the evidence was inconclusive for lowering fractures.
Since May 2016, the US Food and Drug Administration (FDA) has mandated that manufacturers list the amount of vitamin D as “nutrients of public health significance” on nutrition facts labels.
A suggested extension of the deadline gave some firms till July 1, 2021, to comply.
Cancer
Low vitamin D levels have been linked to an increased risk of developing a number of cancer forms.
Although the strength of the relationships was deemed modest, meta-analyses of observational studies have indicated a lower risk of cancer incidence associated with vitamin D intake and 25 (OH)D levels, specifically for colorectal cancer.
The relative risk of cancer mortality was found to be lower by up to 16% in multiple meta-analyses, despite the fact that randomized controlled studies have not demonstrated that vitamin D supplements lower the risk of cancer incidence.
Cardiovascular disease
There is no proof that taking vitamin D supplements lowers the risk of ischemic heart disease, stroke, myocardial infarction, or cerebrovascular illness.
In the general population, supplementation does not lower blood pressure.
Immune system
Infectious diseases
Generally speaking, vitamin D has antibacterial, antiviral, and anti-inflammatory properties that help to stimulate the innate immune system and suppress the adaptive immune system.
In the past, vitamin D was employed as a treatment for TB and appears to be a risk factor for the disease.
Low-dose vitamin D supplements (400–1000 IU/day) may marginally reduce the incidence of acute respiratory tract infections overall.
Higher doses (>1000 IU per day or more) could not confirm the benefits observed in young children and adolescents (ages 1 to 16).
For individuals with baseline 25(OH)D levels below 25 nmol/L, vitamin D treatment significantly lowers the likelihood of moderate or severe exacerbations of COPD; however, this effect is not observed in individuals with less severe insufficiency.
Asthma
Supplementing with vitamin D has little effect on preventing or treating asthma attacks.
Inflammatory Bowel Disease
Crohn’s disease and ulcerative colitis are the two main types of inflammatory bowel disease that affect people, and both are linked to low vitamin D levels.
The severity of inflammatory bowel illness has been associated with vitamin D insufficiency; however, it is unclear if vitamin D deficiency is the cause of inflammatory bowel disease or just one of its symptoms.
There is some evidence to suggest that vitamin D supplementation therapy may enhance biochemical markers and clinical inflammatory bowel disease activity ratings in patients with inflammatory bowel disease.
Treatment with vitamin D may be linked to a decrease in the symptoms of inflammatory bowel disease recurrence (relapse).
It’s unclear what the clinical response to vitamin D medication is or if this treatment enhances the patient’s quality of life.
Not enough research has been done to determine the best course of action and dosage for vitamin D therapy.
Other Conditions
Diabetes
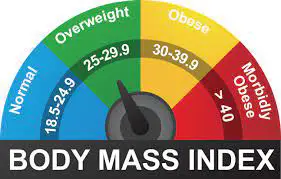
According to a meta-analysis, vitamin D treatment dramatically lowered the incidence of type 2 diabetes in non-obese individuals with prediabetes.
Vitamin D treatment was found to significantly enhance hemoglobin A1C (HbA1C), fasting blood glucose (FBG), and glycemic control [homeostatic model assessment-insulin resistance (HOMA-IR)] in people with type 2 diabetes, according to another meta-analysis.
According to prospective studies, there was a substantial reduction in the risk of type 2 diabetes, prediabetes, and combined type 2 diabetes and prediabetes, respectively, with high versus low levels of vitamin D.
One study, which was reviewed in a 2011 Cochrane systematic review, demonstrated that insulin and vitamin D combined maintained fasting C-peptide levels after a year more effectively than insulin alone.
However, it’s crucial to emphasize that the research that could be included in this analysis offered significance.
Attention Deficit Hyperactivity Disorder (ADHD)
Low vitamin D levels at birth were found to have a weak correlation with the development of ADHD later on, according to a meta-analysis of observational studies.
Children with ADHD also had lower vitamin D levels. Numerous small-scale, randomized controlled trials including vitamin treatment showed ameliorated symptoms of ADHD, including hyperactivity and impulsivity.
Depression
Although subgroup analysis revealed supplementation had a moderate effect for participants with clinically significant depressed symptoms or depressive disorder, clinical trials of vitamin D supplementation for depressive symptoms have largely been of low quality and show no overall effect.
Cognition and Dementia
A correlation between low vitamin D levels and cognitive impairment as well as an increased risk of Alzheimer’s disease was discovered through a comprehensive evaluation of clinical research.
Lower vitamin D levels, however, are also linked to inadequate diet and less time spent outside.
Consequently, a direct causal association between vitamin D levels and cognition could not be demonstrated because there are alternative explanations for the rise in cognitive impairment.
Schizophrenia
Studies have shown that persons with schizophrenia, especially those experiencing acute episodes, frequently have reduced vitamin D levels.
Pregnancy
Pre-eclampsia, low levels of vitamin D during pregnancy, and small-for-gestational-age babies are all linked to gestational diabetes.
It’s unknown how much vitamin D supplements can benefit a pregnant woman and her unborn child, even if they enhance the mother’s blood levels of the vitamin at term.
Taking enough vitamin D during pregnancy may have beneficial effects on the immune system and reduce the incidence of pre-eclampsia.
Supplementing with vitamin D is also likely to lower the risk of undersized newborns, poor growth rate, and gestational diabetes. Many often, pregnant women fail to take the necessary daily intake of vitamin D.
Weight Loss
Despite the theory that vitamin D supplementation, in addition to calorie restriction, may be an effective treatment for obesity, a systematic analysis failed to find any correlation between supplementation and fat mass or body weight.
Weight loss was found to increase circulating vitamin D status in a 2016 meta-analysis, suggesting that there may be an inverse relationship between blood levels of vitamin D and fat mass.
Allowable Health Claims
Governmental regulatory bodies specify which health claims are permissible to make on packaging for the food and dietary supplement businesses.
European Food Safety Authority
- immune system functioning normally
- typical inflammatory reaction
- typical muscular performance
- lower chance of falling in adults over 60
- FDA, the US Food and Drug Administration
- A well-balanced diet that includes adequate calcium and vitamin D, in addition to physical activity, may lower the risk of osteoporosis.
Health Canada
Children and adolescents who receive enough calcium and exercise may develop strong bones, and older adults may experience a lower risk of osteoporosis.
Additionally, a sufficient intake of vitamin D is required. Other potential resources for claim assistance include Australia-New Zealand and Japan FOSHU.
Dietary intake
Recommended levels
Different organizations have put forth differing suggestions regarding the daily allowance of vitamin D.
These differ depending on the exact definition, age, if a woman is pregnant or nursing, and how much skin production of vitamin D is assumed. Conversion: 40 IU (international unit) = 1 μg (microgram).
United Kingdom
In order to ensure adequate intake, the UK National Health Service (NHS) advises persons who are at risk of vitamin D insufficiency, infants who are breastfed, infants who are formula-fed and consuming less than 500 ml/day, and children between the ages of six months and four years old, to take daily vitamin D supplements.
This includes those who have low vitamin D synthesis in their skin, are seldom outside users, frail, housebound, residing in a care facility, or who typically wear clothing that covers up a large portion of their skin.
It also includes those with dark complexion, such as those of African, African-Caribbean, or South Asian descent. From April through September, others might be able to get enough vitamin D from sunshine exposure.
Public Health England and the NHS advise everyone, including expectant mothers that wintertime due to insufficient sunshine for the production of vitamin D
United States
The Institute of Medicine (IOM) (renamed the National Academy of Medicine in 2015) published dietary reference intakes for vitamin D in 2010 that superseded earlier recommendations that were stated in terms of appropriate consumption.
The guidelines were developed with the assumption that the person’s lack of skin synthesis of vitamin D is the result of insufficient sun exposure.
The reference intake for vitamin D is the total amount obtained from food, drink, and supplements, and it is based on the assumption that calcium needs are being satisfied.5.
The highest average daily intake of a nutrient that is likely to pose no risk of adverse health effects for nearly all persons in the general population” is the definition of the tolerated upper intake level (UL).
403 While ULs are thought to be safe, details on the long-term effects are not fully realized, and prolonged use of these dosage levels is not advised.
The amount in a serving is represented as a percentage of Daily Value (%DV) for food and dietary supplement labeling in the United States.
100% of the daily value for vitamin D was 400 IU (10 μg) for labeling purposes, but in May 2016, it was changed to 800 IU (20 μg) to align with the recommended dietary allowance (RDA).
Firms with annual food sales of at least US$10 million were required to comply with the new labeling laws by January 1, 2020, and firms with lower volume food sales had to comply by January 1, 2021.
Reference Daily Intake provides a table with the current and old adult daily values.
Canada
For vitamin D, Health Canada released tolerated upper intake levels (ULs) and recommended dietary intakes (DRIs) based on the jointly commissioned and financed Institute of Medicine 2010 report.
Australia and New Zealand
In 2006, Australia and New Zealand released dietary vitamin D consumption guidelines together with nutrient reference values.
The vitamin D insufficiency rate among Australians is about one-third.
European Union
After reviewing the available data in 2016, the European Food Safety Authority (EFSA) concluded that there is considerable variation in the connection between serum 25(OH)D concentration and outcomes related to musculoskeletal health.
They concluded that a serum 25(OH)D concentration of 50 nmol/L was an appropriate target value and that average needs and population reference intake values for vitamin D cannot be determined.
The recommended daily allowance for adults, including women who are pregnant or nursing, is 15 μg (600 IU).
In 2012, the EFSA conducted a study of acceptable consumption levels and came to the same result as the IOM: 100 μg/day (4000 IU) was the tolerated maximum limit for adults.
For children and people up to 75 years old, the Swedish National Food Agency suggests a daily dose of 10 μg (400 IU) of vitamin D3, and for individuals 75 years and above, 20 μg (800 IU).
European non-governmental organizations have put forward their own recommendations. 20 μg is advised by the German Society for Nutrition.
Postmenopausal women should take 15 μg (600 IU) until they are 70 years old, and then 20 μg (800 IU) starting at age 71, according to the European Menopause and Andropause Society.
If a patient has co-morbid problems or an extremely low vitamin D status, this dose should be increased to 100 μg (4,000 IU).
Sources
While very few foods naturally contain vitamin D, it is frequently added as a fortifier in processed meals. Some nations chemically fortify basic foods with vitamin D.
Natural Sources
Generally speaking, foods derived from animals—fish, meat, offal, eggs, and dairy—contain vitamin D3. Fungal ergosterol is exposed to ultraviolet light to create vitamin D2.
When exposed to UV light, mushrooms and the lichen Cladina arbuscula grow in vitamin D2. Industrial ultraviolet lamps are one way to encourage this process of fortification.
D2 and D3 content are reported by the US Department of Agriculture as a single number.
| Animal sources |
| sources | IU/g | Irregular |
| Cooked egg yolk | 0.7 | 44 IU for a 61g egg |
| Beef liver, cooked, braised | 0.5 | |
| Fish liver oils, such as cod liver oil | 100 | 450 IU per teaspoon (4.5 g) |
| Salmon, pink, cooked, dry heat | 5.2 | |
| Mackerel, Pacific, and jack, mixed species, cooked, dry heat | 4.6 | |
| Tuna, canned in oil | 2.7 | |
| Sardines, canned in oil, drained | 1.9 |
| sources | μg/g | IU/g |
| Cladonia arbuscula (lichen), thalli, dry vitamin D3 vitamin D2 | 0.67–2.04 0.22–0.55 | 27-82 8.8-22 |
| Portobello | Raw Exposed to ultraviolet light | 0.003 0.11 | 0.1 4.46 |
| Crimini | Raw Exposed to ultraviolet light | 0.001 0.32 | 0.03 12.8 |
Food Fortification
Certain fruit juices and fruit juice drinks, meal replacement energy bars, soy protein-based beverages, cheese and dairy products, flour products, baby formulas, a variety of breakfast cereals, and milk are examples of manufactured foods fortified with vitamin D.
The Food and Drug Administration (FDA) modified the rules governing food additives for milk fortification in the US in 2016.
The new regulations stipulated that the levels of vitamin D3 in dairy milk could not exceed 42 IU of vitamin D per 100 g (400 IU per US quart), 84 IU of vitamin D2 per 100 g (800 IU per quart) in plant milk, and 89 IU per 100 g (800 IU per quart) in plant-based yogurts or soy beverage products.
Drinks prepared from soy, almonds, rice, and other plant sources that are meant to replace dairy milk are known as plant milk.
While some research indicates that vitamin D3 increases blood levels of 25(OH)D more quickly and stays active in the body longer, other studies suggest that vitamin D2 sources are just as bioavailable and efficient as vitamin D3 at increasing and maintaining 25(OH)D.
Food Preparation
Cooking varies in how much vitamin D is removed from ordinary foods. Foods that were boiled, fried, or baked kept 69–89% of their original vitamin D content.
Recommended Serum Levels
Recommendations for serum levels of 25(OH)D differ throughout agencies and are contingent on various factors, including age. 25(OH)D values are typically reported in ng/mL by US labs. Other nations frequently utilize nmol/L. About 2.5 nmol/L is equivalent to one ng/mL.
According to a 2014 research, blood levels of 25(OH)D that seemed to be most beneficial for all outcomes seemed to be around 30 ng/mL (75 nmol/L).
Although the ideal ranges for vitamin D levels remain debatable, different research came to the conclusion that athletes should aim for levels between 30 and 40 ng/mL (75 and 100 nmol/L).
The fact that multiple studies have discovered variations in 25(OH)D blood levels throughout ethnic groups and have linked these variations to both hereditary and environmental factors contributes to part of the disagreement.
The usage of supplements to reach these recommended levels may result in detrimental vascular calcification.
Although the results of the studies that were analyzed were varied, a 2012 meta-analysis revealed that the risk of cardiovascular disorders increases when blood levels of vitamin D are lowest, within the range of 8 to 24 ng/mL (20 to 60 nmol/L).
An IOM committee determined in 2011 that for bone and general health, a serum 25(OH)D level of 20 ng/mL (50 nmol/L) is required.
The vitamin D dietary reference intakes are set with a margin of safety and intentionally “overshoot” the targeted serum value to guarantee that nearly all individuals meet the recommended intake levels and attain the required serum 25(OH)D levels.
The recommendations apply equally to those with dark skin or minimal sun exposure, and no contribution to serum 25(OH)D level is anticipated from sun exposure.
Serum 25(OH)D levels above 30 ng/mL (75 nmol/L), according to the Institute, are “not consistently associated with increased benefit”. Serum 25(OH)D concentrations of more than 50 ng/mL (125 nmol/L) can be reason for worry.
However, some individuals with serum 25(OH)D levels between 30 as well as 50 ng/mL (75 nmol/L- 125 nmol/L) will be insufficient in vitamin D.
Excess
Toxicology of vitamin D is rare. Taking large amounts of vitamin D supplements instead of getting enough sunshine is the cause. The level at which vitamin D becomes toxic is unknown; however, some studies suggest that the acceptable upper limit of intake (UL) for individuals aged 9 to 71 is 4,000 IU/day, or 100 μg/day. Meanwhile, other studies find that in healthy adults, a sustained intake of more than 50,000 IU/day (1250 μg) can result in overt toxicity after several months and raise serum 25-hydroxyvitamin D levels to 150 ng/mL and higher. Individuals suffering from specific medical diseases, such as primary hyperparathyroidism, are very susceptible to the effects of vitamin D and experience hypercalcemia when exposed to increased vitamin D intake. Additionally, maternal hypercalcemia during pregnancy may heighten the fetus’s susceptibility to the effects of vitamin D and result in a condition characterized by facial abnormalities and intellectual incapacity.
A mutation in the CYP24A1 gene results in a decrease in the breakdown of vitamin D, which is the cause of idiopathic infantile hypercalcemia. Such a mutation increases the sensitivity of infants to vitamin D and increases the risk of hypercalcemia if extra vitamin D is taken. The illness may persist throughout maturity.
According to a 2015 analysis, negative effects have only been documented at blood concentrations of 25(OH)D more than 200 nmol/L.
All documented instances of hypercalcemia-related toxicity where the 25-hydroxyvitamin D levels and vitamin D dosage are known involve daily intakes of at least 40,000 IU (1,000 μg) of vitamin D.
A doctor’s advice should be sought before taking a vitamin D supplement if you are pregnant or nursing. The FDA recommended that droppers included with liquid vitamin D supplements be appropriately and clearly labeled for 400 international units (1 IU is the biological equivalent of 25 ng of cholecalciferol/ergocalciferol).
Furthermore, the FDA advises that dropper hold values for products meant for newborns should not exceed 400 IU. The tolerable upper limit (the highest quantity that may be tolerated without harm) for newborns (birth to 12 months) is 25 μg/day (1,000 IU).
In newborns, a daily dosage of 1,000 micrograms has the potential to cause poisoning within a month.
As of November 30, 2010, following a commission from the governments of Canada and the United States, the Institute of Medicine (IOM)has raised the acceptable upper limit (UL) to 2,500 IU daily for children ages 1-3, 3,000 IU daily for children ages 4–8, and 4,000 IU daily for children ages 9–71+ (including women who are pregnant or nursing).
In addition to being influenced by parathyroid hormone, fibroblast growth factor 23, cytokines, calcium, and phosphate, calcitriol is auto-regulated in a negative feedback cycle.
Based on publicly accessible NHANES data from 1999 through 2014, a 2017 study evaluated the prevalence of high daily consumption levels of supplemental vitamin D among adults in the United States who are 20 years of age or older. Its information reveals the following
- 1 The NIH daily recommended amount (RDA) of 600–800 IU is exceeded by approximately 18% of the population by ingesting over 1000 IU, indicating purposeful supplement usage .
- 2 The daily tolerated upper intake level (UL) of 4000 IU set by the NIH is exceeded by over 3% of the population, above which there is an increased risk of hazardous consequences.
- 3 Trend analysis shows that since 1999, the proportion of the population consuming more than 1000 IU per day as well as the percentage taking more than 4000 IU per day have both increased.
Effect of Excess
Increased thirst and urination are signs of vitamin D poisoning, which is caused by hypercalcemia from a vitamin D excess. Untreated hypercalcemia causes excessive calcium deposits in soft tissues and organs, including the kidneys, liver, and heart, which can cause pain and damage to those organs.
The primary signs and symptoms of a vitamin D overdose are anorexia, nausea, and vomiting due to hypercalcemia. Polyuria, polydipsia, weakness, sleeplessness, anxiety, pruritus, and finally renal failure may ensue from these. In addition, there’s a chance of developing azotemia, proteinuria,
urinary casts, and metastatic calcification, particularly in the kidneys. Additional signs of vitamin D toxicity include weight loss, diarrhea, irritability, improper bone growth and formation, intellectual impairment in young children, and severe depression.
Reducing calcium intake and stopping vitamin D supplementation are the two main treatments for vitamin D toxicity. Damage to the kidneys may be irreparable.
Long-term exposure to sunshine typically does not result in vitamin D toxicity. Any additional vitamin D generated is broken down after the skin’s quantities of the precursors to vitamin D reach equilibrium.
Biosynthesis
In nature, the presence of UV light and the accompanying activation of the liver and kidneys are prerequisites for the synthesis of vitamin D.
Numerous fungi and animals both produce vitamin D2 from ergosterol and vitamin D3 from 7-dehydrocholesterol.
Interactive Pathway
To open, click the symbol in the bottom right corner.
To access the corresponding articles, click on the genes, proteins, and metabolites listed below.
Photochemistry
There are two phases involved in the conversion of 7-dehydrocholesterol to vitamin D3. Previtamin D3 is first produced when UV light photolyzes 7-dehydrocholesterol in a 6-electron conrotatory ring-opening electrocyclic process.
Second, in an antarafacial sigmatropic hydride shift, previtamin D3 isomerizes spontaneously to vitamin D3 (cholecalciferol). Previtamin D3 converts to vitamin D3 in an organic solvent over the course of roughly 12 days at room temperature.
In the skin, previtamin D3 is converted to vitamin D3 approximately ten times more quickly than it is in an organic solvent.
Similar steps are involved in the conversion of ergosterol to vitamin D2. Photolysis forms previtamin D2, which isomerizes to produce vitamin D2 (ergocalciferol).
Previtamin D2 is converted to vitamin D2 in methanol at a rate similar to previtamin D3. In case of white button mushrooms, the process is quicker.
Synthesis In The Skin
Most vertebrate animals, including humans, synthesize vitamin D3 photochemically from 7-dehydrocholesterol in their skin. Relatively substantial amounts of 7-dehydrocholesterol are generated, which is the precursor to vitamin D3. 7-UVB light with wavelengths between 290 and 315 nm reacts with 7-dehydrocholesterol.
Both sunlight and the light emitted by UV lamps in tanning beds contain these wavelengths. While UVA light makes up the majority of UV emissions, UVB light accounts for 4% to 10% of total UV emissions; certain tanning beds can only use UVB light bulbs specifically for the production of vitamin D.
Windows provide insufficient light exposure since UVB light is nearly entirely blocked by glass.
For people with the least amount of melanin, moderate sun exposure to the face, arms, and legs (averaging 5–30 minutes twice a week, or about 25% of the time for minimum sunburn) can create enough levels of vitamin D.
More minutes of exposure are required the darker the skin is on the Fitzpatrick scale and the weaker the sunshine.
The minimal erythema dose (MED) is influenced by three factors: the exposed body parts, exposure, and exposure. It is impossible to get too much vitamin D via UV exposure because the skin reaches a balance where the amount of vitamin D breaks down as quickly as it is made.
The dermis, or inner layer, and the epidermis, or outer, thinner layer, are the two main layers of skin. The keratinocytes of the stratum basale and stratum spinosum, the two innermost layers of the epidermis, are responsible for producing vitamin D. These same cells can also express the VDR and make calcitriol.
Evolution
The only method for synthesizing vitamin D is photochemical. Since it absorbs UVB rays, its sterol-based synthesis would have begun very early in the history of life, around the time of photosynthesis, potentially protecting DNA from harm and resulting in the inactive end product that is vitamin D.
Vertebrates are the only animals that have the well-known vitamin D endocrine machinery, which includes the vitamin D binding protein (DBP), the vitamin D receptor (VDR), and many CYP450 enzymes for activation and inactivation.
It is believed that early marine animals ingested vitamin D-rich plankton and absorbed calcium from the water into their skeletons, though it is unclear what role this played in species without calcified cartilage.
Oceanic phytoplankton, including Emiliania huxleyi and coccolithophore, have been photosynthesizing vitamin D for more than 500 million years.
For their calcified skeletons, land animals needed a source of vitamin D other than plants. To photosynthesize it in their skin, they needed to either consume it or be exposed to sunlight.
For over 350 million years, land vertebrates have been producing vitamin D through photosynthetic processes.
UV rays are blocked from reaching the skin of birds and other fur-bearing mammals by their fur or feathers. Rather, vitamin D is absorbed orally during grooming and is produced from oily skin secretions applied to the feathers or fur.
However, because serum 25-OH vitamin D levels are undetectable, some animals, like the naked mole-rat, are naturally low in cholecalciferol.
Due to the high activity of 7-dehydrocholesterol reductase, dogs and cats are essentially incapable of synthesizing vitamin D; instead, they obtain it from prey animals.
Industrial Synthesis
Industrial production of vitamin D3 (cholecalciferol) involves subjecting 7-dehydrocholesterol to UVB and UVC rays, then purifying the resultant material.
Fish organs, particularly the liver, sheep wool grease (lanolin), and some plants, such as lichen (Cladonia rangiferina), naturally contain 7- dehydrocholesterol. Similar steps are involved in the synthesis of vitamin D2 (ergocalciferol), which starts with ergosterol from yeast or mushrooms.
Mechanism of Action
Metabolic Activation
The prohormone calcifediol is created in the liver by use of the blood, which carries vitamin D. The kidneys may then transform circulating calcifediol into calcitriol, the physiologically active form of vitamin D.
Whether vitamin D is absorbed or generated through the skin, it is hydroxylated in the liver at position 25, which is the upper right corner of the molecule, to create 25-hydroxycholecalciferol, also known as calcifediol or 25(OH)D. The microsomal enzyme vitamin D 25-hydroxylase, which is produced by the human CYP2R1 gene and expressed by hepatocytes, catalyzes this process. After production, the product is released into plasma, where it binds to the vitamin D-binding protein, an α-globulin carrier protein.
Once in the kidney’s proximal tubules, calcifediol undergoes hydroxylation at the 1-α position, which is located on the lower right side of the molecule, resulting in the formation of calcitriol, also known as 1,25-dihydroxycholecalciferol, or 1,25(OH)2D.
The human CYP27B1 gene produces the enzyme 25-hydroxyvitamin D3 1-alpha-hydroxylase, which catalyzes the conversion of calcifediol to calcitriol.
Low calcium or phosphate as well as parathyroid hormone both increase CYP27B1 activity. Calcitriol is released into the bloodstream by the kidney after the last stage of conversion.
By securingCalcitriol is carried throughout the body, including the colon, kidneys, and bones, by a protein that binds vitamin D. The majority of the physiological effects of vitamin D are mediated by the most powerful natural ligand of the vitamin D receptor, calcitriol.
Apart from the kidneys, certain other cells such as immune system monocyte-macrophages also produce calcitriol.
Calcitriol is a local cytokine produced by monocyte- macrophages that stimulates the innate immune system to modulate the body’s defenses against microbial invaders.
Inactivation
Vitamin D3 24-hydroxylase has the ability to hydroxylate calcifediol and calcitriol at position 24, reducing their respective activities to secalciferol and calcitetrol.
Difference Between Substrates
As previously mentioned, the mechanisms of action of vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol) are comparable. To distinguish them from their D3-based counterparts, metabolites produced by vitamin D2 are termed with the prefix er- or ergo- (occasionally with a chole- prefix)
- 1 The vitamin D-binding protein tends to bind less strongly to metabolites derived from vitamin D2.
- 2 Sterol 27-hydroxylase (CYP27A1) has the ability to hydroxylate vitamin D3 to calcifediol, but not vitamin D2.
- 3 CYP27A1 has the ability to directly hydroxylate ergocalciferol at position 24. More inactivation results from this hydroxylation as well: after 24 hydroxylation, calcitriol’s activity drops to 60% of its initial level, whereas ercalcitriol’s activity drops by 10 times when it is converted to ercalcitetrol.
- Whether these variations result in a discernible decline in efficacy is up for debate (see § Food fortification).
Intracellular Mechanisms
Once within the target cell, calcitriol attaches itself to the cytoplasmic vitamin D receptor. When this active receptor connects to vitamin D response elements (VDRE), which are particular DNA sequences on genes, it reaches the nucleus.
The stimulation of transcription from these genes results in increased amounts of the proteins that mediate the actions of vitamin D.
The identification of numerous non-genomic functions of vitamin D can be attributed to some cell responses to calcitriol that seem to be too quick for the traditional VDRE transcription pathway.
In this route, the membrane-bound PDIA3 probably acts as a substitute receptor. There may still be use for the traditional VDR.
History
In 1922, vitamin D was found as a result of further research. In 1914, Elmer McCollum and Marguerite Davis, two American researchers, identified a compound in cod liver oil that was subsequently dubbed “vitamin A”.
British physician Edward Mellanby came to the conclusion that vitamin A, or a closely related substance, could prevent rickets after observing that dogs given cod liver oil did not get the condition.
Elmer McCollum studied modified cod liver oil in 1922 that had lost its vitamin A content. McCollum deduced that the element in cod liver oil that cured rickets was different from vitamin A since the altered oil healed the sick dogs.
Since he believed it to be the fourth vitamin to be named, he gave it the name vitamin D. At first, it was not understood that Since vitamin D may be produced by humans (in the skin) through exposure to UV radiation, it is more appropriately classified as a hormone than a vitamin.
It was discovered in 1925 that 7-dehydrocholesterol produces what is now known as D3, a sort of fat-soluble molecule, when it is exposed to light.
According to Alfred Fabian Hess, “Light equals vitamin D.” Adolf Windaus, a German scientist at the University of Göttingen, was awarded the 1928 Nobel Prize in Chemistry for his research on the makeup of sterols and how they relate to vitamins.
The structure of steroids and the as-yet- unknown vitamin D structure were being studied in 1929 by a team at NIMR in Hampstead, London.
A meeting took place with J.B.S. Haldane, J.D. Bernal, and Dorothy Crowfoot to discuss possible structures, which contributed to bringing a team together. X-ray crystallography showed the sterol molecules were flat, contrary to what was previously thought the Windaus-led German team.
Otto Rosenheim and Harold King presented a study in 1932 that proposed structures for bile acids and sterols, and it was quickly accepted.
Vitamin D was isolated and characterized as a result of the highly fruitful informal academic collaboration between Otto Rosenheim, Harold King, Kenneth Callow, and Robert Benedict Bourdillon.
The Medical Research Council at the time believed that everyone should have access to the findings of medical research, hence it had a policy of not patenting discoveries. Windaus provided additional clarification on the chemical makeup of vitamin D in the 1930s.
The University of Wisconsin’s Harry Steenbock, an American biochemist, proved in 1923 that exposing food and other organic materials to UV light might raise their vitamin D concentration.
Steenbock found that the rats had recovered from rickets after irradiating their diet. Steenbock paid US $300 out of his own funds to patent his creation. His method of irradiating food—most notably milk—was utilized.
By the time his patent expired in 1945, rickets had virtually disappeared in the United States.
The vitamin D receptor, a particular binding protein for vitamin D, was discovered in 1969. It was soon established that vitamin D is converted to calcifediol and subsequently to calcitriol, the form that is biologically active.
In 1980, a description of the photosynthesis of vitamin D3 in skin through previtamin D3 and its subsequent metabolism was published.
Research
The advantages of vitamin D therapies are the subject of conflicting studies. While 800–1,000 IU of supplements are safe, greater dosages that result in blood levels above 50 ng/mL (125 nmol/L) may have unfavorable effects.
Over the years, the US Office of Dietary Supplements launched the Vitamin D Initiative to keep tabs on the latest findings and enlighten consumers.
As of 2022, research on vitamin D’s potential benefits for treating and preventing diabetes, glucose intolerance, hypertension, multiple sclerosis, and other illnesses is still in its early stages.
Early research indicates a connection between low vitamin D levels and diseases in later life. An elderly person’s death rate has decreased, according to one meta-analysis.
Another meta-analysis with over 350,000 participants found that vitamin D supplementation does not, in unselected community-dwelling individuals, reduce non-skeletal outcomes (myocardial infarction, ischemic heart disease, stroke, cerebrovascular disease, cancer) or skeletal outcomes (total fracture) by more than 15%.
It is also unlikely that additional research trials with a similar design will alter these findings. As of 2022, there is not enough data to conclude that taking supplements of vitamin D lowers the risk of cancer.
A meta-analysis conducted in 2019 discovered a slight rise in stroke risk when calcium and vitamin D supplements were used concurrently.
COVID-19
The US National Institutes of Health declared in September 2022 that there wasn’t enough data to make a determination about whether vitamin D supplements should be used to treat or prevent COVID-19.
The UK’s National Institute for Health and Care Excellence (NICE) advises against giving vitamin D supplements to individuals purely for COVID-19 prevention or treatment.
For additional reasons, such as the health of the bones and muscles, both organizations included suggestions to stick with the previously set guidelines regarding vitamin D dosage.
Both groups stated that because of the pandemic’s reduced sun exposure, a greater number of people could need to take supplements.
The links between vitamin D insufficiency and unfavorable outcomes in COVID-19 have been reported in a number of systematic reviews and meta-analyses of numerous research.
Vitamin D deficiency or insufficiency significantly increased the susceptibility to contracting COVID-19 and having severe COVID-19, with odds ratios of 1.5 and 1.9, respectively, in the largest analysis, which included data from 76 observational studies involving nearly two million adults. However, these findings had a high risk of bias and heterogeneity.
Although a two-fold increase in mortality was discovered, the analysis lacked strength. These findings confirm smaller, earlier analyses, one of which, in reporting that people with COVID-19 tend to have lower 25(OH)D levels than healthy subjects, stated that the trend for associations with health outcomes was limited by the low quality of the research as well as by the potential for pathways of reverse causality.
Three studies on the effects of oral vitamin D or calcifediol supplementation were meta-analyzed, and the results showed no change in mortality but a lower rate of intensive care unit (ICU) admissions (odds ratio: 0.36) when compared to those who did not get the supplementation.
The data supporting the usefulness of vitamin D supplementation for the treatment of COVID-19 was found to be extremely ambiguous in a Cochrane review that included three additional studies.
They discovered that the three included trials had significant clinical and methodological variability, mostly due to variations in supplementing techniques, vitamin D formulations (one used calcifediol), pre-treatment status, and reported outcomes.
Another meta-analysis found that while calcifediol supplementation may have a benefit, the use of large dosages of vitamin D in individuals with COVID-19 is not supported by reliable data safeguarding impact on ICU admissions.
FAQ
Which food is rich in vitamin D?
The best food sources of vitamin D are oily fish, including salmon, mackerel, and sardines. Other sources include egg yolks, red meat, and liver. Vitamin D is added to some foods too, including breakfast cereals, plant milks and fat spreads.
How can I increase vitamin D in my body?
You can increase your vitamin D levels by getting sun exposure or eating foods rich in vitamin D, including fatty fish, egg yolks, and vitamin D-fortified milk and grains. In some cases of deficiency, a doctor may recommend vitamin D supplements.
Is 2 eggs a day enough vitamin D?
According to the USDA, one large egg contains around 11% of your daily value (DV). This means that if you like to scramble up two eggs for breakfast, that’s 22% of your vitamin D needs for the day from one meal.
Which fruit is good for vitamin D?
Oranges are one of the fruits rich in Vitamin D as its juice is fortified with calcium & vitamin D. This is one of the best sources of vitamin D for people who are lactose intolerant and cannot include milk & dairy products in their diet.
Which dry fruits are high in vitamin D?
You can boost Vitamin D content in your body by incorporating dry fruits such as almonds, raisins, prunes, and figs. Also meat, mushroom, and yogurt are also good sources of vitamin D.



7 Comments