Disuse Osteoporosis
What is a Disuse Osteoporosis?
Osteoporosis is a medical condition characterized by the gradual weakening of bones, leading to a decrease in bone density and an increased risk of fractures. Disuse osteoporosis specifically refers to bone loss that occurs as a result of reduced physical activity or immobilization.
When bones are not subjected to regular mechanical stress through weight-bearing activities, such as walking or resistance training, they may lose mineral density and structural integrity.
Your bones become silently weaker due to osteoporosis, which increases your risk of bone fractures. Exercise and certain treatments can help stop the loss of bone density. If you have a family history of osteoporosis or are elderly, ask your doctor about a bone density test. Osteoporosis is generally divided into two categories: primary and secondary.
Osteoporotic diseases that are not associated with other conditions are referred to as primary osteoporosis.
Secondary osteoporosis is the type of osteoporosis brought on by other medical conditions, but it is typically associated with aging and decreased genital function, such as a lower level of estrogen. Chronic illnesses are also contributing factors.
Introduction:
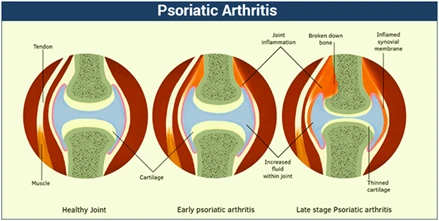
Disuse osteoporosis is a condition characterized by a reduction in mechanical stress on bones, leading to either localized or generalized bone loss. Reduced or absent mechanical stress on bones causes osteoblast-mediated bone formation to be inhibited and osteoclast-mediated bone resorption to accelerate, ultimately resulting in bone loss.
Neglect Osteoporosis can be brought on by extended voluntary bed rest, therapeutic bed rest, paraplegia or paraparesis from a spinal cord injury, hemiplegia or hemiparesis from a stroke, or localized immobilization from fracture treatments involving casts.
In general, your bones are strong and dense enough to support your weight and withstand most types of impacts. Your bones’ natural capacity to regenerate (remodel) themselves and lose some of their density as you age. Your bones are weaker and far more brittle than they should be if you have osteoporosis.
Disuse osteoporosis is marked by the morphological thinning of cortical bone at the diaphysis and a decrease in bone mineral density (BMD), which lowers bone strength and increases fracture risk. Despite aggressive and ongoing treatment with medication and rehabilitation, disuse osteoporosis is a long-term condition. Therefore, prophylactic osteoporosis management is the best treatment available.
Due to osteoporosis, bones become weak and brittle, easily breaking from simple stresses like bending over or coughing. The most common broken bones related to osteoporosis are the hip, wrist, or spine. Living tissue, such as bone, is continually being replaced and broken down. Osteoporosis develops when the body fails to produce new bone to replace lost bone.
Osteoporosis Pathogenesis
When we grow and become adults, our bones are constantly remodeling or being “modeling,” and this is due to the coordinated actions of two different types of cells known as osteoblasts and osteoclasts. While osteoclasts are in charge of bone resorption, osteoblasts create new bone. Both kinds of cells function because they are regulated by hormones.
Osteoporosis is a disorder that causes bone mass to decrease and fracture risk to increase when the loss of bone goes over bone formation. Osteoporosis is mostly caused by low the hormone estrogen, which increases bone turnover to the point where resorption outpaces formation.
Furthermore, corticosteroids may cause osteoporosis that primarily affects trabecular bone. The decrease in osteoblastic activity is the main reason for this. Compared to other chronic diseases, osteoporosis has a more complex pathogenesis. Its prevalence is correlated with other risk factors and genetics. An individual’s peak bone mass reaches its maximum value after necessary skeletal growth and bone mineral deposition.
The process slows down after adulthood. At that point, bone resorption begins to occur faster than bone formation. Cancellous bones become three times more osteoporotic during accelerated bone loss because of their higher metabolic activity than cortical bone. Important cancellous bones like vertebrae are good examples of this. The regulation of bone turnover is influenced by hormones, age, genetics, physical activity, and nutrition.
Symptoms of Disuse Osteoporosis
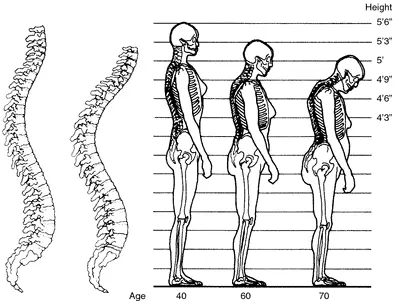
In the early stages of bone loss, symptoms are usually absent. Due to the absence of symptoms, osteoporosis is frequently referred to as the “silent” illness. Most often, a bone break usually after a small fall that would not typically result in a fracture tells a person they have the illness. Compression fractures of the spine are prevalent.
Even actions that appear normal, like bending or twisting to pick up a light object, might result in these. Either way, the vertebrae collapse down on themselves and the person loses height. The fractures can cause severe back discomfort, but they can also go undetected.
Osteoporosis’s effect on the vertebrae is the cause of the hunchback appearance that many old women have, sometimes referred to as “dowager’s” or “widow’s” hump.
Although there are no obvious symptoms associated with osteoporosis, you may observe certain changes in your body that may indicate your bones are weakening or losing density.
The following indications and symptoms could be present in you:
- Pain in the back that results from a fractured or dislocated vertebrae.
- Gradual decrease in height.
- A crouching position.
- An unexpectedly easily fractured bone.
Causes of Disuse Osteoporosis
While it is common for people to lose bone as they age, some people lose bone far more quickly than others. This may lead to osteoporosis and an increased risk of broken bones.
Like any other part of your body, your bones are made of living tissue. Though it may not seem like it, throughout your life, they are continually replacing their cells and tissue. Up until about age thirty, your body mostly replaces lost bone naturally. After the age of 35, your body can no longer replace the broken bone as quickly, causing you to gradually lose bone mass.
During the first few years following menopause, women also experience rapid bone loss. Women are more likely than men to have osteoporosis, particularly if they have had ovarian removal or if their menopause begins before the age of 45.
Children, men, and younger women are also at risk for osteoporosis. Numerous other factors can also contribute to the development of osteoporosis, including;
- Osteoporosis is more common in older adults and those who lose bone tissue more quickly.
- Additional medical conditions, such as those relating to inflammation, hormones, or malabsorption
- Osteoporosis in the family, especially if there is a parent’s hip fracture history
- Prolonged use of some medications, such as anti-estrogen tablets, which many women take after breast cancer, that can alter hormone levels or bone strength
- Developing or experiencing an eating disorder, such as anorexia or bulimia
- Possessing a low BMI (body mass index)
- Not engaging in regular exercise
- Excessive drinking and smoking
- Women are thinner than males and have less bone at birth. They also lose bone tissue more quickly as they age, with women often losing 30–50% of their total bone mass over their lifetimes, compared to men’s 20–33%.
Diagnosis
Conventional radiography and bone mineral density (BMD) measurements can be used to diagnose osteoporosis. Dual-energy X-ray absorptiometry is the most widely used technique to measure BMD.
Blood tests may be used to investigate potentially modifiable underlying causes in addition to detecting abnormal BMD, to diagnose osteoporosis. Depending on the likelihood of an underlying problem, tests for multiple myeloma, Cushing’s syndrome, cancer with bone metastases, and other conditions mentioned above might be performed.
Conventional radiography:
Conventional radiography is helpful in many clinical situations, such as soft tissue calcified tissue, secondary hyperparathyroidism, and cartilage loss in renal osteodystrophy. It can also be used in conjunction with CT or MRI to identify problems that arise from decreased bone mass, pre-osteoporosis, including fractures, and osteopenia follow-up exams. Conversely, radiography is relatively insensitive to early disease detection and requires a considerable amount of bone loss (approximately 30%) to be visible on X-ray images.
Increased radiolucency and cortical thinning are the two main radiographic characteristics of generalized osteoporosis. Vertebral fractures are common consequences of osteoporosis, and spinal radiography can be very helpful in the diagnosis and follow-up of these injuries. When examining vertical deformity in the T4-L4 region, for example, height loss combined with area reduction is a useful technique for objectively measuring vertebral height on plain-film X-rays. Another method is to calculate a spinal fracture index that accounts for the number of involved vertebrae.
Dual-energy X-ray:
The dual-energy X-ray (DEXA) scan is considered the gold standard for osteoporosis diagnosis. Osteoporosis is diagnosed when bone mineral density is less than or equal to 2.5 standard deviations below that of a young, healthy adult woman reference population, aged 30 to 40. T-scores are one way to express this. However, as people age, more people develop osteoporotic conditions because bone density declines with age.
Mostly because densitometers are still not widely available, doctors do not often recommend the test. It’s crucial for patients and doctors to talk about osteoporosis risk factors as well as when to get tested. A woman should have her bone density evaluated during menopause and then on a regular basis if her bone health permits. Males should get tested around age 65. For both men and women, a higher risk assessment might be necessary sooner, especially if they use certain drugs.
Complications
Bone fractures are the worst effects of osteoporosis, particularly when they happen in the hip or spine. Falls are often the cause of hip fractures, which can limit or even increase the risk of death in the year that follows the injury. It is possible to have broken vertebrae even in lack of a fall. The bones that make up your spine, known as vertebrae, can weaken and collapse, resulting in back pain, height loss, and a hunched-forward posture.
Treatment of Disuse Osteoporosis
The goals of osteoporosis treatment are to strengthen your bones with medication and treat and prevent broken bones. The likelihood that you will break a bone in the future will determine whether you require treatment. Your age, sex, and the findings of your bone density scan are just a few of the variables that will determine this.
A combination of treatments that slow down bone loss and strengthen your remaining bone tissue will be recommended by your physician. Preventing bone fractures is crucial when treating osteoporosis.
Osteoporosis treatment options could include;
- Modifying your way of life by altering your diet and exercise regimen
- Taking supplements of calcium and vitamin D
- Utilizing medications
To strengthen bones, medication can be used when;
Regardless of whether you have fractured or not, a bone density test has identified osteoporosis, and you have a high risk of doing so. A bone density test indicates that, despite not having osteoporosis, you have thin bones after suffering a bone fracture.
Supplements for vitamins and minerals:
- You might need to get your calcium and vitamin D from prescription or over-the-counter medications. Your healthcare provider will decide on the kind, strength, and quantity of the necessary medications for you.
Exercise:
- You can strengthen your bones and all the tissue that is attached to them, such as your muscles, tendons, and ligaments, by engaging in regular exercise. Weight-bearing exercises may be recommended by your healthcare provider to build muscle and improve your balance. Exercises that force your body to work against gravity, such as tai chi, yoga, Pilates, and walking, can help you become more balanced and strong without overstressing your bones. To discover the exercises and movements that are best for you, you might need to consult with a physical therapist.
Osteoporosis medications:
The most rough way to prevent further bone loss is to take prescription medication, such as the ones listed below.
Bisphosphonates:
The most widely used medications for treating osteoporosis are bisphosphonates. These are usually the first treatments suggested for postmenopausal women. Bisphosphonates include, for example;
- People who take alendronate (Fosamax) orally once a day or once a week
- Ibandronate, also known as Boniva, is administered intravenously four times a year or as a monthly tablet.
- As an oral tablet, Actonel comes in doses of one day, one week, or one month.
- One intravenous infusion of zoledronic acid is administered every one to two years.
Antibodies.
Antibody medications are available in two varieties.
Denosumab:
- Den is a medication that has been linked to a protein in your body that thins bone. It lessens the rate at which bones deteriorate. It also aids in keeping bone density intact. Every six months, you will receive an injection of a medication known as den.
Romosozumab:
Romosozumab (Evenity), a recently developed antibody, stimulates the formation of new bone. It received FDA approval in April 2019. The target audience consists of postmenopausal women who are at high risk of fracture. Among the women in this category are;
- Have fracture risk factors
- possess a fractured past
- Cannot take other osteoporosis medications or have not responded to them
Romosozumab is administered in two shots. For up to a year, you receive them once a month.
There are boxed warnings for Romosozumab, which are the FDA’s strongest cautions. It might make heart attacks, strokes, and cardiovascular disease more likely for you. If you had a heart attack or stroke within the last year, you should not take Romosozumab.
Surgery:
However, fractures resulting from advanced stages of osteoporosis require a significant amount of treatment. Hospitalization and surgery are necessary for serious fractures, such as shattered hips. A new hip composed of plastic or a combination of metal and plastic replaces the fractured hip following hip replacement surgery. Even though the procedure is mostly effective, hip fracture consequences can be quite dangerous.
These people are more likely than others in their age group to pass away in the first year after the accident, with a risk increase of 5 to 20%. Many of the survivors are unable to resume their prior level of activity, and many decide to relocate their self-care to a nursing home or assisted living arrangement. This is why it’s so important to start therapy as soon as possible and take action to stop bone loss.
Living with osteoporosis:
If you have osteoporosis, you can take precautions to lessen your risk of falling, like clearing out potential hazards from your home and scheduling routine vision and hearing tests.
Some possible treatments for a fracture would be to use:
- pain relievers
- Warm baths and cold packs are examples of hot and cold therapy.
- Methods of relaxation along with other pain management
If living with a long-term condition worries you, talk to a physician. They may be able to answer any questions you may have.
Speaking with other individuals who have the same condition as you or with a qualified counselor or psychologist may also be beneficial.
Risk factors:
The risk of developing osteoporosis can be increased by a variety of factors, such as age, race, lifestyle choices, and medical conditions and treatments.
Unchangeable dangers:
Some of the risk factors for osteoporosis are beyond your control, including:
- Your sex. Compared to men, women are far more likely to develop osteoporosis.
- years old. As you age, your likelihood of developing osteoporosis increases.
- Background. The two populations most at risk for osteoporosis are Asian and White.
- Ancestry. You run a higher risk if you have a parent or sibling who has osteoporosis, particularly if your parent broke a hip.
- Dimensions of the body frame. Smaller-statured men and women are generally more at risk because they may have less bone mass available to them as they get older.
Levels of hormones:
People with excess or insufficient levels of specific hormones in their bodies are more likely to develop osteoporosis.
As an example, consider;
- Sexual hormones. Bone is typically weakened by reduced sex hormone levels. One of the biggest risk factors for osteoporosis in women is the decline in estrogen levels that occurs during menopause. Bone loss is likely to be accelerated by treatments for breast cancer that lower estrogen levels in women and prostate cancer that lower testosterone levels in men.
- Thyroid issues. Elevated levels of thyroid hormone can cause bone loss. This can happen if you take too much medication to treat an underactive thyroid or if your thyroid is overactive.
- Other glands. Additionally linked to osteoporosis are hyperactive parathyroid and adrenal glands.
Dietary components:
An increased risk of developing osteoporosis is seen in those with:
- low consumption of calcium. The cause of osteoporosis is a chronic calcium deficit. Reduced calcium intake raises the risk of fractures, early bone loss, and decreased bone density.
- Eating issues. Being underweight and drastically reducing food intake affects bone in both men and women.
- Surgery related to the gastrointestinal. The amount of surface area available to absorb nutrients, including calcium, is limited by surgery to reduce the size of your stomach or remove a portion of your intestine. These surgical procedures cover weight loss as well as other gastrointestinal issues.
Steroids as well as other drugs:
Prednisone and cortisone are two examples of oral or injectable corticosteroid medications that can interfere with the process of rebuilding bone over time. Additionally linked to osteoporosis are drugs used to treat or eliminate;
- Seizures.
- Reflux of the stomach.
- Cancer.
- Rejection of a transplant.
Medical issues:
Osteoporosis is more common in those with specific medical conditions, such as;
- Gluten intolerance.
- Intestinal inflammation.
- Liver or kidney disease.
- Cancer.
- Multiple myelomas.
- Inflammatory arthritis
Preventive measures:
Osteoporosis can be managed, but there is no known cure. Once treated, osteoporosis patients typically have good results. The medications on the market now prevent bone loss, promote bone growth, and slow the disease’s progression.
Your lifetime bone health depends on eating a balanced diet and getting regular exercise. The best ways to prevent osteoporosis are usually to exercise and ensure that your diet contains adequate amounts of calcium and vitamin D. The best course of action for you and your bone health will be determined in collaboration with your physician.
Calcium:
- Between the ages of 18 and 50, both men and women require 1,000 mg of calcium daily. When women turn fifty and men turn seventy, this daily dosage rises to one thousand milligrams.
Among the best places to get calcium are:
- Dairy products with less fat.
- Green vegetables with a dark green color.
- Salmon or sardines with bones from containers.
- Foods such as cereal and orange juice with added calcium.
Many people may require calcium supplements because they do not consume enough calcium in their diets, particularly those who dislike or are unable to consume dairy products. There is variation in the calcium content of supplements. Those with calcium carbonate have the highest amount of useful calcium. It is advised to consume six to eight glasses of water daily along with supplements when eating.
Taking D-vitamin:
The body uses vitamin D to help soak up calcium. People can obtain vitamin D from foods like liver, fish oil, and milk fortified with vitamin D, or they can get it from sunshine and short walks (15–20 minutes each day). It might be necessary to take supplements during the winter. Usually, 400 mg per day is the recommended amount.
Follow these general safety tips to reduce your risk of injury:
- When taking part in any sport or activity, get the proper protective gear.
- Make sure nothing in your house or place where you work could trip you or anyone else.
- At home, always use the proper tools or equipment when reaching for objects. Never stand on countertops, tables, or chairs.
- Stick to a healthy exercise and nutrition regimen.
- Use a walker or cane if you have difficulty walking or are at risk of falls.
Staying away from alcohol and smoking:
Both smoking and binge drinking lower bone mass. Risks can be decreased by abstaining from smoking and consuming no more than two alcoholic beverages per day. One and a half ounces of hard liquor, twelve ounces of beer, or five ounces of wine make up an alcoholic drink.
Prognosis
Although osteoporosis is incurable, it can be controlled. Following treatment, the majority of osteoporosis patients get good outcomes. The current generation of medications prevents bone loss, promotes bone growth, and slows the disease’s progression.
Summary
Reduced pressure on the bone causes is known as disuse osteoporosis by speeding up osteoclast-mediated bone resorption and inhibiting osteoblast-mediated bone formation. Long-term therapeutic bed rest, immobilization resulting from peripheral nerve or central nervous system injury-related motor paralysis, and the use of casts to treat fractures are common causes of osteoporosis disuse. Rough trabecular pattern and cortical bone thinning are visible in the imaging diagnosis. Bone metabolism has been evaluated using signs of bone metabolism.
Antiresorptive drugs should be used to prevent bone resorption from the perspective of bone metabolism. To provide the weakened bone with the proper amount of mechanical stress, rehabilitation such as electrical stimulation, therapeutic exercise, and bed positioning should be recommended.
Even with these vigorous and ongoing treatments, bone takes a while to regain its strength and mineral density in the majority of cases of disuse osteoporosis. Whether disuse bone loss occurs in the sublesional territory of paralyzed patients or in the weight-bearing bones of immobilized individuals, it is still worthwhile discovering more about the various factors that contribute to this condition.
Many people worldwide suffer from osteoporosis, and while there isn’t a cure at this time, there are treatments that can help. Medication, medication for hormones, and exercise can all help to slow the loss of bone mass and strengthen existing bones. See your doctor if you think you may have osteoporosis. Talk about every potential course of action and lifestyle modification. You can choose the best course of treatment for yourself together.
FAQ:
It is likely that osteoporosis will require long-term management typically for the remainder of your life. Testing for bone density and routine visits with a physician are required. To modify your treatments as necessary, your provider will keep an eye on any changes in your bone density.
If you observe any physical changes that could be indicators of osteoporosis, get in touch with a healthcare professional. Any other symptoms you’re having should be mentioned to your doctor, particularly if you have bone pain or difficulty moving.
When there is insufficient force or strain on the bones, either locally or overall, the condition known as “disuse osteoporosis” occurs, leading to bone loss. Bones break easily as a result of becoming weak and brittle.
Although there is no cure for osteoporosis, its symptoms can be managed with medication and a change in lifestyle. Your doctor will suggest various treatments to help you based on your age, sex, and medical history. Strengthening your bones to make them less prone to breaking is the goal of treatment.
Osteoporosis is a disease that causes thinning, feeble bones. This raises the possibility of the bones shattering. The most commonly affected bones are the wrists, hips, and spine. Because of the decline in estrogen after menopause, men are four times less likely than women to develop osteoporosis.
Osteoporosis by itself is not harmful, and it does not affect life expectancy. On the other hand, it may raise your chance of getting a bone fracture (as well as a more serious break or post-fracture complications).
Numerous exercises can help to slow down the bone density loss that is associated with osteoporosis, even though there is nothing that can be done to reverse the condition. Individuals can increase their strength and lower their chance of fractures and falls by regularly walking with weights.
Generally speaking, things need to continue as usual possibly with a few minor modifications. Not every osteoporosis patient will experience a bone break. Rest assured that there won’t be any pain or other long-term issues if you don’t break a bone. It’s not inevitable to experience pain and other long-term issues even if you do break a bone.
Avoid exercises like sit-ups and touching your toes. Golf, tennis, bowling, and certain yoga poses are among the other sports that might need you to make a strong bend or twist at the waist.
People with osteoporosis are advised to sleep on their sides with a pillow between their knees to help realign their spines. To ease the strain on your lower back, you can also try sleeping on your back with a pillow between your knees.
The brief reply is that there are several lifestyle and health changes you can make to slow down bone loss, but osteoporosis cannot be fully cured. Additionally, your doctor might recommend drugs to you to promote bone growth and slow down bone loss.
Based on factors influencing bone metabolism, primary and secondary osteoporosis are the two types of osteoporosis. Age and menopause-related bone demineralization can lead to the development of primary osteoporosis.
A condition known as osteoporosis causes fragile bones with heightened susceptibility. Osteoporosis can have a variety of causes, but insufficient calcium in the bones is the main one. Low calcium causes a decrease in bone density. Because of this, bones become weaker and are more prone to breaking.
Bone density tends to remain constant between the ages of 25 and 50, with equal amounts of bone formation and bone breakdown. Bone loss frequently quickens after the age of 50 as bone resorption (breakdown) surpasses bone formation, especially during menopause.
Osteoporosis is not painful in and of itself. However, if the illness worsens, it may result in fractures and other uncomfortable issues. A long-term treatment plan is essential. Usually, the pain is worse than the aches that many people experience as they age.
For all women 65 years of age and above, as well as for younger women who are at a higher risk of fracture than average, bone density tests are advised. If a man is over 70 or has a high risk of developing thinning bones, then should talk with their doctor about getting tested for osteoporosis.
Family history: It is likely that there are inherited factors affecting bone development, as osteoporosis does run in families. You run a higher risk of fracture than usual if a close relative has experienced a fracture related to osteoporosis.
The most prevalent bone disease in humans, osteoporosis is a serious public health issue. It is more prevalent in older adults, women, and Caucasians. Just as hypertension increases the risk of stroke, osteoporosis does the same for fractures.
References:
- Utilize osteoporosis. August 1, 2001. PubMed. 116949544/pubmed.ncbi.nlm.nih.gov Reference inside text: Disuse Osteoporosis (2001)
- “Symptoms and Causes of Osteoporosis,” Mayo Clinic, September 7, 2023 Osteoporosis symptoms, causes, and Mayo Clinic website. Accessed April 20, 2035. In-text Citation: (Mayo Clinic, 2023) Osteoporosis: Symptoms and Causes
- Osteoporosis. January 18, 2024. Wikipedia. Osteoporosis. https://en.wikipedia.org/wiki/ Reference within the text: (Osteoporosis, 2024)
- Website, N. (October 14, 2022). NHS.uk/Osteoporosis. Osteoporosis: https://www.nhs.uk/conditions/ Citation inside the text: (Website, 2022)
- C. C. M., Professional (n.d.). https://my.clevelandclinic.org/health/diseases/4443-osteoporosis Cleveland Clinic. Osteoporosis Reference within the text: (Professional, n.d.)
- Treatments for Osteoporosis. (2019, November 6). Healthline. Available at https://www.healthline.com/health/treatments-for-osteoporosis#outlook Reference within the text: Osteoporosis Treatments, 2019
- Osteoporosis misuse. (n.d.). TheFreeDictionary.net. Osteoporosis is defined at https://medical-dictionary.thefreedictionary.com/disuse. Reference inside text: (Disuse Osteoporosis, n.d.)