Paraplegia: Rehabilitation & Physiotherapy Management
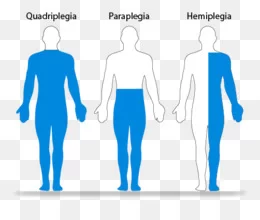
What is a Paraplegia?
- Paraplegia is paralysis or weakness (paraparesis) of both lower limbs.
- It may be due to:
- Pyramidal (U.M.N.) lesion resulting in spastic paraplegia.
- Lower motor neuron (L.M.N.) lesion resulting in flaccid paraplegia.
Definition of Paraplegia:
- It is paralysis or weakness of both lower limbs due to bilateral pyramidal tract lesion, most commonly in the spinal cord (spinal paraplegia), and less commonly in the brain stem or the cerebral parasagittal region (cerebral paraplegia).
Spinal paraplegia may be:
- Focal: paraplegia with sensory level.
- Systemic.
- Disseminated.
Causes of Spinal Paraplegia:
I- Focal causes:
- A. Compression:
- 1. Vertebral:
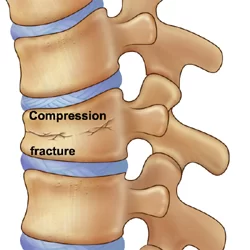
- Fracture or fracture-dislocation of the vertebra, Disc prolapse and spondylosis, Pott’s disease, Neoplastic diseases: Primary or metastatic and Deformity of the vertebral column as kyphoscoliosis.
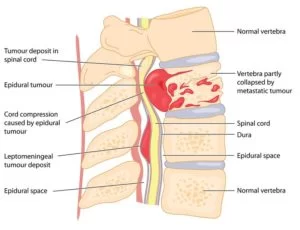
- 2. Meningeal (extramedullary):
- Extradural e.g. leukaemic deposits.
- Dural e.g. meningioma.
- Intradural e.g. neurofibroma.
- 3. Cord (intramedullary): Syringomyelia.
- B. Inflammatory:
- Transverse myelitis
- Myelomeningitis
- Myeloradiculitis.
- C. Vascular:
- Anterior spinal artery occlusion.
II. Systemic causes:
- Systemic disease in neurology is a disease that affects one or more systems selectively and is usually bilateral and symmetrical. When a systemic disease affects the pyramidal tracts, either alone or with other tracts, paraplegia will result.
- A. Heridofamilial:
- 1. Hereditary spastic paraplegia.
- 2. Hereditary ataxias e.g. Friedreich’s or Marie’s ataxia.
- B. Symptomatic:
- 1. Pellagral lateral sclerosis.
- 2. Subacute combined degeneration.
- C. Idiopathic: motor neuron disease.
III. Disseminated cause:
Disseminated Sclerosis (D.S.)
- Causes of Cerebral Paraplegia:
- A. Causes in the Parasagittal Region: (area of cortical presentation of L.L.)
- Traumatic e.g. depressed fracture of the vault of the skull, Subdural haematoma.
- Vascular e.g. superior sagittal sinus thrombosis.
- Inflammatory e.g. encephalitis, meningio-encephalitis.
- Neoplastic e.g. parasagittal meningioma.
- Degenerative e.g. cerebral palsy.
- B. Causes in the Brain Stem:
- Syringobulbia and midline tumors. These lesions arise in the midline and involve the innermost fibers which are those of the lower limbs.
Signs & Symptoms of Paraplegia:
- The patient experiences loss of movement or muscle control in the legs, feet, toes, or trunk.
- The patient experiences loss of sensation in the legs, feet, toes, or trunk.
- Tingling in the legs, feet, toes or trunk can also be felt.
- Bladder and bowel incontinence.
- Changes in sexual function, sexual sensitivity, and fertility.
- Exaggerated reflex activities or spasms.
- Pain or an intense stinging sensation caused by damage to the nerve fibers in your spinal cord.
- Difficulty breathing, coughing, or clearing secretions from your lungs.
Emergency signs and symptoms:
- Extreme back pain or pressure in your neck, head, or back.
- Weakness, incoordination, or paralysis in any part of your body.
- Numbness, tingling, or loss of sensation in your hands, fingers, feet, or toes.
- Loss of bladder or bowel control.
- Difficulty with balance and walking.
- Impaired breathing after injury.
- An oddly positioned or twisted neck or back.
Clinical Picture of Focal Paraplegia:
A. At the level of the lesion:
- 1. Vertebral manifestations:
- only present if the cause is vertebral.
- Localized pain or tenderness.
- Localized deformity or swelling.
- 2. Radicular manifestations:
- only present in extra-medullary causes.
- (a) Posterior root affection:
- Early pain in the back refers to the distribution of the affected root and is described as girdle pain; it is exaggerated by coughing, sneezing, and straining.
- Later, there is hypoesthesia or anesthesia in the dermatome supplied by the affected root.
- (b) Anterior root affection:
- Localized L.M.N. weakness in the muscles supplied by the affected root.
B. Below the level of the lesion: (cord manifestations):
- 1. Motor Manifestations:
- They depend on whether the cause of the lesion is acute or gradual.
- (a) If the cause is acute (inflammation, vascular, or traumatic), the paraplegia passes through 2 stages:
- Stage of flaccidity due to neuronal shock:
- Immediately following the lesion, there is sudden paralysis of the lower limbs, associated with complete loss of tone and absence of reflexes. This stage lasts from 2 to 6 weeks.
- Stage of spasticity due to recovery from the neuronal shock:
- On recovery from the shock stage, the full picture of U.M.N.L. will be established including hypertonia, hyperreflexia, positive Babinski sign & maybe clonus.
- (b) If the cause is gradual (e.g. neoplastic):
- The shock stage is absent and there will be a gradual progressive weakness of LL with hypertonia and hyperreflexia.
- The weakness affects the distal more than the proximal muscles and the flexor more than the extensors.
- Hypertonia and hyperreflexia affect the extensor group of muscles (antigravity) more than the flexor group (progravity). The paraplegia in this stage is described as (paraplegia in extension)
- With further progression of the lesion, the extrapyramidal fibers in the cord will be affected. The hypertonia and hyperreflexia will be more in the flexor group of muscles than in the extensors. In this stage, the paraplegia is described as (paraplegia in flexion).
- This last stage may be associated with the mass reflex where there is spontaneous urination, defecation, and sweating on scratching the skin over the medial side of the thigh.
- 2. Sensory of Manifestations:
- (a) If the cause of the lesion is extramedullary, encroachment on the ascending tracts at the site of the lesion results in a sensory level below which, all types of sensations are diminished. There is early loss of sensation in the saddle area (S 3, 4, 5), as the sacral fibres lie in the outermost part of the spinothalamic tracts in the cord.
- (b) If the cause of the lesion is intramedullary, there will be a jacket sensory loss (hyposthetic area with normal sensations above and below it).
- The sensory loss is of a dissociated nature i.e. pain and temperature sensations are lost but touch and deep sensations are preserved; this is due to the interruption of the crossing fibers carrying pain and temperature by the midline lesion, while touch and deep sensation fibers ascend in the posterior column without decussation.
- The sensations over the saddle area are preserved (sacral spare), as the sacral fibers lie far from the midline lesion.
- 3. Sphincteric Manifestations:
- (a) In acute lesions:
- There is the retention of urine in the shock stage, followed by precipitancy of micturition.
- (b) In gradual lesions:
- There is precipitancy of micturi¬tion which may terminate in the automatic bladder when a complete transaction of the cord occurs.
- These changes start late in extramedullary lesions and early in intramedullary lesions as the pyramidal fibres controlling the bladder center lie medially in the cord.
Diagnosis:

- Computerized CT scan for a better understanding of the severity of the injury.
- X-ray to examine any tumors or fractures in the spine.
- Magnetic Resonance Imaging(MRI) is to test for blood clots or any mass formation that may compress the spinal cord.
Treatment of Paraplegia:
I. General Management:
- Frequent changes in the patient’s posture to guard against bedsores.
- Care of the skin by frequent washing with alcohol followed by talc powder. In case of urinary incontinence, frequent change of bed-sheets.
- Care of the bladder: If there is retention, use parasympathomimetic drugs. If this fails, use a catheter to evacuate the bladder.
II. Physiotherapy Treatment:
A balanced exercise program includes three types of exercise:
(1) Stretching/Flexibility Exercises:
- slow, sustained lengthening of the muscle
- Stretching is the most important exercise you can do.
- Stretching improves flexibility – the ability to move the parts of your body through their full range of motion.
- Stretching also can reduce muscle spasticity and cramps and may also reduce problems such as tendonitis and bursitis.
- To be effective, stretching routines must be done regularly, usually once or twice a day.
- Stretch as far as you can hold the stretch for 10 seconds and then ease back.
- Each stretch should be performed slowly, with no sudden jerking or bouncing.
- Stretching also should be done before and after other exercises to prevent muscle strain and soreness and to help avoid injuries.
(2) Aerobic Exercises:
- Steady exercise using large muscle groups
- Aerobic exercise strengthens your heart and lungs and improves your body’s ability to use oxygen. It also reduces fatigue, increases energy levels, and helps you sleep better, control your weight, and lift your spirits.
- It is generally recommended to gradually work up to three or four sessions per week, each lasting 15 to 60 minutes. Include a 5-minute warm-up (including stretching) before the activity and 5 to 10 minutes of a cool down (stretching and slower activity) afterward.
- Walking, stationary bicycling, water exercises, and chair exercises are excellent choices.
- Walking: Experts recommend walking according to your ability, comfort, and safety. Even short, slow walks can provide benefits. Aquatic (water) exercises: Aquatic exercises and swimming provide optimal exercise conditions. Water eliminates the effects of gravity, allowing weakened limbs to attain a greater range of motion. Water also helps support the body so there is less stress on the hips, knees, and spine.
- Exercise in the water: This can help increase muscle power and endurance and help mobilize joints and muscles. They also help to relax muscles and improve coordination. Warm water (between 83 and 90 degrees F) can be especially good for stiff, sore joints. Exercises can be done while standing in shoulder-height water or while sitting in shallow water. In deeper water, an inflatable tube, floatation vest, or belt can be used for flotation.
- Stationary bicycling: Stationary bicycling is a great way to improve fitness without putting stress on hips, knees, and feet. It can be done in any weather, and balance is generally not an issue. Add resistance only as you are comfortable and only after warming up.
- Chair exercises: If mobility and balance are big issues, consider chair exercises. They can provide a great workout and easily incorporate strengthening and stretching exercises.
(3) Strengthening Exercises:
- Repeated muscle contractions until the muscle becomes tired.
- Strengthening exercises help increase muscle tone and improve the quality of muscles. This enhances mobility and provides energy and a positive sense of well-being.
- Strong hip and leg muscles are needed to lift the legs to walk, and strong arm muscles are needed to carry out daily functions. Strong abdominal and back muscles help maintain correct posture and can counter pain resulting from poor gait, poor posture, or the use of mobility aids.
Physical agents:
- Thermotherapy is used to decrease pain and spasticity. They are (i) Superficial heat: IR, wax bath, and (ii) Deep heat: SWD, MWD, etc.
- Electrical therapy: is used to increase muscle power and decrease pain. e.g., TENS, EST, IFT.

Therapeutic exercises:
- Mat exercise.
- PNF exercise.
- Active and passive ROM exercise.
- Strengthening exercise.
- Stretching exercise.
- Endurance exercise
- Co-ordination exercise.
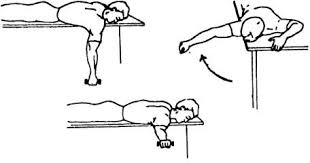
- Pelvic tilting exercise.
- Hamstring muscle stretching.
- Spinal rotation.
- Calf muscle stretching.
- Neck raising exercise
- Knee rolling exercise.
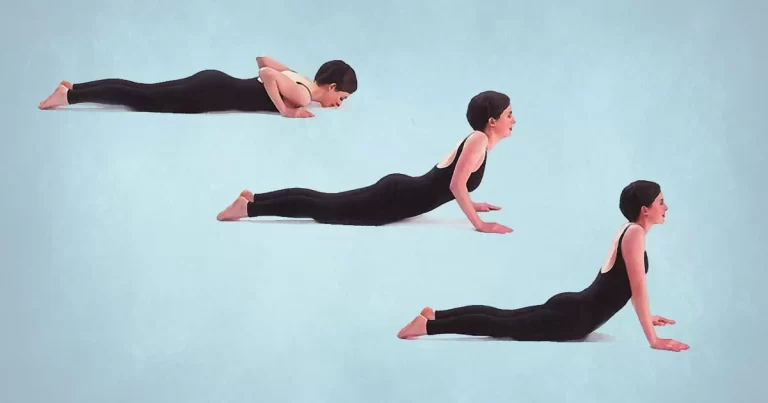
- Lying in extension.
- Extension exercise.
- Back and gluteal exercise.
III. Symptomatic Treatment:
- Analgesics and sedatives for pain.
- Muscle relaxants for the spasticity.
- Vitamins and tonics
IV. Orthosis:
- Various orthoses are used to assist patients with paraplegia.
- These are a crutch, walker, cane, lumbosacral brace, and wheelchair.
V. Gait training:
- It is an important part of the rehabilitation program balance can be achieved through proper gait training. Gait training can be done by following methods:
- Pre-ambulation MAT program:
- Rolling, prone on an elbow, prone on hand, quadruped, pelvic tilting, setting, and standing balance.
- Parallel bar progression
- Advanced parallel bar activities.
- Assistive device: E.g, Cane, crutches, walker
VI. Home program and Ergonomics:
- The patient is advised to use the lumbosacral orthosis to support the back during traveling.
- The patient is advised for hot fomentation at home.
- The patient is advised to lie in a prone position for at least 15 minutes duration twice a day.
- The patient is explained about proper sitting, standing, lying, and lying to standing, and doing household activities in a proper way.
- the patient is advised to rest and to avoid forward bending as much as the patient can avoid.




Thank you so much for this… Really very helpful.. I appreciate.. Thanks again..
Thank you for this topic
Thankyou so much,its really very helpful
Hey everyone,I’m from Pakistan,your work is very helpful.Keep it up.
Good one which is creating awareness and educative I will like to be posting any articles related to this thanks
Good article’s help full thank you.