Tibial Nerve Injury
What is a Tibial Nerve Injury?
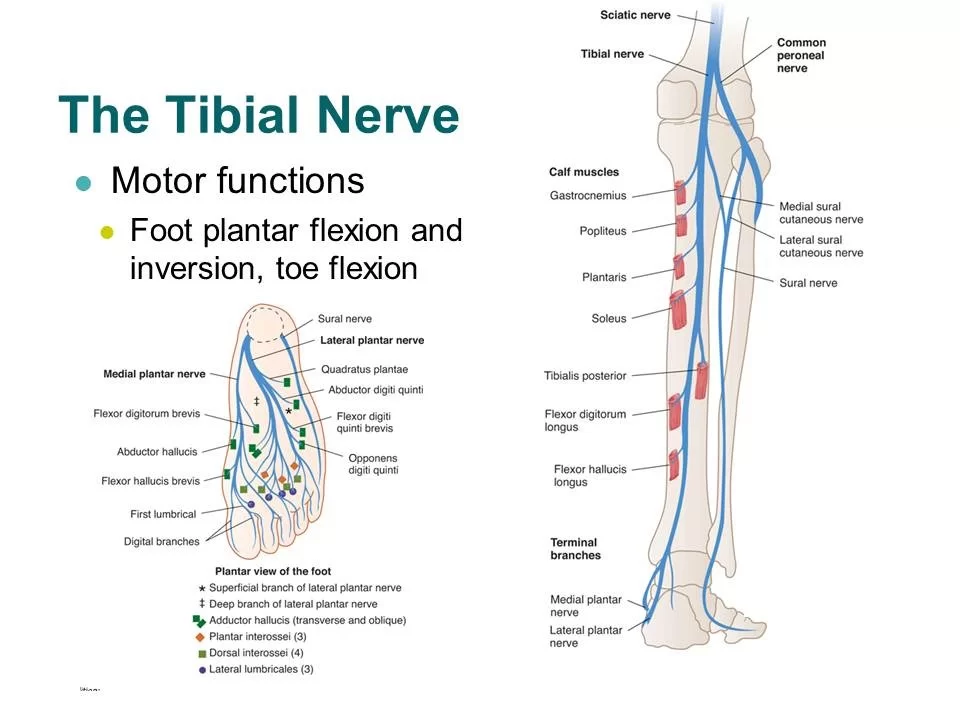
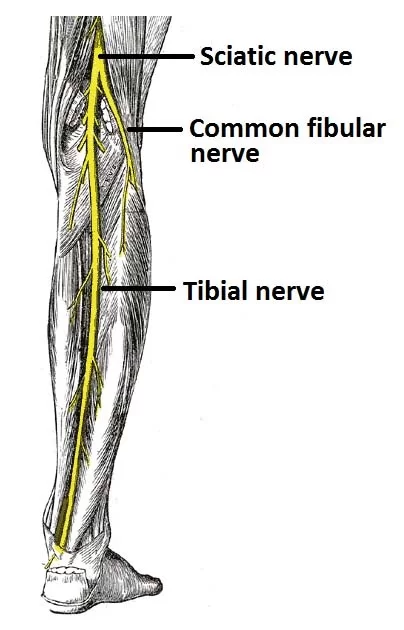
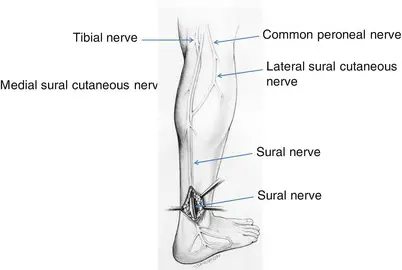
- The tibial nerve is derived from the L4-S3 nerve roots as part of the sciatica nerve.
- The tibial nerve runs through the popliteal fossa to pass below the arch of soleus.
- In the popliteal fossa the nerve gives off branches to gastrocnemius, popliteus, soleus, and plantaris muscles, an articular branch to the knee joint, and a cutaneous branch that will become the sural nerve.
- The sural nerve is joined by fibres from the common fibular nerve and runs down the calf to supply the lateral side of the foot.
- Below the soleus muscle, the nerve lies close to the tibia and supplies the tibialis posterior, the flexor digitorum longus, and the flexor hallucis longus.
- The nerve passes into the foot running posterior to the medial malleolus. Here it is bound down by the flexor retinaculum in company with the posterior tibial artery.
Courses of Tibial nerve:
- Branches from the sciatic nerve in the distal thigh and continues through the popliteal fossa entering the calf between the two heads of the gastrocnemius muscle.
- After passing deep to the soleus, it continues in the posterior compartment between the tibialis posterior and the soleus muscles.
- At the medial ankle, the nerve becomes superficial, before passing into the foot through the tarsal tunnel.
- Within the tunnel, it splits into the medial and lateral plantar nerves.
- The medial plantar nerve divides into muscular and cutaneous branches.
- The lateral plantar nerve passes between the quadrates plantae and flexor digitorum brevis.
BRANCHES:
- Direct branches:
- Motor innervations to the semimembranosus, semitendinosus, biceps femoris(long head), plantaris, popliteus, gastrocnemius, soleus, tibialisposterior, flexor hallucis longus, and flexor digitorum longus.
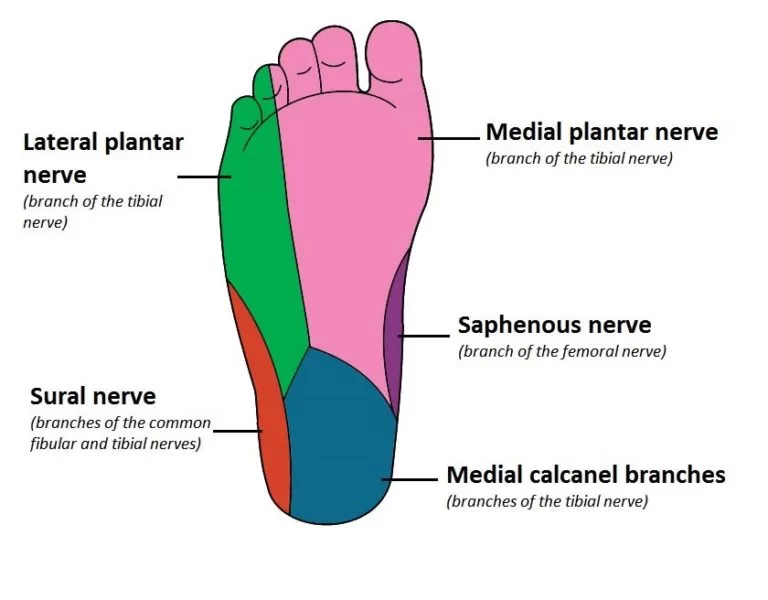
- Sensory innervations to posterolateral calf via sural branches.
- Medial plantar nerve:
- Motor innervations to the abductor hallucis, flexor digitorum brevis, flexor hallucis brevis, and first lumbrical.
- Sensory innervationto the medial sole and medial 3 ½toes.
- Lateral plantar nerve:
- Motor innervationto the quadrates plantae, flexor digiti minimi, adductor hallucis, interossei, abductor digitiminimi, and lateral three lumbricals.
- Sensory innervations to the lateral sole and lateral 1 ½toes.
- Medial Calcaneal Nerve:
- Sensory innervations to the plantar and medial heel.
Mechanism of Injury:
- Traumatic:
- Direct or indirect trauma (most commonly to the distal tibia or ankle), overuse.
- Compression:
- Mass lesion (e.g., varicosity, synovial thickening, ganglion cyst) or exostosis, accessory flexor digitorum longus, varicose veins, over-pronation, rear foot valgus deformity, muscular hypertrophy
- Systemic disorders:
- Rheumatoid arthritis, diabetes, etc.
Risk Factors:
- Walking and running.
- High-impact sports.
- Climbing stairs.
- Hiking.
- Obesity
- Diabetics.
- Individuals with hypertension.
Causes of Tibial Nerve Injury:
- Direct trauma.
- Pressure on the nerve for a long period of time.
- Pressure on the nerve from nearby body structures.
- The damage may destroy the myelin sheath that protects and insulates the nerve or part of the nerve cell (the axon). This damage reduces or prevents the movement of impulses through the nerve.
- The tibial nerve is often injured by pressure from a ligament on the inner part of the ankle. Injury or disease of structures near the knee may also damage the tibial nerve.
- The tibial nerve may also be affected by diseases that damage many nerves, such as diabetes.
Symptoms:
- Sensation changes in the bottom of the foot and toes, including burning sensation, numbness, tingling, or other abnormal sensation, or pain.
- Weakness of foot muscles.
- Weakness of the toes or ankle.
- Ankle that rolls inwards.
Possible Complications:
- Deformity of the foot (mild to severe).
- Movement loss in the toes (partial or complete).
- Repeated or unnoticed injury to the leg.
- Sensation loss in the toes or foot (partial or complete).
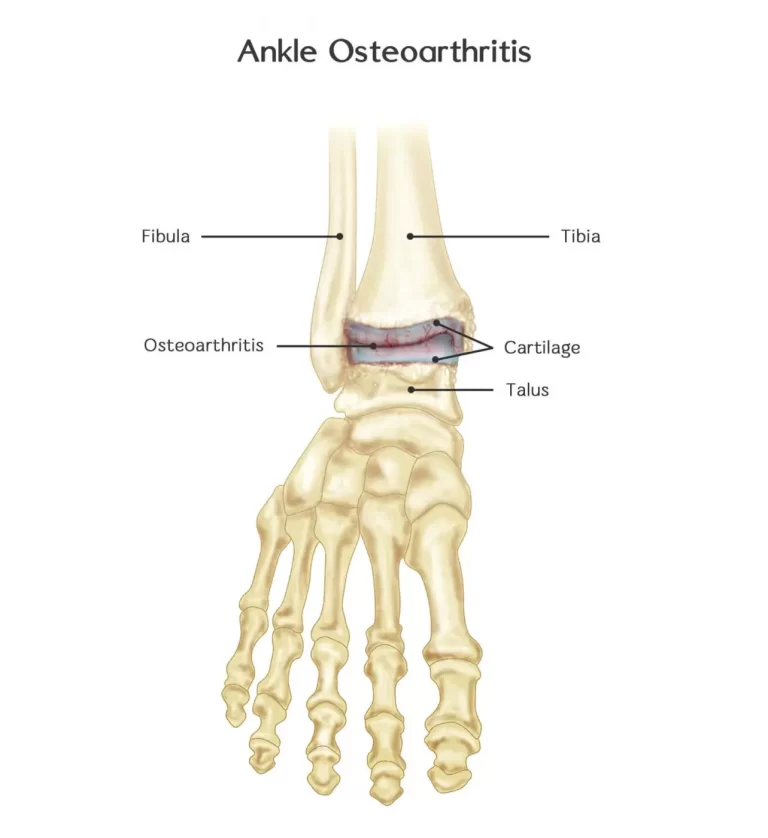
- Arthritis of the ankle or foot.
- Inability to walk due to pain.
- Muscle atrophy due to foot immobilization following treatment.
- Emotional stress can affect the quality of life.
TESTS AND EXAMS:
- Tests for tibial nerve dysfunction may include:
- EMG.
- Nerve biopsy.
- Nerve conduction tests ( NCV Test)
- Ultrasound.
- MRI.
- An examination of the legs will be done to diagnose tibial nerve dysfunction. The healthcare provider will also take a medical history.
- Signs include:
- Inability to curl the toes, push the foot down, or twist the ankle inward.
- Weakness.
- In severe cases, the foot muscles may become very weak and the foot may be deformed.
Treatments for Tibial nerve injury:
- The treatment of Tibial nerve injury is undertaken based on the severity of the condition and assessment of the signs and symptoms. The condition is often treatable without surgery.
- The following measures may be used in the treatment of Tibial nerve injury:
- Reduction of pain and swelling.
- Applying ice to the sore area.
- Taking non-steroidal anti-inflammatory medications.
- Resting; avoiding running or playing high-impact sports until the affected leg heels.
- Providing foot support.
- Ankle brace to support the damaged tendon around the ankle joint.
- Custom orthotics to improve one’s posture.
- Immobilization of the foot for 6-8 weeks may be recommended in some cases. However, this may lead to muscle atrophy.
- If Tibial nerve injury is severe and does not resolve using the above non-surgical treatment methods, then the following invasive surgical procedures may be necessary:
- Lengthening of the calf muscle.
- Removing damaged tendon areas.
- Replacing the posterior tibial tendon with another tendon.
- Cutting and moving bones (osteotomy).
- Joint fusion to correct flatfoot.
Physiotherapy Treatments:

- Range of motion exercises for hip flexion, extension, abduction, adduction
- Range of motion exercises for knee flexion and extension
- Range of motion exercise for ankle eversion.
- Range of motion exercises for ankle inversion.
- Range of motion exercise for ankle dorsiflexion, active assisted.
- Stretching of calf and hamstring muscle.
- Stretching of the gastrocnemius, soleus muscle.
- Strengthening exercises for hip and knee flexion and extension.
- Strengthening exercises for dorsiflexors, ankle eversion, and ankle inversion.
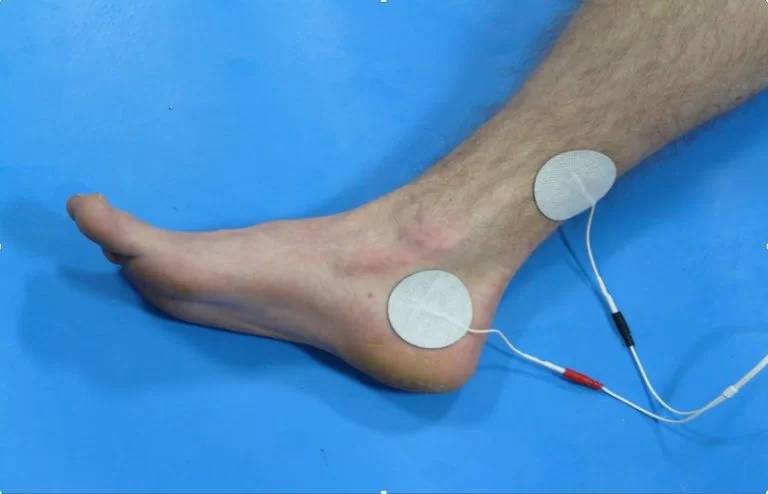
Modalities:
- Cold therapy.
- Electric stimulation.
- Ultrasound.
- Iontophoresis
Prevention:
- Reducing the risk of blunt force injury that can occur from falls or high-impact sports.
- Using protective sports gear while participating in high-impact sports.
- Excessively exercising without appropriate recovery may result in damage to the muscles, tendon, and nerves of the leg, particularly to the posterior tibial tendon. This can increase the risk of Tibial Nerve Dysfunction.
- Thus, limiting overuse and damage to the posterior tibial tendon during the following activities can help:
- Excessive walking and running.
- Climbing stairs.
- Long hikes without adequate rest.
- Your healthcare provider can recommend the correct amount and duration of exercises and the techniques for performing the same correctly.
Prognosis:
- The prognosis of Tibial Nerve Dysfunction when diagnosed and treated early is usually very good with a complete recovery expected in a majority of individuals.
- In some cases, there may be a partial or total loss of sensation and/or mobility in the foot.
- Nerve pain may cause discomfort and last for a long period of time.
FAQ
What are the symptoms of tibial nerve damage?
Some possible symptoms are as follows:
alterations in feeling, such as burning, tingling, numbness, or other unusual sensations, in the bottom of the foot and toes.
discomfort in the toes, sole of the foot, and around the ankle.
weakness and atrophy of the toe-moving muscles in the foot.
How do you test for tibial nerve?
Plantarflexion/Inversion Test:
This test involves putting the foot in its maximal plantarflexion and inversion position, holding it there for ten to fifteen seconds, and then bringing it back to neutral. If the patient experiences pain or paresthesia in the distal branches of the posterior tibial nerve, the test is deemed successful.
What does the tibial nerve control?
The lower leg can communicate with the brain thanks to the tibial nerve. It begins in the rear of the leg, above the knee. Your leg, foot, and toes can move because of the connections made by this nerve to 21 muscles.
How long does a tibial nerve take to heal?
After surgery, tibial neuropathy symptoms go away right away, however, some post-procedural pain may last for a few weeks. Complete nerve recovery may require a year or longer due to its gradual nature.





2 Comments